The association of erythroderma and dermatomyositis is rare. In 6 reported cases found by searching Pubmed, half of them were associated with digestive tract neoplasms (stomach and liver). We report the case of a 69 years-old woman with bilateral proximal weakness, joint pain, photosensitivity, facial and heliotrope erythema lasting 18 months. One month prior to hospital admission she showed progressive dysphagia and a universal erythema and scaling that affected mucosa, palms and soles with an accompanying weight loss of 10kg in 6 months. No malignancy was identified at any level despite an exhaustive search.
La asociación de eritrodermia y dermatomiositis es rara. En 6 casos encontrados mediante búsqueda en PubMed, la mitad de ellos se encontraron asociados a neoplasias del tubo digestivo (estómago e hígado). Se presenta el caso una mujer de 69 años con debilidad proximal bilateral, artralgias, fotosensibilidad, eritema facial y en heliotropo de 18 meses de evolución. Un mes antes de su ingreso hospitalario presentó disfagia alta progresiva y una dermatosis universal con eritema y escama que afectó a mucosas, palmas y plantas, acompañándose de pérdida de peso de 10kg en 6 meses. No se logró identificar neoplasia a ningún nivel a pesar de una búsqueda intencionada.
The association of eritrodermia and dermatomyositis is rare and has usually been related with neoplasia of the gastrointestinal tract (stomach and liver). Eerythroderma is a condition characterized by erythema and desquamation of more than 90% of the skin surface. Most cases are secondary to psoriasis, other dermatoses, adverse drug reactions or cutaneous T-cell lymphoma. 25%–30% of cases are considered idiopathic erythrodermas. Erythrodermas present with systemic symptoms such as fever, tachycardia, lymphadenopathy, hepatomegaly, edema and poikilothermia. Histological examination of the skin allows the establishment of a diagnosis in 53%–66% of cases.1 6 cases of an association between erythroderma and dermatomyositis were found in Anglo-Saxon literature, 3 of them with an associated malignancy (two gastric and one of the liver),2–4 in 2 it was not found despite being looked for and in one case it was not intentionally sought.5,6 The case in question, a woman of 69 years of age with no comorbidity and dermatomyositis, presented associated erythroderma, so we sought the presence of neoplasia.
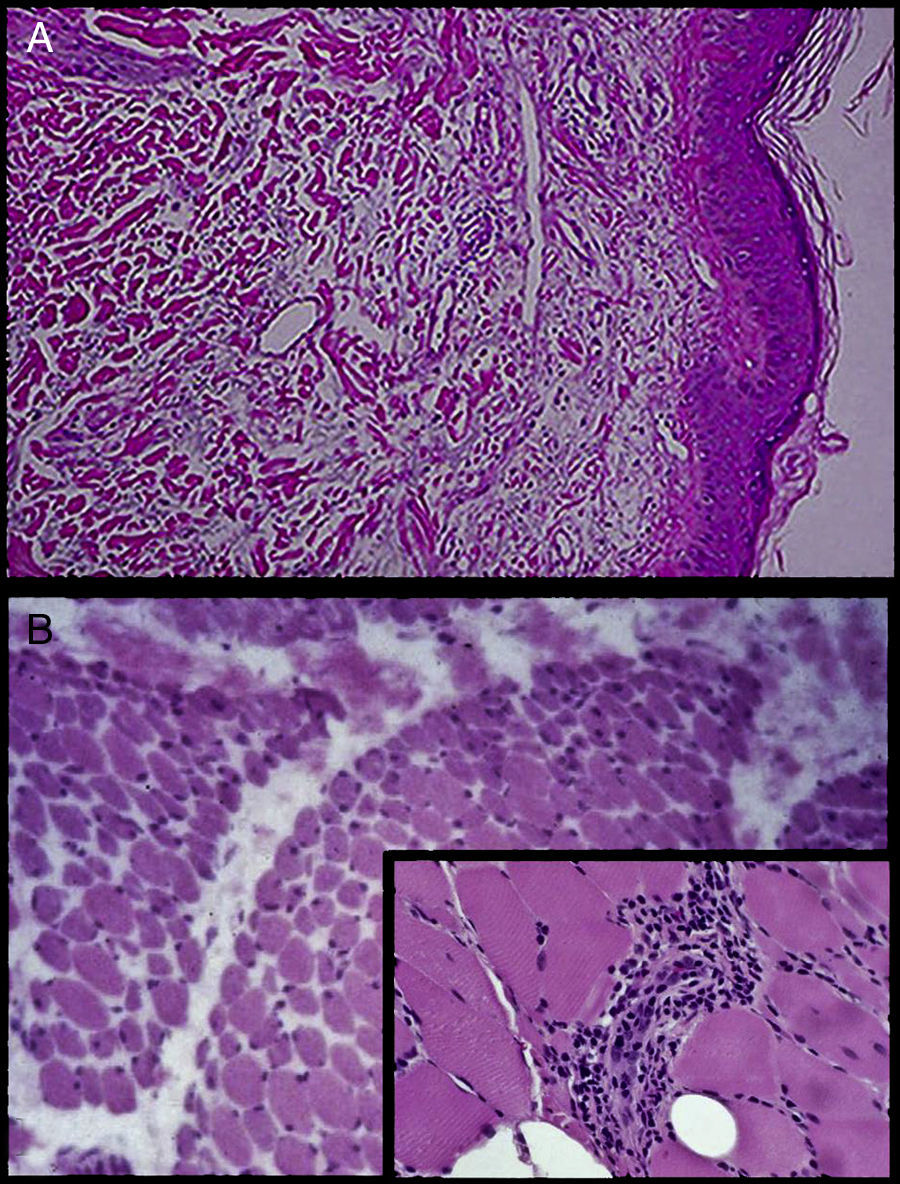
Case PresentationWe report the case of a 69-year-old woman without comorbidity. She had a history of 2 years with progressive proximal muscle weakness. A year later she had joint pain with no apparent synovitis, affecting small and large joints with progressive deterioration of functional class limiting her to her bed, and high progressive dysphagia, initially to solids and later liquids, accompanied by a loss of weight of 10kg. Six months before hospital admission she presented facial erythema, heliotrope rash (Fig. 1a) and photosensitivity. A month before the current hospitalization she presented a universal rash (95% of body surface) characterized by erythema, scaling and pruritus involving mucous membranes, palms and soles (Fig. 1b) and hair loss. During her hospital stay the following studies were performed: skin biopsy, which reported slight spongiosis and some mitosis in clear spaces of the dermis and an infiltrate of lymphocytes, plasma cells, and few eosinophils, as well as moderate diffuse edema of the papillary dermis distributed at the periphery of the annexes (Fig. 2a). Muscle biopsy showed inflammatory infiltrates predominantly of the perymisium and connective tissue and small vessels with endothelial injury and fibrosis (Fig. 2b) as well as perifascicular fiber atrophy. CPK was 2679U/dL. She had a positive antinuclear antibody titer of 1: 80 and a nucleolar pattern, anti-Mi-2 positive antibodies and negative anti-Jo-1 antibodies (immunofluorescence). Cervical cytology showed mild inflammation and a hormonal pattern consistent with atrophy. Upon examination of these mammary glands they were found to be in accordance to the age and gender of the patient without nodules. An endoscopy and gastric biopsy reported mild chronic superficial gastritis of the body and antrum. Finally, an abdominopelvic computed tomography with double contrast of the stomach found only a thickened body and antrum with no other abnormalities. The patient responded adequately in terms of muscle strength and dermatosis with steroid use, initially c using boluses of methylprednisolone (1g iv every 24h for 3 doses) and subsequently prednisone at a dose of 1mg/kg, in addition to the indication of emollients. There was later progression to sepsis secondary to a ventilator-associated pneumonia, and she presented an inferior acute myocardial infarction, dying on day 21 of hospitalization. No approval was obtained to perform an autopsy.
(A) Skin biopsy with slight spongiosis and some dermis mitosis in clear spaces with moderate edema and diffuse infiltration by lymphocytes, plasma cells and a few eosinophils, distributed in the papillary dermis and the periphery of the annexes. (B) Muscle biopsy: predominantly perimysial inflammatory infiltrates of connective tissue and small vessels, which have endothelial injury and fibrosis (zoomed image).
Erythrodermas is considered an emergency, so whenever possible the patient should be hospitalized. Fatal complications may occur without proper and timely treatment. The aims of treatment are to maintain skin moisture, prevent scratching and aggravating factors, and treat the underlying cause. All concomitant treatments that are not essential should be removed. It is advisable to apply emollients of topical corticosteroids after performing warm baths. Antibiotics are added to treatment if superinfections occur.1 In our case, dermatomyositis was initially treated with steroids, although other methods such as methotrexate, azathioprine, and combinations of these with biological therapy have been employed.7 Given the respiratory complications associated with mechanical ventilation and the fatal outcome we did not employ any of the alternatives mentioned. Our case adds to the few described in the medical literature that have reported the association between dermatomyositis and erythroderma. Despite a deliberate search we found no evidence of neoplasia. Although there are few reports on this association, the finding of cancer in half of them warrants a deliberate search of tumors, particularly intra-abdominal neoplasia.
Ethical ResponsibilitiesProtection of people and animalsThe authors state that no experiments were performed on humans or animals.
Data confidentialityThe authors state that no patient data appears in this article.
Right to privacy and informed consentThe authors state that no patient data appears in this article.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Valdés-González G, et al. Dermatomiositis-eritrodermia: presentación clínica no asociada a malignidad. Reporte de un caso. Reumatol Clin. 2014;10:48–50.