Behçet's disease (BD) is a multisystem disorder. The main pathology in BD is vasculitis that involves arteries and veins of all calibers. Central nervous system involvement occurs in 5–10% of patients. Increased morbidity and mortality is rarely observed in children. The mean age at onset in pediatric BD is approximately 7 years. Neurologic involvement in BD is usually observed after 3–6 years. We report the case of a four-year-old Turkish boy with BD with sagittal sinus thrombosis treated with infliximab. The patient presented papilledema without neurologic signs. Although long-term efficacy evaluations are needed in this case, infliximab therapy may be a good option in childhood BD with refractory sinus thrombosis. This is the youngest case of BD with sagittal sinus thrombosis reported so far.
La enfermedad de Behçet's (EB) es una enfermedad multisistémica. La principal patología es la vasculitis que involucra tanto las arterias como las venas, de cualquier calibre. La afección del sistema nervioso central ocurre en 5–10% de los pacientes. En niños rara vez se ve un incremento en la morbilidad o mortalidad. La edad media de inicio en niños es aproximadamente 7 años. La afección neurológica en EB se observa tras 3 a 6 años de evolución. Reportamos el caso de un niño Turco de 4 años de edad con EB y trombosis del seno sagital tratado con infliximab. El paciente presenta papiledema sin datos neurológicos. Aunque la eficacia a largo plazo de su tratamiento no se evaluó en este caso, el infliximab pudiera ser una buena alternativa en niños con EB y trombosis del seno refractaria. Este es el caso más joven de trombosis del seno sagital reportado hasta la fecha.
Behçet's disease (BD) is a multisystemic vasculitis. Superficial or deep vein thrombosis is seen in approximately 30% of patients.1 Herein we report a four-year-old boy who had BD complicated with superior sagittal sinus and transverse sinus thrombosis. To the best of our knowledge, this is the youngest case reported. The patient showed a good response to infliximab administration for the treatment of refractory deep vein thrombosis.
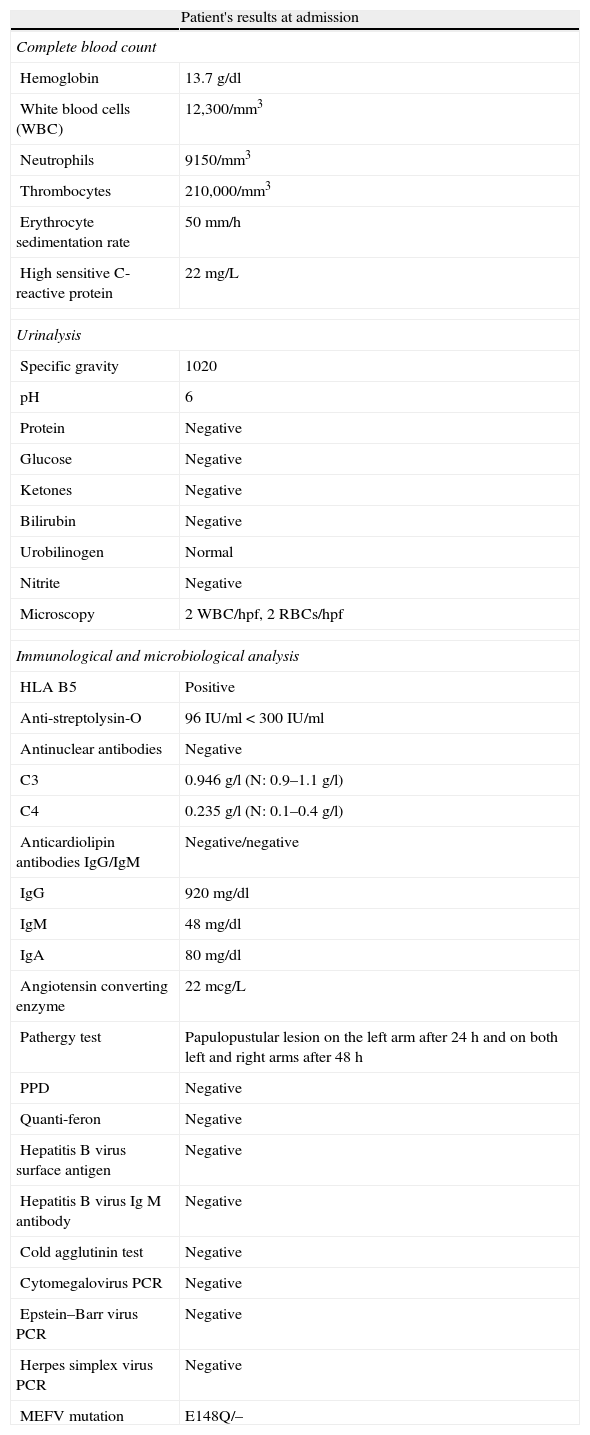
Clinical observationA four-year-old boy was admitted to the hospital due to recurrent oral aphthae and erythema nodosum. He had epididymitis in two occasions. The patient has nonconsanguineous healthy parents. Oral mucosa ulcerations and anal fissure were noticed in physical examination. The patient did not have uveitis. Pathergy test was positive. Laboratory test results are presented in Table 1. The patient was diagnosed with BD and treated with colchicine and prednisolone (1mg/kg/day).
Patient's laboratory examinations.
| Patient's results at admission | |
| Complete blood count | |
| Hemoglobin | 13.7g/dl |
| White blood cells (WBC) | 12,300/mm3 |
| Neutrophils | 9150/mm3 |
| Thrombocytes | 210,000/mm3 |
| Erythrocyte sedimentation rate | 50mm/h |
| High sensitive C-reactive protein | 22mg/L |
| Urinalysis | |
| Specific gravity | 1020 |
| pH | 6 |
| Protein | Negative |
| Glucose | Negative |
| Ketones | Negative |
| Bilirubin | Negative |
| Urobilinogen | Normal |
| Nitrite | Negative |
| Microscopy | 2 WBC/hpf, 2 RBCs/hpf |
| Immunological and microbiological analysis | |
| HLA B5 | Positive |
| Anti-streptolysin-O | 96IU/ml<300IU/ml |
| Antinuclear antibodies | Negative |
| C3 | 0.946g/l (N: 0.9–1.1g/l) |
| C4 | 0.235g/l (N: 0.1–0.4g/l) |
| Anticardiolipin antibodies IgG/IgM | Negative/negative |
| IgG | 920mg/dl |
| IgM | 48mg/dl |
| IgA | 80mg/dl |
| Angiotensin converting enzyme | 22mcg/L |
| Pathergy test | Papulopustular lesion on the left arm after 24h and on both left and right arms after 48h |
| PPD | Negative |
| Quanti-feron | Negative |
| Hepatitis B virus surface antigen | Negative |
| Hepatitis B virus Ig M antibody | Negative |
| Cold agglutinin test | Negative |
| Cytomegalovirus PCR | Negative |
| Epstein–Barr virus PCR | Negative |
| Herpes simplex virus PCR | Negative |
| MEFV mutation | E148Q/– |
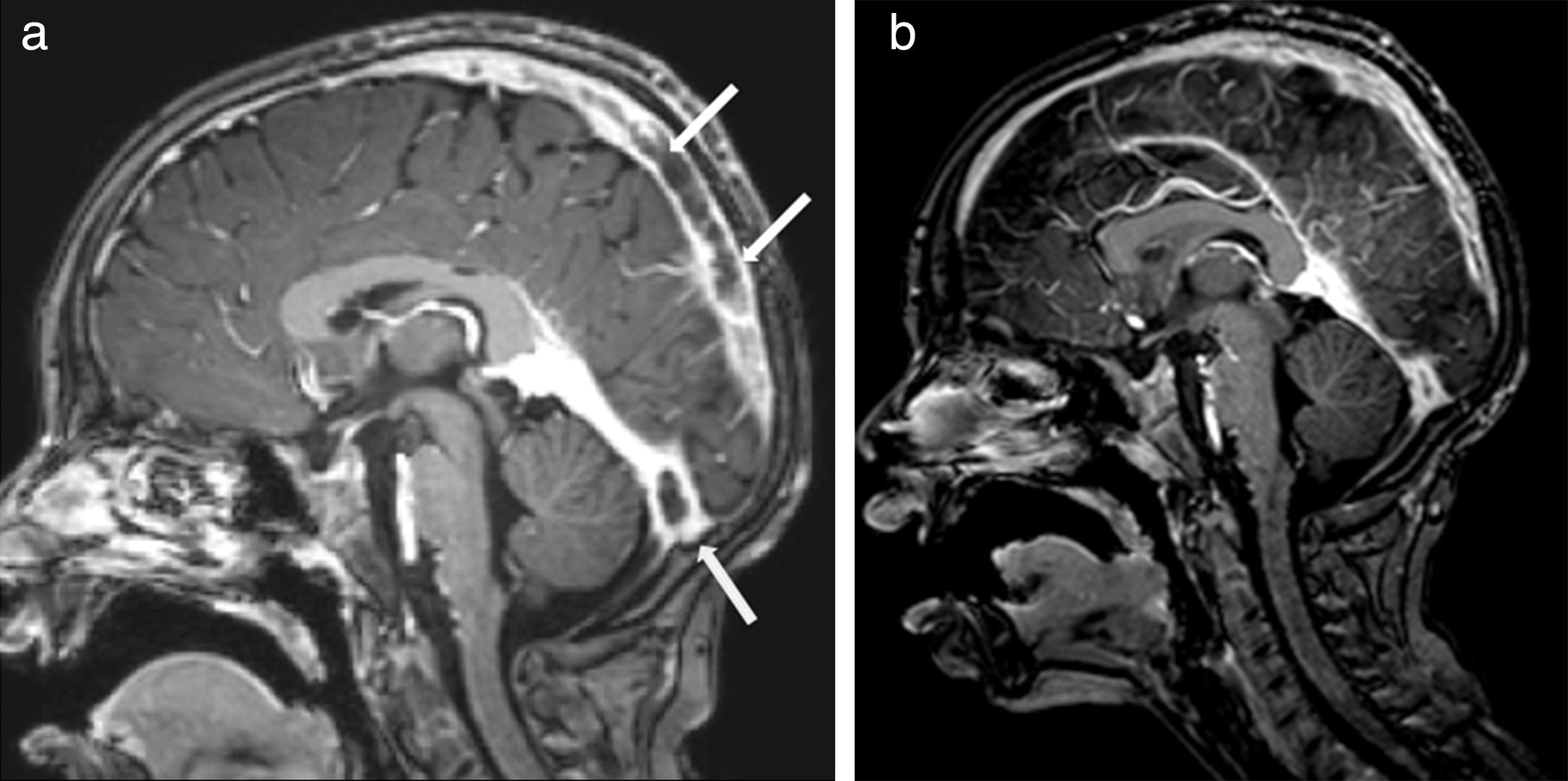
The patient had normal blood pressure; however, bilateral papilledema was detected. Magnetic resonance imaging (MRI) showed hyperintense thrombosis in the superior sagittal sinus and in both proximal segments of transverse sinuses (Fig. 1a). Subcutaneous low-molecular-weight heparin (LMWH) was started. The patient was investigated for a prothrombotic state and a methylenetetrahydrofolate reductase (MTHFR) heterozygous mutation was found. Azathioprine was added. One month later bilateral papilledema was detected again. The brain MRI was repeated and a new thrombosis distal to the superior sagittal sinus was detected. After permission from the ministry of health, infliximab was used at a 5mg/kg/day dose and 3 doses were applied on the 0, 2 and 6 weeks. Before the infliximab, azathioprine was stopped; prednisolone was tapered and stopped at the 7th day of infliximab. Ten days after first dose of infliximab, C-reactive protein was decreased to normal range, and both frequency and severity of the oral aphthous lesions were reduced. Resolution of the thrombosis was seen after the second dose of infliximab in the brain MRI (Fig. 1b). Ongoing therapies consist of colchicine and LMWH. Infliximab was well tolerated by this patient; no drug-induced side effects were recorded.
(a) Magnetic resonance imaging of brain before the infliximab. Hyperintense thrombosis filling the superior sagittal sinus and proximal segments of both transverse sinuses was showed and (b) after second dose of infliximab, significant dissolution of the thrombosis was observed in the brain MRI.
The mean age of onset in pediatric BD epidemiologic studies has been 7 years.2,3 The earliest age reported for thrombotic BD is 11-years.4 To the best of our knowledge, this is the youngest Behçet's patient who had cerebral thrombosis.
Vascular lesions in BD can involve both arterial and venous vessels, and cause refractory complications with poor prognosis. In our patient, cerebral thrombosis was refractory to treatment which corticosteroids, immunosuppressants, and anti-coagulants. The administration of infliximab resulted in the improvement of clinical and laboratory findings. In addition, cerebral sinus thrombosis in MRI was reduced.
The vascular involvement of BD develops in the active stage. Mononuclear cells infiltrate the vessel walls and damages them, and this may cause thrombosis.5 Infliximab may inhibit the activation of infiltrated mononuclear cells by blockade of TNF and TNF-producing cells, resulting in the prevention of thrombosis. Although long-term efficacy evaluations are still needed in this case, infliximab therapy may be a good option in childhood BD with refractory sinus thrombosis.
Since the International Study Group criteria are accepted for adult BD but not for pediatric BD, the delay in diagnosis of pediatric BD is unavoidable. Especially in the Silk Road countries, even in the absence of the cardinal findings of BD, pediatric patients with recurrent oral aphthous ulcers should be followed up for early detection and treatment of BD complications.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflict of interest statementNone.