There is no agreement in defining osteoporosis in premenopausal women and diagnosis must be done carefully and not based on densitometric parameters. One must take into account the presence of other risk factors and history of fragility fractures, diseases or drugs that cause bone loss. Over 50% of premenopausal women with osteoporosis will have a secondary cause, with the remainder diagnosed with idiopathic osteoporosis. Therapeutic considerations are limited by a few studies in this group of patients, especially in regard to the risk of fractures. On the other hand, the FRAX index cannot be applied to premenopausal women. This article will review the measures to apply depending on the type of premenopausal osteoporosis, based on current scientific evidence.
No existe un acuerdo para definir la osteoporosis en mujeres premenopáusicas y el diagnóstico debe realizarse cuidadosamente y sin basarse únicamente en parámetros densitométricos. Hay que tener en cuenta la presencia de otros factores de riesgo como los antecedentes de fracturas por fragilidad, enfermedades o fármacos osteopenizantes. Más del 50% de las mujeres con osteoporosis premenopáusica van a presentar una causa secundaria, el resto serán diagnosticadas de osteoporosis idiopática. Las consideraciones terapéuticas están limitadas por los escasos estudios en este grupo de pacientes, sobre todo en lo que se refiere al riesgo de fracturas. Por otro lado, no disponemos del índice de FRAX, ya que no se puede aplicar a pacientes premenopáusicas. Este artículo pretende realizar una revisión sobre la actitud que se debe seguir según el tipo de osteoporosis premenopáusica basándonos en la evidencia científica actual.
Osteoporosis is defined as a bone disease characterized by decreased bone strength that predisposes fractures.1 In 1994 a committee of experts from the World Health Organization proposed the term densitometric osteoporosis, defining a category applicable to postmenopausal white women who had a bone mineral density (BMD) less than or equal to −2.5 standard deviations from a young population of same sex, that is, a T value less than −2.5.2
However, there is no agreement in defining osteoporosis in premenopausal women and the diagnosis must be done carefully so as to not rely solely on densitometry3 parameters. The International Society for Clinical Densitometry has suggested that these criteria should not apply to young women and has argued for the use of the Z value in this population group: a value of Z less than −2 at the lumbar spine or femur indicate a BMD value below normal for the age and sex of the individual. However, for a premenopausal osteoporosis diagnosis, it is recommended not relying solely on densitometric parameters and taking into account the presence of other risk factors and a history of fragility fractures and diseases or bone loss inducing drugs. This consideration is due to the fact that low BMD in a young individual can translate only a poor acquisition of peak bone mass and not related to an increased risk of fracture. On the other hand, the risk of fractures in postmenopausal women is higher than that of premenopausal women with the same BMD as premenopausal women have better estrogen stimulation, increased muscle mass, thicker bone cortex, less bone turnover and fewer falls.
What Is Its Impact?Postmenopausal osteoporosis is well documented and studied, but the pre-menopausal osteoporosis has been given less attention probably because of its low incidence. In fact, there are few studies on its actual incidence. The prevalence of osteoporosis by densitometry in younger women (20–44 years) of our population is 0.34%–0.17% in the lumbar spine and femoral neck, respectively.4 Studies examining the incidence of fractures in this group are limited; it is estimated that the incidence of vertebral fractures in younger patients (<35 years) is 3 per 100 000/year and rises to 21 in the population aged 35–44 years but often are due to trauma.5 Note that the presence of fractures in this group, with particular emphasis on those affecting the distal radius, is associated with decreased bone mass and also constitutes a risk factor for fractures in older adults.6
Moreover, as in any silent disease that causes symptoms in its early stages, it is probably an underdiagnosed disease. However, there are no studies on this in our environment.
What Determines Peak Bone Mass?Low BMD in premenopausal women is the result of the acquisition of a low peak bone mass, its subsequent loss, or both. Peak bone mass is genetically determined, but life habits, exercise and diet, and hormonal factors may contribute to this acquisition. At the end of the second decade of life, it is very similar in both sexes and lasts until age 40. Several factors were independently associated with increased bone mass, such as maintaining a BMI within the normal range at menarche, physical exercise involving mechanical loading during adolescence and normal pubertal development. It is estimated that the “peak” bone mass has a relatively greater influence on the development of osteoporosis in adulthood than the bone loss that occurs with age.7,8
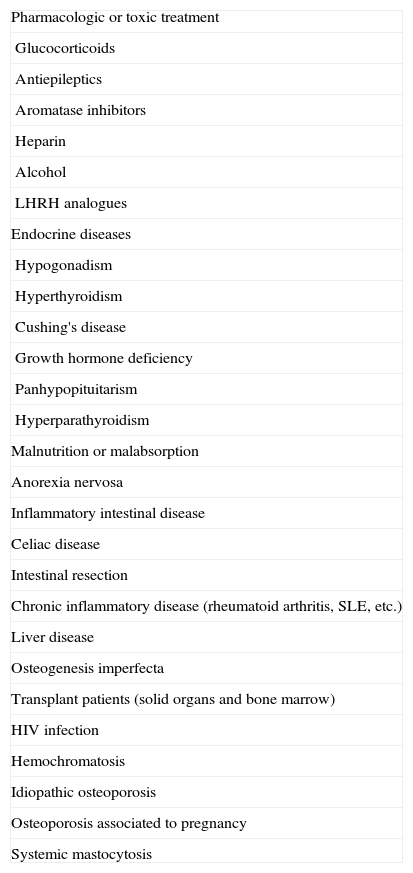
What Are the Causes of Premenopausal Osteoporosis?Over 50% of premenopausal women with osteoporosis will have a secondary cause; the rest will be diagnosed as idiopathic osteoporosis (Table 1). Epidemiological studies on the etiology of this disease are very rare. Peris et al. analyzed the causes of secondary osteoporosis in a single center in a total of 52 premenopausal women. Fifty-six percent had idiopathic osteoporosis. The most common secondary causes were found to be Cushing's disease, osteoporosis associated with pregnancy and osteogenesis imperfecta. In a previous study by the same research group in men, the most common causes were alcohol, hypogonadism and treatment with glucocorticoids. Another group in 1994, studied a population of 22 patients with osteoporosis, both young men and women, and described treatment with glucocorticoids as the most frequent cause of secondary osteoporosis and, in contrast, found that idiopathic osteoporosis was unusual.9
Causes of Secondary Osteoporosis in Premenopausal Women.
| Pharmacologic or toxic treatment |
| Glucocorticoids |
| Antiepileptics |
| Aromatase inhibitors |
| Heparin |
| Alcohol |
| LHRH analogues |
| Endocrine diseases |
| Hypogonadism |
| Hyperthyroidism |
| Cushing's disease |
| Growth hormone deficiency |
| Panhypopituitarism |
| Hyperparathyroidism |
| Malnutrition or malabsorption |
| Anorexia nervosa |
| Inflammatory intestinal disease |
| Celiac disease |
| Intestinal resection |
| Chronic inflammatory disease (rheumatoid arthritis, SLE, etc.) |
| Liver disease |
| Osteogenesis imperfecta |
| Transplant patients (solid organs and bone marrow) |
| HIV infection |
| Hemochromatosis |
| Idiopathic osteoporosis |
| Osteoporosis associated to pregnancy |
| Systemic mastocytosis |
Therefore, before reaching a diagnosis, the clinician should be thorough in finding an underlying cause. The first thing that must be performed is a thorough medical history, family history (50% of adult daughters of women with osteoporosis had low10 bone mass), a history of fractures, menarche, amenorrhea, pregnancy and lactation, diet and exercise, gastrointestinal symptoms, lifestyle and osteopenia associated medication. The use of drugs and concomitant diseases should be carefully questioned. Systemic physical examination should look for signs of underlying disease and laboratory tests are deemed necessary to rule out secondary causes of osteoporosis.11
The basic study includes: CBC, ESR, renal and liver function, electrolytes, calcium and phosphate in blood and urine, alkaline phosphatase, total serum protein and total proteins, lipid profile, ferritin, urinalysis, 24h urine calcium, 25-hydroxyvitamin D with estradiol and gonadotropins. Depending on the degree of clinical suspicion, parathyroid hormone, thyroid hormones, cortisol, prolactin or growth hormone should be requested. Clinical suspicion of celiac disease, mastocytosis or hypophosphatasia should expand testing. The determination of biochemical markers of bone turnover may provide additional information on bone remodeling in these patients and the therapeutic response. On rare occasions it may be necessary to perform a bone biopsy, especially to exclude osteomalacia.
What Is There to Treat Premenopausal Osteoporosis?Therapeutic considerations are limited by the few studies in this group of patients, especially in regard to the risk of fractures and treatment. On the other hand, we have no FRAX index because it cannot be employed in premenopausal patients. For premenopausal osteoporosis there are several recommended treatments:
- -
General measures (lifestyle adjustment). Exercise, a diet rich in calcium and vitamin D, calcium supplements and vitamin D in case of nutritional deficit, avoidance of smoking and alcohol, and maintaining a body mass index above underweight.
- -
Bisphosphonates. In studies with a limited number of patients, risedronate and alendronate orally and zoledronate and pamidronate intravenously have proven effective in preventing bone loss. It is important to note that bisphosphonates suffer bone accumulation, so excretion is maintained for years despite their suspension. This could determine a difficulty for the consolidation of fractures and a hypothetical teratogenicity. There are no systematic studies of bisphosphonate use during pregnancy, but animal studies suggest possible placental transfer and fetal skeletal development involvement. A systematic review of the literature studied 58 women treated with oral bisphosphonates in the period before conception or during pregnancy and did not detect any congenital abnormality.12,13 There are also some documented cases of patients treated intravenously with pamidronate14 who have had healthy children. The only data that indicate teratogenicity is described by the unit of clinical genetics and epidemiology at the University of Padua, which included 10 cases of women treated with bisphosphonates during pregnancy, resulting in 20% of congenital malformations.15 However, it is advisable to avoid conception while treated with the drug, but if it occurred inadvertently, interruption is not recommended.
- -
Hormone replacement therapy and anovulatory drugs. Applicable in patients with amenorrhea or early menopause. There are no consensus guidelines and employed less frequently, especially hormone replacement therapy.
- -
Teriparatide. It is not accepted as first-line therapy in premenopausal patients with idiopathic osteoporosis because there are insufficient safety and efficacy long-term studies in young patients. However, a study lasting 6 months in young women with premature menopause showed prevention of bone mass loss.16 Also, intermittent therapy with teriparatide has recently proven useful in the treatment of osteoporosis secondary to glucocorticoid treatment, being even superior to treatment with bisphosphonates in preventing vertebral fractures.17
- -
Calcitonin. It has not been shown to decrease the number of fractures in young women and it is not clear if it sufficiently improves BMD.18
- -
Low calcium (thiazides, amiloride, chlorthalidone and indapamide). In patients with hypercalciuria, to avoid a negative balance. It has shown an increase in BMD and a decrease in the risk of fractures.19
- -
Drugs contraindicated in this age group are selective modulators of estrogen receptors, which act by blocking estrogen action in bone and may cause increased bone loss; they should only be indicated in younger patients if they are menopausal. There are no studies of the effectiveness of strontium ranelate or denosumab in premenopausal women.
Women who have low BMD alone, without other risk factors should not be diagnosed with osteoporosis and not receive any treatment. They should undergo the same control as patients of any other age, with the same general recommendations.
In women who in addition to low BMD have risk factors, such as a fracture or secondary causes of osteoporosis, should undergo a therapeutic intervention. And treating the underlying cause always should be considered first. There are very few studies on drug treatment in this population, so we can divide the approach to be followed by the type of premenopausal osteoporosis:
- 1.
Idiopathic osteoporosis. Women with low bone mass and/or a pathological fracture, and in whom an underlying cause has not yet been found, should be diagnosed as idiopathic osteoporosis. This entity is rare, affects both sexes equally and its cause is not clear. Often these patients have a family history of osteoporosis, which confirms the relevance of genetic factors. A study showed that 50% of daughters of women with postmenopausal osteoporosis showed a decrease in bone mass. Between 36% and 50% of patients with idiopathic osteoporosis have associated hypercalciuria,19 quite often with kidney stones. Also other findings, described in isolation, are alterations in the dynamics of parathyroid hormone secretion, decrease in the values of growth hormone or serum estradiol, alterations in osteoblasts α-estrogen receptor expression or increased production of interleukin-1, which stimulates bone resorption and decreases bone formation associated with impaired osteoblast proliferative capacity.20
Regarding treatment, the few existing studies show that some of these women just need general measures to stabilize bone mass. In patients with hypercalciuria drugs that reduce calcium loss in urine and sodium restriction patterns in the diet may be added, as well as avoidance of a decreased calcium intake to avoid a negative balance. In young men with idiopathic osteoporosis, bisphosphonates and teriparatide have been effective, but there are little data on safety and efficacy of these treatments in young women with this disease, so the establishment of systematic guidelines is recommended.21
- 2.
Secondary osteoporosis. Each underlying disease has special considerations. In many cases, treating the underlying disease leads to an increase in BMD. Here are the most frequent findings:
- -
Treatment with glucocorticoids. Treatment with glucocorticoids is the most common drug related cause of osteoporosis. Glucocorticoids reduce the number and function of osteoblasts, and increased half-life of osteoclasts. Between 18% and 22% of young premenopausal women develop osteoporosis following prolonged and high doses of prednisone.22 The incidence is related to dose and duration of treatment.23 A recent Japanese study shows that high doses of glucocorticoids in premenopausal patients with connective tissue diseases are associated with a high prevalence of symptomatic vertebral fractures (11.3%) and increase with age, dose and duration of treatment, and alcohol consumption.24 There is limited experience in the treatment of glucocorticoid-induced osteoporosis in this group of patients. The American College of Rheumatology (ACR) recommended patients taking glucocorticoids for more than 3 months with a dose above 7.5mg daily and with a prior history of fracture, to be treated, in addition to general measures, with bisphosphonates (alendronate or risedronate as first options, or zoledronate depending on the case).25–27 However, the number of premenopausal women included in these studies is limited. Another option that has proven effective in a recent study is intermittent therapy with teriparatide, and is even superior to treatment with bisphosphonates in preventing vertebral fractures.17 It should be used if the risk of fracture is high or the response is not considered appropriate. However, the long-term use of the drug in premenopausal women and the number of young patients included in this study was limited.28 However, in patients treated with lower doses of corticosteroids or no history of fractures, the ACR concluded that currently there are not enough data to make specific recommendations, insisting only on general measures.
- -
Eating disorders and states of amenorrhea. These situations are associated with significant bone loss, especially when the onset occurs in adolescence. Multiple factors are implicated: malnutrition, deficit of calcium and vitamin D, estrogen deficiency, increased production of cortisol and secondary hyperparathyroidism.29 Treatment should include calcium and vitamin D. Other treatments such as hormone replacement therapy, oral contraceptives, or bisphosphonates (alendronate and risedronate) have been shown to increase BMD in some studies, but all agree that the most important determinant is weight gain.30 Therefore, pending further studies, these drugs should not be used in a routine manner.31
- -
Endocrine. Patients with primary hyperparathyroidism often have osteoporosis due to increased bone remodeling. A T score <−2.5 and an age of less than 50 years are among the indications for surgery. After surgery, most patients manifested present an improvement in BMD.32 Other examples of loss of bone due to increased remodeling are hyperthyroidism and Cushing's disease. This decline can be reversed with adequate treatment.33
- -
Gastrointestinal disorders and malabsorption. Calcium absorption is mediated by the active metabolite of vitamin D (1,25-hydroxyvitamin D), which is absorbed in the intestine. Vitamin D deficiency can lead to loss of bone density due to secondary hyperparathyroidism. Diseases such as celiac disease and pancreatic insufficiency, women who have undergone bariatric surgery or have inflammatory bowel disease should be considered at risk for premenopausal osteoporosis. Treatment can slow bone loss. In the case of inflammatory bowel diseases, the mechanism is multifactorial and includes the effect of inflammatory cytokines, malabsorption, and treatment for the disease, which is often steroid based.34 The exact risk of fractures is unknown at present. There is no consensus, but bisphosphonates can be considered a good therapeutic option in the future, although to date no sufficient scientific evidence for guidelines is systematic.35
- -
Transplantation of solid organs and bone marrow. After transplantation there is a loss of bone mass and an increase in the number of fractures. The reason for this, besides the underlying disease, is mainly immunosuppressive treatment. A study of mineral metabolism before transplantation and densitometry is therefore recommended. Treatment with vitamin D supplements, if required, as well as bisphosphonates has been shown to be useful to increase BMD. However, no studies on the reduction in the number of fractures exist to date.36,37
- -
Osteoporosis associated with pregnancy. It presents with insufficiency fractures, especially vertebral, during late pregnancy or postpartum. The etiology of this disease is not clear. After pregnancy an increased spontaneous and progressive bone mass, but not normalization may be seen. Administration of bisphosphonates for a short period has been associated with improvement in BMD, but no studies on reduction in the number of fractures are available. Further studies are needed to establish specific recommendations. In these patients breastfeeding is not recommended because it can contribute to further bone loss in this period.38,39
- -
Chronic inflammatory diseases (rheumatoid arthritis, lupus, etc.). Both osteopenia inducing drugs in these patients and the disease inflammatory activity contributes to osteoporosis, so the goal in this type of bone loss is the control of the underlying disease.40,41
- -
Other. In patients treated with antiepileptics or other osteopenia inducing drugs, guidelines consider supplemental calcium and vitamin D. In other pathologies, such as osteogenesis imperfecta or chemotherapy or hormone therapy for breast cancer, intravenous bisphosphonates have proven useful. However, this is not the objective of the current review.
- -
Monitoring should be performed in premenopausal women with osteoporosis until BMD remains stable, and should be monitored by performing densitometry every 18–36 months.33 Since there are no treatment guidelines, treatment should be individualized, using common sense and experience with the help of therapy, but few consensuses exist on secondary causes. We should mention, finally, the need for further studies in this area.
Fundamental Ideas- -
A low BMD in premenopausal women is not associated with the same risk of fractures as in postmenopausal women.
- -
The Z score should be used in young people to define BMD.
- -
A Z score <−2 is defined as “below the expected range for age”, not as pre-menopausal osteoporosis.
- -
Premenopausal osteoporosis diagnosis requires not only densitometry but the consideration of other risk factors.
- -
Over 50% of premenopausal osteoporosis are secondary.
- -
If no secondary cause is found, the diagnosis is “idiopathic osteoporosis.”
- -
All premenopausal women should receive basic recommendations on the prevention of osteoporosis.
- -
Secondary causes should be treated first.
- -
The use of other therapies is limited to situations with high risk of fracture or rapid loss of bone mass, as well as some secondary causes.
- -
More studies are needed to specify when to start treatment in premenopausal osteoporosis.
- -
There are no guides, so use common sense and experience, and individualize treatment.
Please, cite this article as: Martínez-Morillo M, et al. Osteoporosis premenopáusica: ¿cómo tratarla? Reumatol Clin. 2012;8(2):93–7.