PFAPA syndrome is an autoinflammatory disease whose diagnosis is mainly clinical. Several treatments have been proposed; among them, tonsillectomy could be an effective one.
Material and methodsRetrospective multicenter study. Patients included were diagnosed with PFAPA syndrome, according to the Thomas criteria, in 3 hospitals in Madrid between 2009 and 2013.
ResultsThirty-two cases were included. Median age at onset and at diagnosis were 32 months (IQR 24–44) and 47.5 months (IQR 37–60), respectively. There were increases in leukocytes (13,580/μl [IQR 8200–16,600] vs 8300/μl [IQR 7130–9650], p=.005), neutrophils (9340/μl [IQR 5900–11,620] vs 3660/μl [IQR 2950–4580], p=.002) and C-reactive protein (11.0mg/dl [IQR 6.6–12.7] vs 0.2mg/dl [IQR 0.1–0.6], p=.003) during febrile episodes. In all, 80.8% of patients reported remission of symptoms within 24h after oral corticosteroid therapy. Fourteen patients were tonsillectomised. In 11, the febrile episodes stopped while, in 3, the frequency was reduced; there were 2 cases of postoperative bleeding. The disease was resolved in 56.3% of the patients, at a median age of 60 months (IQR 47–95), with similar duration in patients who were tonsillectomised and those who were not.
ConclusionsWe present a large cohort of children with PFAPA syndrome, with clinical and analytical features similar to those described in the literature, and a good response to corticosteroids and a high resolution rate of symptoms after tonsillectomy.
El síndrome PFAPA es una enfermedad autoinflamatoria de diagnóstico clínico. Se han propuesto diversos tratamientos; entre ellos, la tonsilectomía podría ser un tratamiento efectivo.
Material y métodosEstudio multicéntrico retrospectivo. Se incluyeron pacientes diagnosticados de síndrome PFAPA, según los criterios de Thomas, en 3 hospitales madrileños, entre 2009-2013.
ResultadosSe incluyeron 32 casos. Las medianas de edad de inicio del cuadro y al diagnóstico fueron 32 meses (RIQ 24-44) y 47,5 meses (RIQ 37-60), respectivamente. Se hallaron incrementos en las cifras de leucocitos (13.580/μl [RIQ 8.200-16.600] vs 8.300/μl [RIQ 7.130-9.650], p=0,005), neutrófilos (9.340/μl [RIQ 5.900-11.620] vs 3.660/μl [RIQ 2.950-4.580], p=0,002) y proteína C reactiva (11,0mg/dl [RIQ 6,6-12,7] vs 0,2mg/dl [RIQ 0,1-0,6], p=0,003) durante los episodios febriles, respecto a los periodos libres de síntomas. El 80,8% refería remisión de los síntomas en 24h tras corticoterapia oral. Fueron tonsilectomizados 14 pacientes. En 11 cesaron los episodios febriles, mientras que en 3 se redujo su frecuencia; hubo 2 sangrados posquirúrgicos como complicación. El cuadro se había resuelto en el 56,3% de los pacientes, a una mediana de edad de 60 meses (RIQ 47-95), con una duración similar entre los pacientes que fueron tonsilectomizados y los que no.
ConclusionesSe presenta una cohorte amplia de niños con síndrome de PFAPA en la que se confirma que, en nuestro medio, los niños con este síndrome presentan unas características clínicas y analíticas similares a las descritas en la literatura, con buena respuesta a corticoterapia y elevada resolución de la clínica tras la amigdalectomía.
PFAPA syndrome or periodic fever with aphthous stomatitis, pharyngitis and adenitis, was first described by Marshall in 1987,1 and 2 years later received this acronym as its name.2 It is a periodic febrile syndrome of unknown aetiology, related to the group of autoinflammatory diseases, and consists of recurrent febrile episodes associated with at least one of the following symptoms: pharyngitis, aphthous stomatitis afthosa or cervical adenitis. Age of presentation is early, usually before school age and tends to resolve itself over the years,3 although long-term evolution has not been much studied.
The real rate of PFAPA syndrome is unknown, since few population data have been published, but it is considered the most frequent of diseases with periodic fever and it is believed that probably all paediatricians will come across at least one case over the length of their career.4 In this context, apart from describing its clinical findings, attempts have been made to describe the analytical pattern of the patients with this disease during febrile episodes so as to facilitate diagnosis, which is currently essentially clinical.
Since its description 30 years ago, several treatments have been empirically studied due to its possible autoinflammatory aetiology. Corticosteroids are the most popular treatment during acute episodes, and tonsillectomy could be an effective treatment according to some studies.5
The aim of this paper was to describe the epidemiological and clinical characteristics of a cohort of children diagnosed with PFAPA syndrome in our environment, analysing the analytical pattern presented during febrile episodes and assessing the role of tonsillectomy in treatment.
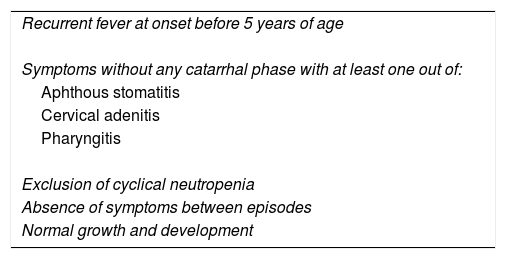
Material and MethodsA retrospective, multicentre cohort study. It included patients diagnosed with PFAPA syndrome, according to Thomas,6 criteria (Table 1), whose diagnosis and/or follow-up was undertaken between 2009 and 2013 in 3 hospital centres of the Community of Madrid: the General University Hospital Gregorio Marañón, the University Hospital 12 de Octubre and the University Hospital Severo Ochoa. Cases with suspected hereditary periodic fever syndrome or a specific immunodeficiency, albeit not confirmed, were excluded, as were those patients with pharynx, blood and/or urine cultures in which positive isolation was obtained in the majority of febrile episodes, since these episodes could be related to recurrent infections.
Thomas’ Diagnostic Criteria for PFAPA Syndrome.
| Recurrent fever at onset before 5 years of age |
| Symptoms without any catarrhal phase with at least one out of: |
| Aphthous stomatitis |
| Cervical adenitis |
| Pharyngitis |
| Exclusion of cyclical neutropenia |
| Absence of symptoms between episodes |
| Normal growth and development |
The epidemiological and clinical characteristics were collected in all cases, including gender, ethnicity and geographical origin, age at the beginning of symptoms, age at diagnosis, duration and periodicity of febrile episodes and the presence of pharyngitis, adenitis, canker sores and/or other associated symptoms during the episode.
Additional tests performed were recorded, both those during febrile episodes and those during symptom-free periods, in cases where they were available. The analytical data assessed were haemoglobin, platelet, leucocyte, neutrophil, lymphocyte, monocyte, eosinophil, reactive C protein (RCP) and erythrocyte sedimentation rates.
Regarding the therapeutic interventions involved, the analysed variables were the age of symptom resolution, the response to corticosteroids in at least 24h in the majority of episodes, the periodicity of the episodes after corticosteroid administration and the performing of tonsillectomy. In the case of tonsillectomy, age at surgery was also collected, as was the time of posterior follow-up, the appearance of new episodes and their frequency and the side effects attributed to them.
In all patients clinical evolution during a minimum of 18 months was assessed.
Analysis of data was undertaken with the SPSS 15.0 statistical programme, using descriptive analysis of frequencies and the Student's T-test for comparison of quantitative variables means with normal distribution, the Mann–Whitney U test for quantitative variables with non normal distribution, and the Chi-Square test for qualitative variables. A p value below .05 was considered significant throughout analysis.
ResultsA total of 32 children diagnosed with PFAPA syndrome were included, of whom 21 were female (65.6%). The majority were Caucasian (87.5%), one (9.5%) was from Latin American and one was of gypsy ethnicity.
Median age at onset of symptoms was 32 months (interquartile range [IQR] 24–44 months), whilst diagnosis was at 47.5 months (IQR 37–60 months). The median time which elapsed since the onset of medical symptoms until diagnosis of PFAPA syndrome was 12 months (IQR 6–25 months).
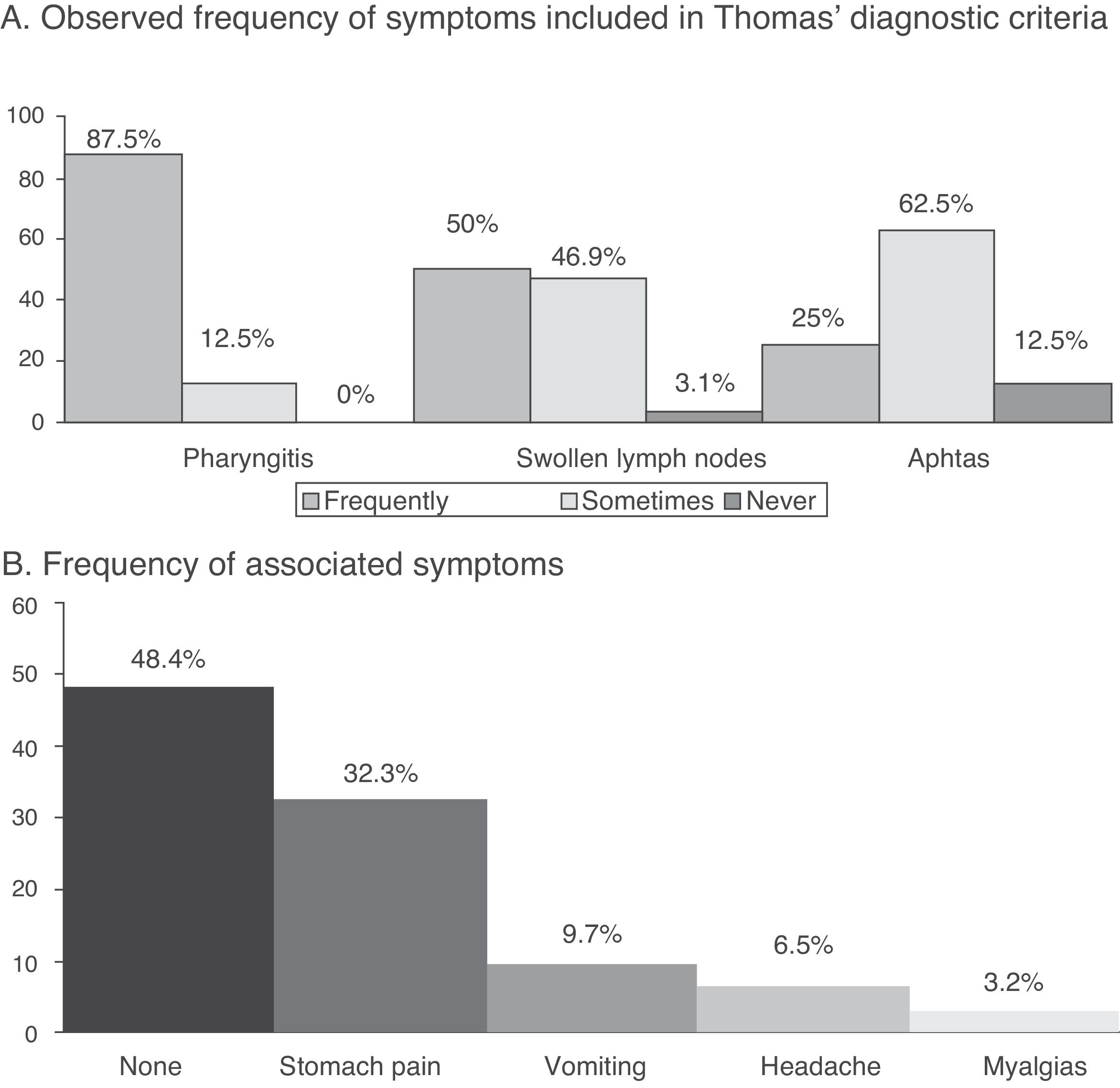
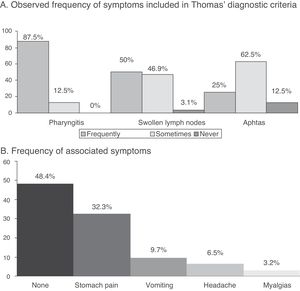
The median periodicity of episode occurrences was 4 weeks (IQR 3–5 weeks), whilst the duration of fever in acute episodes was 4.5 days (IQR 4–5 days). The most frequently referred to symptom during these was acute pharyngitis, followed by cervical adenopathies (Fig. 1A). In 51.6% of cases the patients referred to other symptoms (associated with P, with the most common being abdominal pain (Fig. 1B).
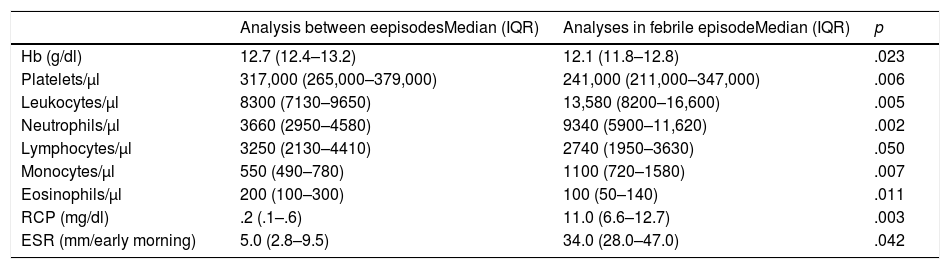
In 28 cases (87.5%) analysis was available during the inter-episode period, and in 19 of these, at least another was performed during a febrile episode attributed to PFAPA syndrome. Findings from these analyses are reflected in Table 2. The statistically significant differences stand out in the rate of leukocytes, neutrophils and RCP between the acute phase and the inter-episode period.
Comparison of Analytical Values of Children With PFAPA Syndrome at the Time of Acute Episode and Inter-episode Period.
| Analysis between eepisodesMedian (IQR) | Analyses in febrile episodeMedian (IQR) | p | |
|---|---|---|---|
| Hb (g/dl) | 12.7 (12.4–13.2) | 12.1 (11.8–12.8) | .023 |
| Platelets/μl | 317,000 (265,000–379,000) | 241,000 (211,000–347,000) | .006 |
| Leukocytes/μl | 8300 (7130–9650) | 13,580 (8200–16,600) | .005 |
| Neutrophils/μl | 3660 (2950–4580) | 9340 (5900–11,620) | .002 |
| Lymphocytes/μl | 3250 (2130–4410) | 2740 (1950–3630) | .050 |
| Monocytes/μl | 550 (490–780) | 1100 (720–1580) | .007 |
| Eosinophils/μl | 200 (100–300) | 100 (50–140) | .011 |
| RCP (mg/dl) | .2 (.1–.6) | 11.0 (6.6–12.7) | .003 |
| ESR (mm/early morning) | 5.0 (2.8–9.5) | 34.0 (28.0–47.0) | .042 |
With regard to treatment, all cases received oral corticosteroids in the acute episodes after diagnosis. In 80.8% of cases the fever disappeared in under 24h after administration.
43.8% (14) of cases included underwent tonsillectomy, with a median age of 54.5 months (IQR 46.3–72.5 months). Median evolution prior to the surgical procedure was 24.5 months (IQR 13.5–35.8 months). In 11 of them (78.6%) symptoms were completely resolved after tonsillectomy and no new episodes presented, whilst in the 3 remaining patients there was a reduction in the frequency of the febrile episodes. Median follow-up after tonsillectomy was 8 months (IQR 6.5–25.5 months). In 2 cases adverse events from surgery were recorded. Both were postsurgical bleeding of relevance which required hospital admittance, but no blood transfusions.
Of the 32 patients included in the study 56.3% had resolved the symptoms at the time of study, with a median age of 60 months (IQR 47–95 months). The median evolution time up to resolution was 25 months (IQR 16.8–33.5 months). The percentage of patients whose symptoms had been resolved were higher in those who underwent tonsillectomy (78.6% vs 38.9%, p=.025), although there were no statistically significant differences during the resolution time between the patients who underwent tonsillectomy and those who did not (37.7 months [95% CI 16.5–59] vs 24.4 months [95% CI 14.1–34.8 months], p=.683). No statistically significant differences were found between the epidemiological characteristics, age at diagnosis, age at resolution or episode characteristics between both groups.
DiscussionMost patients from this series were female, had begun attending the clinic in their third year of life and were diagnosed after approximately 12-month duration of their condition. The clinical characteristics of the cohort of this study did not differ from other previously published series. The febrile episodes occurred every 3–5 weeks, and during them a rise in leukocytes, neutrophils, RCP and erythrocyte sedimentation rates took place, with no association of acute bacterial symptoms. Tonsillectomy was performed on 14 of the patients, with resolution of their symptoms in 11 cases. Notwithstanding, no statistically significant differences were found in the resolution time between the groups whether or not tonsillectomy was performed although it was more prolonged in the children who had surgery, probably because those cases where symptoms resolved spontaneously with a shorter evolution time were less frequently candidates for surgery.
Recurrent fever is a frequent finding in paediatrics, and its causes vary, with the most common being recurrent self-limiting viral processes. However, there is a group of illnesses which may cause fever from time to time, among which are auto inflammatory diseases.7 Auto inflammatory diseases are included within the framework of primary immunodeficiences,8 as conditions which occur from deregulation of the immune system.9 The PFAPA syndrome is the most common of these,7 but its real rate and pathogenesis are unknown. One Norwegian study published in 2013 estimated an incidence of 2.3 cases per 100,000 children under 5 years of age.10 Small series of cases have been published in Spain,11 the broadest of which, as far as we know, is the one presented herewith.
Diagnosis of PFAPA syndrome was made based on Thomas’ criteria published in 1999,6 and modified from those of Marshall of 1989,2 which are currently those accepted by the Spanish Society of Paediatric Infectious Diseases.7 Since this is a clinical diagnostic entity, they are not the only previously proposed criteria,12 and probably the main source of conflict would be age at the beginning of symptoms which is usually earlier than 5 years of age. Data collected in this study therefore refers to patients whose symptoms began before they were 5, although some series have described cases where clinical symptoms began later.13–15
The age of presentation of this cohort was similar to that of previously published studies, with a median age of between 11 months and 3 and a half years16–21; the same is true of age at diagnosis which is situated between 3 and 8 years.17,18,20,21 Median time elapsed from the onset of symptoms to diagnosis, which in our cohort was 12 months, were slightly higher in 2 publications than our data: 217 and 3.2 years,18 respectively. Greater familiarity with the disease and its higher rate in recent years has led to a shorter delay in diagnosing patients.
Previously published studies present a periodicity of the episodes and a duration of fever in each episode similar to those of this series, oscillating in the majority of cases between 2 and 8 weeks, and 4 days, respectively.10,16–21 In most published cohort studies, the frequency of main symptoms is similar to that found in our study, with a predominance of pharyngitis (between 75% and 100% of cases), followed by cervical adenopathies (between 62% and 90% of cases) and canker sores (between 38% and 76%).16,17,19,21 The patients of this study presented with other symptoms not included in Thomas’ diagnostic criteria, which were mainly gastrointestinal, including stomach pain and nausea, headache and arthralgias, as similarly described by other authors.16,17,19,21
In this series we observed a very slight reduction of haemoglobin during the febrile episodes, which was statistically significant but not clinically relevant. Similarly, an absence in the number of platelet increase was observed. These findings are consistent with previously published data.3,4 The raising of leucocyte, neutrophil and monocyte levels, as well as the reduction in absolute figures of lymphocytes in our cohort, has also been described in previous publications although on many occasions these changes are moderate and may remain within normal ranges.4,22 The raising of RCP during febrile episodes is usually more marked,4,21,23,24 just as is reflected in this series, whilst procalcitonin usually remains unaltered,24 although this parameter was not sufficiently assessed in our study to be able to draw any conclusions in this regard.
Initial recommended treatment in patients affected by PFAPA syndrome is the administration of oral corticosteroids during the acute episodes, in a single dose of 1mg/kg of prednisone or its equivalent.5,7 80.8% of the patients in this series stated their symptoms had ceased after administration of the treatment in the majority of episodes. In previous publications, the percentage of patients who responded after a single dose of oral corticosteroids were between 63%21 and 84%.25 There are indication of a possible shortening of symptom-free episodes after administration16 in some patients. The appearance of changes in periodicity of episodes could not be accurately assessed after the administration of corticosteroids, since this was not stated in the majority of records.
Among alternative treatments, tonsillectomy has been the most highly studied. Out of the 14 patients of this cohort who underwent tonsillectomy, all experienced improvement of clinical symptoms, with resolution or reduction of frequency of febrile episodes in the remainder. A review of the Cochrane Library published in 2014,26 based on 2 minor clinical trials where the symptoms were resolved in 6327 and 10028 of the patients who underwent surgery, respectively, concluded that tonsillectomy was an effective treatment but the quality of the evidence is moderate. In the observational studies published, the efficacy of tonsillectomy was between 50% and 100%.10,16,20,25,29,30 In this series, at the time of assessment, the symptoms had been resolved in 56.3% of cases and although the rate of resolution was higher in patients who had undergone tonsillectomy, there were no differences in time of evolution between those who had undergone tonsillectomies and those who had not. In fact, the resolution time in this series was higher in the children who had undergone tonsillectomy which could indicate that those whose symptoms took longer to resolve were referred to surgery. Furthermore, there is the factor of family anxiety towards recurring febrile episodes, which could impact the decision for surgery, but this factor is rarely assessed in studies, although often present.
The main limitation of this work is its retrospective character, which impedes optimum assessment of the characteristics of the patient episodes due to loss of inherent information, and the possible bias of selection and information. Also, the number of patients, given the low rate of disease, impedes the creation of inferences. Another limitation is the variability in diagnosis of the PFAPA syndrome, due to the existence of many different published diagnostic criteria. We have tried to minimise this by establishing the Thomas criteria as inclusion criteria. Lastly, no viral studies were undertaken during the acute episodes, which could have facilitated an accurate differential diagnosis with recurrent infectious processes. However, it is a broad cohort compared with other published studies in our environment, and the selection criteria was intended to be as strict as possible.
To conclude, a broad cohort of children with PFAPA syndrome was obtained in multicentre collaboration where it was confirmed that, in our environment, the children with this syndrome present several clinical and analytical characteristics similar to those described in the literature, with good response to corticosteroids. Knowledge of the analytical pattern in the febrile periods, where often leukocytosis, neutrophilia and a rise in RCP takes place, is essential to prevent unnecessary antibiotic treatments. Regarding tonsillectomy, this seems to be an effective treatment, which is suggested for those patients with a more torpid evolution. However, it is not exempt from side effects, which would have to be taken into account due to the self-limiting nature of the process. Each case should probably be individualised and this process considered as a therapeutic alternative. To determine the efficacy of surgical treatment it would be pertinent to carry out a random, but complex study, due to the low incidence of the disease.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ibáñez Alcalde MM, Caldevilla Asenjo L, Calvo Rey C, García-Mon Marañés F, Blázquez Gamero D, Saavedra Lozano J, et al. Características y evolución de una cohorte de niños con síndrome PFAPA en la Comunidad de Madrid. Reumatol Clin. 2019;15:355–359.
This paper was presented as scientific communication at the 7th Congress of the Spanish Society of Paediatric Infectious Diseases, which took place in Santiago de Compostela from 6th to 8th March 2014.