Granulomatosis with polyangiitis (GPA) is a type of vasculitis associated with neutrophil anti-cytoplasm antibodies (ANCA) which may affect small and medium calibre vessels.1 It is characterised by granulomatose lesions and/or necrosing vasculitis in the upper and/or lower respiratory tract, glomerulonephritis and, less often, mucocutaneous, orbital and neurological involvement, among others.1 Pre- or paravertebral pseudotumour lesions are rare, and there are few reports of them in GPA.2,3 A case is presented of paravertebral pseudotumour as an incidental finding in the context of systemic GPA involvement.
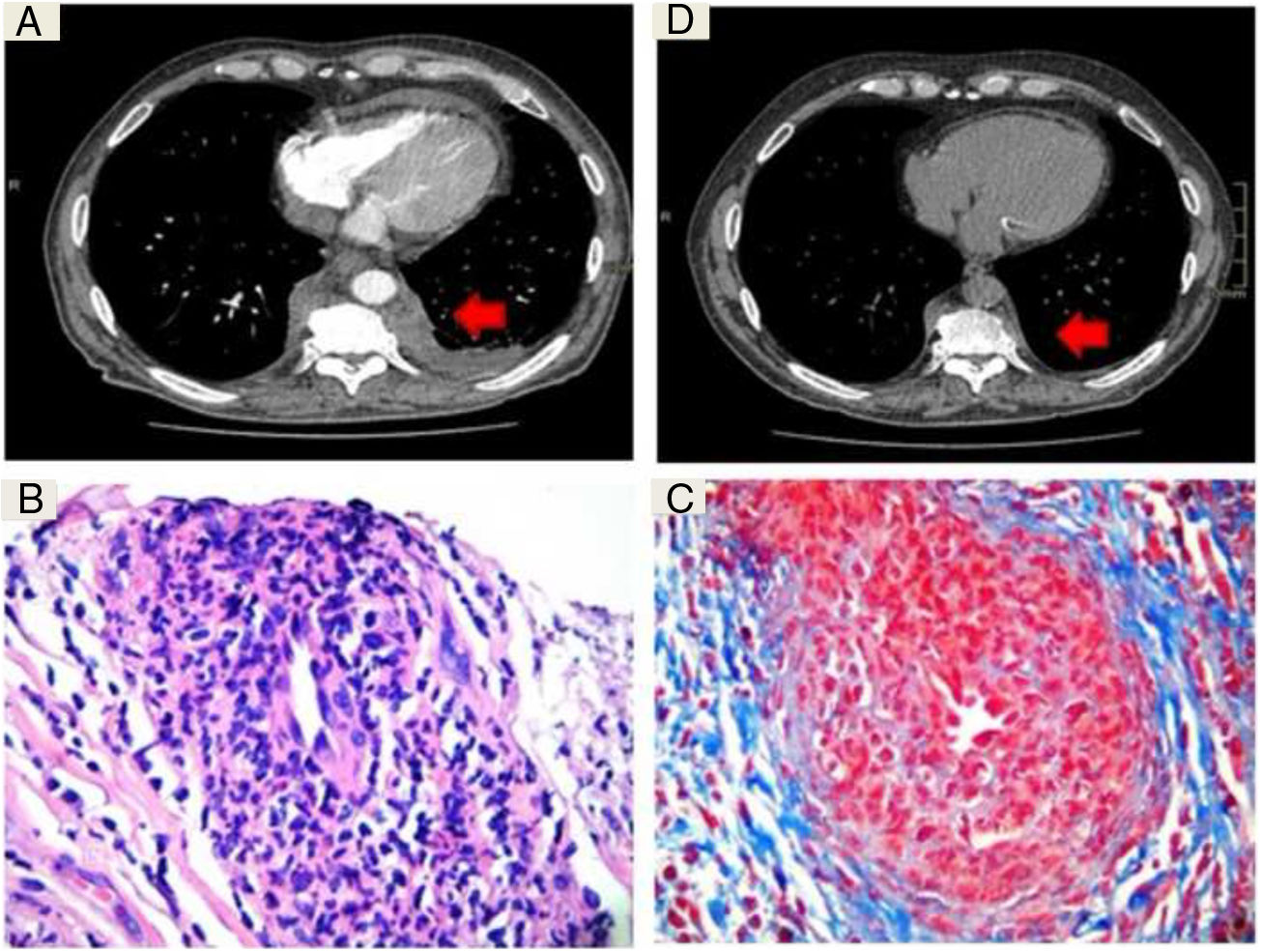
A 60 year-old man with arterial hypertension and chronic kidney disease that had evolved over 2 years, requiring haemodialysis and previous renal biopsy with sclerosed glomeruli, pericapsular and interstitial fibrosis and atrophic tubules. He visited due to weight loss over 3 months and palpable purpura in the lower limbs. He had symptoms of a compromised upper airway, renal involvement with haematuria and proteinuria in a non-nephrotic range with deterioration of kidney function. Laboratory tests found normocytic normochromic anaemia (haemoglobin 7.1 g/dl and haematocrit 21.9%), normal white blood cells (5,600/mm3), accelerated erythrosedimentation (70 mm/hr.), raised reactive C protein (3.19 mg/dl), creatinine (6.3 mg/dl), proteinuria/creatininuria quotient 2.1 and macroscopic hematuria. ANCA were positive, PR3 ELISA and cytoplasmic pattern in immunoflourescence. The antinuclear antibodies, anti-Ro/SS-A, anti-La/SS-B, anti-DNA and viral serologies for hepatitis B, C and HIV were negative. Computed tomography (CT) of the paranasal sinuses showed thickening of the mucosa and bone erosion, and high resolution CT of the thorax revealed centrolobulillar nodules and a paravertebral pseudotumour lesion (Fig. 1A). CT guided biopsy was performed and showed findings that could be associated with vasculitis without granulomatosis (Fig. 1B and C).
A) Computed tomography with intravenous contrast showing a dorsal paravertebral mass of soft tissues (arrow) which extends to the extrapleural space, without calcifications or bone involvement. B) Fragment of fibroconnective tissue that shows vascular elements with abundant intramural inflammatory infiltrate and reduction in the calibre of openings (H&E ×10). C) Artery with dense mixed inflammatory infiltrate composed of lymphocytes and polymorphonuclear neutrophils, prominent endothelial cells and a narrowed opening (Masson ×40). D) Computed tomography without contrast at check-up, showing a reduction in the lesion after 4 months of treatment.
Due to the said clinical findings, the positive ANCA and the histological changes in the paravertebral mass, GPA was diagnosed and induction therapy commenced with pulses of methylprednisolone and cyclophosphamide (15 mg/kg/every 15 days/6 doses). Thoracic CT was performed after 4 months, finding a significant reduction in the size of the lesion (Fig. 1D).
Infiltrating pseudotumour lesions are frequent in patients with GPA. The may be located in the orbit, paranasal sinuses, the mediastinum, breast, kidney and retroperitoneum, among other locations.1 Paravertebral lesions are rare,2,3 and to our knowledge only 10 cases have been reported in this location, although there are other reports of mediastinal lesions.2,3 They may present at the moment the disease starts or during its evolution.2,3 The frequency of such lesions may be underestimated as 50% of cases are asymptomatic and are not associated with bone erosion or the compression of adjacent structures.2 Some patients may experience chronic thoracic pain.3 Thoracic CT with contrast and magnetic resonance imaging studies are the main studies suggested for the detection of these lesions and to establish differential diagnoses. Histopathology is essential for diagnosis.2–4 It also makes it possible to rule out malignity and other differential diagnoses such as tuberculosis, mycosis, sarcoidosis, histiocytosis and disease associated with IgG4.4–6 This lesion location gives rise to difficulties in obtaining histological samples, so that it is suggested that a CT-guided biopsy be performed.2,3 The samples obtained usually show granulomatose infiltrates, rarely vasculitis and calcifications.2–7 After treatment, the inflammatory lesions may reduce in size, while the lesions that have evolved the most and fibrosis are unchanged.2–6
To conclude, GPA should be suspected if there is a finding of paravertebral pseudotumours within an appropriate clinical context. Obtaining samples for histopathological study is fundamental for the etiological diagnosis.
Please cite this article as: Flores Balverdi J, Baenas DF, Riscanevo NC, Chiple E, Orozco M, Saurit V. Seudotumor paravertebral en granulomatosis con poliangeítis. Reumatol Clin. 2021;17:181–182.