Pulmonary hypertension (PH) associated with systemic sclerosis (SSc) increases morbidity and mortality. Cardiopulmonary comorbidities, as per the 2021 PH consensus, play a role in the choice of therapy between monotherapy and combination therapy.
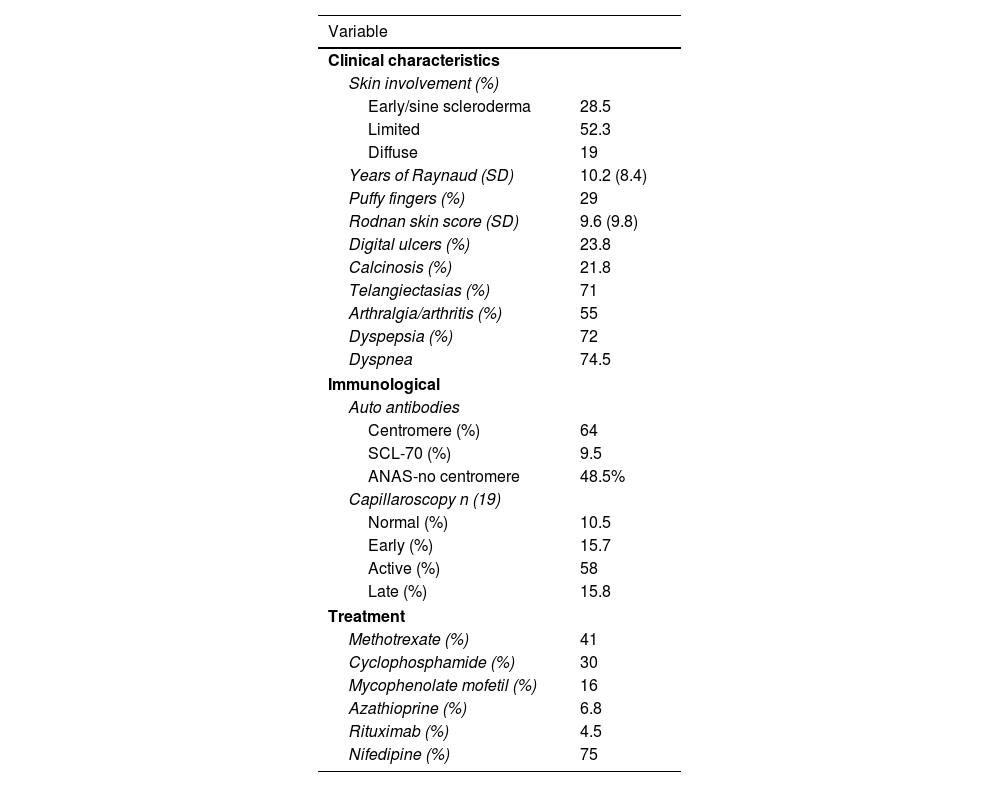
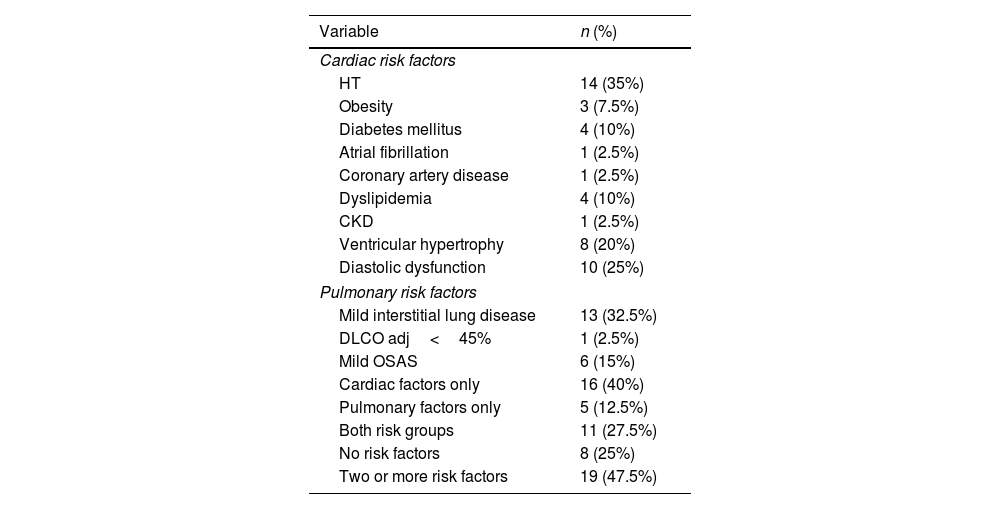
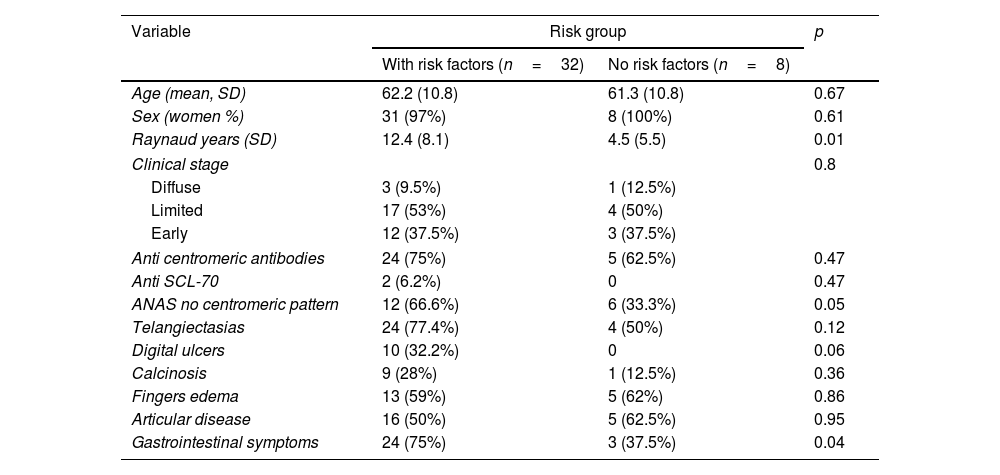
MethodsA cross-sectional study was conducted in patients with SSc based on the 2013 ACR/EULAR criteria or very early disease (VEDOSS 2011). PH was considered if they met the following criteria: pulmonary artery systolic pressure (PASP)>39mmHg or peak tricuspid regurgitation velocity (PTRV)>3.4m/s, PASP between 33 and 39mmHg or PTRV between 2.9 and 3.4m/s plus two additional findings suggestive of PH. PH was classified as type 2 if LVEF<50% or moderate to severe diastolic dysfunction was present; type 3 if extensive interstitial disease on tomography>20% or forced vital capacity (FVC)<75%; type 4 if abnormalities related to embolism were detected on scintigraphy or tomography. If patients did not meet these criteria, they were classified as type 1 PH. Complete data on cardiopulmonary risk factors and other factors were required. The frequency of these factors in the population and differences between groups based on risk factors were estimated.
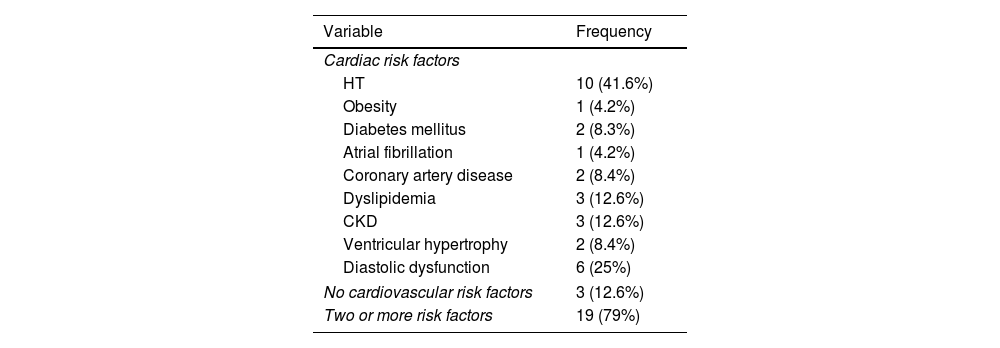
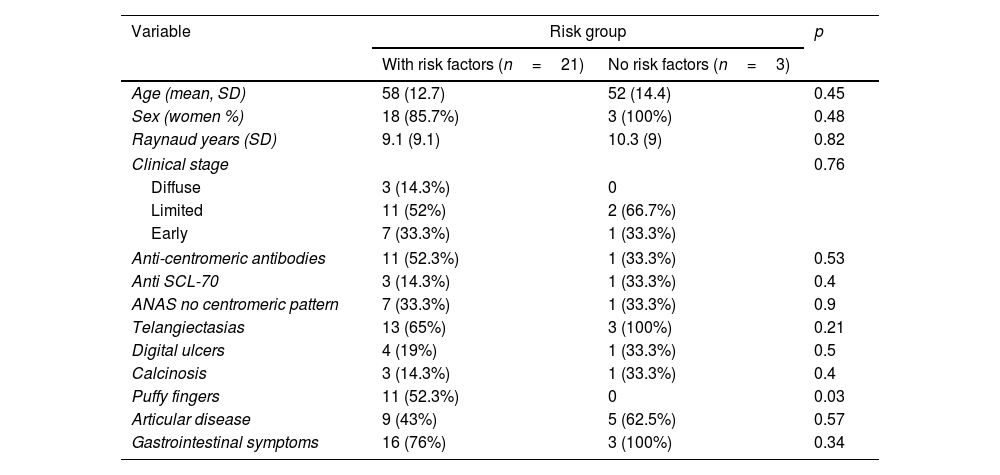
ResultsA total of 228 patients were selected. Three had type 2 PH, 24 had type 3, and 40 had type 1 PH, with the majority (75%) having at least one cardiopulmonary risk factor, and 47.5% having more than one. Mild diastolic dysfunction (25%) and hypertension (35%) were the most prevalent. In the type 1 PH group, those with risk factors experienced an increase in the number of years with Raynaud's phenomenon, anticentromere antibodies, and gastrointestinal symptoms (p<0.05).
ConclusionIn patients with PH, 75% have one, and 45% have two or more risk factors.
La hipertensión pulmonar (HP) asociada con esclerosis sistémica aumenta la morbimortalidad. Las comorbilidades cardiopulmonares, del consenso de la HP del 2021 desempeñan un papel en la elección de la terapia entre monoterapia y combinada.
MétodosSe llevó a cabo un estudio transversal en pacientes con esclerosis sistémica según criterios ACR/EULAR 2013 o enfermedad muy temprana (VEDOSS 2011). Se consideró HP si cumplían los siguientes criterios: presión sistólica de la arteria pulmonar>39mmHg o velocidad máxima de regurgitación tricuspídea>3,4m/s, presión sistólica de la arteria pulmonar entre 33 y 39mmHg o velocidad máxima de regurgitación tricuspídea entre 2,9 y 3,4m/s más 2 hallazgos adicionales de HP. Se consideró HP tipo 2 si fracción de eyección del ventrículo izquierdo<50% o disfunción diastólica moderada a grave; HP tipo 3 si enfermedad intersticial extensa en tomografía>20% o capacidad vital forzada<75%; HP tipo 4 si presentaba anomalías en gammagrafía o tomografía relacionadas con embolia. Si no cumplían con lo anterior, se considero HP tipo 1. Debían tener datos completos sobre factores de riesgo cardiopulmonares además de otros. Se estimó la frecuencia de estos factores en la población y las diferencias entre grupos en función de factores de riesgo.
ResultadosSe seleccionaron 228 pacientes. Tres HP tipo 2, 24 tipo 3 y 40 como tipo 1, la mayoría (75%) tenía al menos un factor de riesgo cardiopulmonar y el 47,5% tenía más de uno. La disfunción diastólica leve (25%) y la hipertensión (35%) fueron los más prevalentes. En el grupo HP tipo 1, aquellos con factores de riesgo tuvieron aumento en el número de años con fenómeno de Raynaud, anticuerpos anticentrómero y síntomas gastrointestinales (p<0,05).
ConclusiónEn pacientes con HP, el 75% tiene uno y el 45% 2 o más factores de riesgo.