Infectious diseases are a significant cause of morbidity and mortality in patients with connective tissue diseases. Corticosteroids and immunosuppressive drugs, such as cyclophosphamide (CYC), increase the risk of infections. The objective of this study was to estimate the incidence rates of severe infections in patients who received treatment with CYC.
Patients and methodsThe records of 60 patients with systemic autoimmune diseases who received treatment with CYC were retrospectively reviewed. We evaluated the rate of severe infections that occurred during CYC therapy and the 3 subsequent months.
ResultsSystemic lupus erythematosus was the most common disease, and diffuse proliferative glomerulonephritis the most frequent indication. Severe infection occurred in 9 patients (15%). Community acquired pneumonia was the most frequent infection with 3 cases (33%) followed by Herpes Zoster with 2 reports (22%). The cumulative dose of corticosteroid was the only significant risk factor for infection, 32.8±16.7 vs 20.1±15.3, P=0.007.
ConclusionThe use of lower doses of corticosteroids and an aggressive management of infectious complications allow for an acceptable safety profile in patients treated with CYC.
Las infecciones son una de las principales causas de morbimortalidad en los pacientes con enfermedades autoinmunes sistémicas. Los corticoides y los inmunosupresores como la ciclofosfamida (CF) son algunos de los factores que se asocian a esta complicación. El objetivo de este estudio fue determinar el porcentaje de pacientes que presentaron infecciones graves durante el tratamiento con CF y en los 3 meses posteriores.
Pacientes y métodosSe realizó un análisis retrospectivo de 60 pacientes con diferentes enfermedades autoinmunes que recibieron tratamiento con CF. Se valoró el porcentaje de infecciones graves.
ResultadosLa patología mñas común fue el lupus eritematoso sistémico y la indicación más común fue la glomerulonefritis proliferativa difusa. El 15% de los pacientes presentó un episodio infeccioso. Las infecciones más frecuentes fueron neumonía adquirida en la comunidad en 3 casos y herpes zóster en 2 casos. La dosis acumulada de corticoides fue el único parámetro que se asoció a infecciones 32,8±16,7 vs. 20,1±15,3 p=0,007.
ConclusiónUn seguimiento estricto, la utilización de corticoides en la menor dosis posible y el tratamiento enérgico de los procesos infecciosos permiten un perfil de seguridad aceptable en aquellos pacientes tratados con CF.
Systemic autoimmune diseases are a heterogeneous group of disorders in which immune system dysfunction plays a central role, and with infections a major cause of morbidity and mortality in these patients. Among the predisposing factors for this complication, genetic, immunological abnormalities, different organ systems affected, disease activity and drug use, among which are corticosteroids and immunosuppressants, such as cyclophosphamide (CF), stand out.1
CF is an alkylating agent with potent antiproliferative action on T and B lymphocytes, used in the most severe forms of rheumatic diseases, particularly systemic lupus erythematosus (SLE) and ANCA-associated vasculitis; it has contributed to improved survival in these patients. However, its use is associated with bone marrow suppression, bladder toxicity, increased risk of malignancies, infertility and infections.2
The objective of this study was to determine the percentage of patients with systemic autoimmune diseases, in treatment with CF, who had developed serious infections.
Severe infection was defined as an event caused by the herpes zoster or that which merited hospitalization and/or intravenous antibiotic therapy; it also considered its relationship with the type of rheumatic disease and the cumulative dose of CF and corticosteroids.
Materials and MethodsThe medical records of 60 patients with systemic autoimmune diseases seen at the Rheumatology and Systemic Autoimmune Diseases Section of the Hospital Iturraspe JB in Santa Fe, Argentina, who were treated with CF between November 1996 and March 2011, were retrospectively reviewed. Demographics of each patient, the reason for using CF, concomitant steroid use, cumulative dose of CF and corticosteroids, infection, need for hospitalization and/or antibiotics/antivirals were analyzed.
Statistical AnalysisAn observational, retrospective and cross-sectional analysis was performed. Position summary measures were calculated: mean and median, as well as dispersion measures such as standard deviation, ranges and their respective 95% confidence intervals (CI). Risks were estimated by odds ratio (OR) (the variables analyzed were gender, age, cumulative dose of steroids and CF) and the corresponding CI. The nonparametric Mann–Whitney test was used for comparison of means and Fisher's exact test for independence. A significance level of alpha=0.05 was adopted. SPSS 18.0 and Epi Info 20003 software packages were used for analysis.
ResultsThe study included 60 patients, 48 women and 12 men; mean age±standard deviation thereof was 42.83±14.12 years.
The most common pathology was SLE (n=37), followed by systemic vasculitis (n=8), systemic sclerosis (n=6), overlap syndromes (n=4), rheumatoid arthritis (n=2), relapsing polychondritis (n=1), cutaneous vasculitis (n=1) and retinal vasculitis (n=1).
The presence of diffuse proliferative glomerulonephritis (DPGN) in 28 cases was the main indication for the use of CF, which represented 47% of cases.
In total, 541 boluses were applied, the doses of each varying from 500mg to 1g.2 The cumulative dose of CF ranged from 1.0 to 166.5g, with a median of 7.3g. There were 5 patients who received 25g or more of CF, values considered statistically atypical for this sample, of which one (cumulative dose =102g) had an infectious process.
In the case of steroids, the median of the cumulative dose was 17.3g, with a range of 3.0–91.0g. In this case there were 4 patients with cumulative doses higher than 54.0g, one of which (cumulative dose 69.7g) presented infection.
It should be noted that patients with cumulative doses of CF considered atypical are not the same as those that had high cumulative doses of corticosteroids.
During follow-up, 2 patients with severe forms of granulomatosis with polyangiitis (Wegener's granulomatosis [WG]) received oral CF for a time.
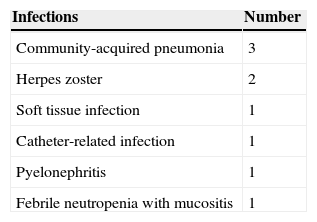
15% of patients (n=9) had at least one infectious episode during treatment with CF. The most frequent infections were community acquired pneumonia (CAP), 3 cases (33%) and herpes zoster, 2 cases (22%) (Table 1). A single case presented leucopenia with neutropenia at time of infection. None of the patients died as a result of the infectious process. The time from the start of treatment with CF and infectious symptoms ranged between 2 and 66 months.
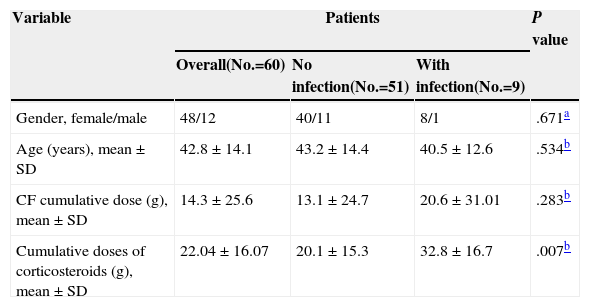
When comparing the group of patients who were infected with those who were not, no statistically significant differences regarding age (P=0.534), gender (P=0.675) and cumulative dose of CF were found at the time of infection (P=0.283) (Table 2).
Comparison of Doses Received Between Patients With and Without Infection.
| Variable | Patients | P value | ||
|---|---|---|---|---|
| Overall(No.=60) | No infection(No.=51) | With infection(No.=9) | ||
| Gender, female/male | 48/12 | 40/11 | 8/1 | .671a |
| Age (years), mean±SD | 42.8±14.1 | 43.2±14.4 | 40.5±12.6 | .534b |
| CF cumulative dose (g), mean±SD | 14.3±25.6 | 13.1±24.7 | 20.6±31.01 | .283b |
| Cumulative doses of corticosteroids (g), mean±SD | 22.04±16.07 | 20.1±15.3 | 32.8±16.7 | .007b |
Significant P-value <.05.
SD: standard deviation.
When analyzing the cumulative dose of steroids and comparing them between patients with and without infection, it was observed that all patients who developed infections had a cumulative dose between 15.0 and 69.6g, while those in which there was no infectious process, the dose ranged between 3.0 and 90.6g. Furthermore, in 50% of patients without infection the accumulated dose was 16.0g or less.
Cumulative corticosteroid doses in patients with and without infection were compared, finding significant differences (P=0.007).
A cutoff was established in the cumulative steroid doses of 20.0g, which coincided with the 75th percentile of the dose values of patients who were not infected .A statistically significant association between high levels of cumulative dose of steroids and infection (P=0.029) was found, which would indicate that patients with cumulative doses greater than or equal to 20.0g have almost 6 times more chance of infections (OR=5.89, 95% CI, 1.1–31.3) than those with smaller cumulative doses.
DiscussionThe introduction of CF in the rheumatology armamentarium has led to an increase in survival of 10% per year in untreated patients to 80% in severe conditions such as WG.4 Moreover, its use in patients with severe forms of SLE is associated both with an increase in survival and a decline in chronic renal failure in patients with renal compromise.5
The usually mild infectious processes are the most common complication of patients treated with CF. Martin et al. analyzed 451 boluses in 75 CF patients with different rheumatic diseases, finding 28% of infections, while only 9% of patients presented a serious infection.6
15% of our patients had a severe infection, the most common being community-acquired pneumonia. Other researchers have reported a lower rate of serious infections using a lower dose of CF.7,8 The second most common infection in our study was Herpes in 2 cases (22%), a percentage similar to reports by others.5
Reversible myelosuppression is common with the use of CF, and the degree of leuco/neutropenia and thus the risk of infection is related to the dose used. Also, prolonged use leads to greater sensitivity for bone marrow suppression.9,10 In our series, leuko/neutropenia was seen in one case and had no serious impact on the patient.
Increased susceptibility to infections is also one of the most common side effects of steroid use. This complication is related to the time of use, the doses and cumulative doses.11 Steroid use was the only statistically significant factor associated with infections in our patients.
None of our patients died as a result of infection, possibly due to early and intensive antibiotic treatment.
The main limitation of this study is its retrospective nature; however, it reflects daily clinical practice, where patients are very heterogeneous, as are the treatments instituted, as there were patients who had to be retreated with CF due to the severity of their affection and, in 2 cases, the need for oral therapy for a time.
While infections are one of the most feared adverse events in patients using CF, in our series there was 15% of serious infections, which did not cause the death of any patient related to the dose of corticosteroids received.
In conclusion, we believe that strict monitoring associated with the use of corticosteroids in the lowest possible dose and aggressive treatment of infectious processes allows for an acceptable safety profile in patients with severe autoimmune diseases who need to be treated with CF.
Ethical ResponsibilitiesProtection of human and animal subjectsThe authors declare this research did not perform experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflicts of InterestThe authors have no conflicts of interest to state.
Please cite this article as: Cavallasca JA, Costa CA, Maliandi MR, Contini LE, Fernandez de Carrera E, Musuruana JL. Infecciones severas en pacientes con enfermedades autoinmunes tratados con ciclofosfamida. Reumatol Clin. 2015;11:221–223.