To assess therapeutic compliance in osteoporosis in women in a primary care (PC) setting.
Patients and methodsObservational, descriptive, cross-sectional and multicenter study, conducted in PC centers of the 17 Spanish autonomous regions. 1649 women who had initiated treatment for osteoporosis at least 3 months before entering the study were recruited. To assess therapeutic compliance, two questionnaires, the Haynes–Sackett or self-communicated compliance test (AC) and the Morisky–Green test (MG) were used.
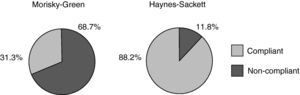
ResultsPatients’ mean age (±SD) was 66.59 years (9.5) and the mean time since diagnosis was 5.08 years (4.87). Bisphosphonates were the most prescribed drugs (82% of the patients) and only 52% of the patients were taking calcium and vitamin D supplements. Analysis of the therapeutic compliance level shows that, as per the MG test, 68.7% of the patients were non-compliers, and 11.2% were non-compliers as per the AC test.
ConclusionsAn important percentage of women with post-menopausal osteoporosis in Spain's PC setting show a high level of non-compliance.
Evaluar el cumplimiento del tratamiento farmacológico de la osteoporosis en mujeres atendidas en el ámbito de la Atención Primaria (AP). En la osteoporosis, como en otras enfermedades crónicas, el fomento del tratamiento a largo plazo es fundamental.
Pacientes y métodosSe trata de un estudio observacional, descriptivo, transversal y multicéntrico, realizado en Centros de Salud de AP de las 17 Comunidades Autónomas. Se reclutaron 1.649 mujeres que habían iniciado tratamiento farmacológico para la osteoporosis al menos 3 meses antes. Para evaluar el cumplimiento se utilizaron dos cuestionarios: el test de Haynes-Sackett o de cumplimiento autocomunicado (CA) y el test de Morisky-Green (MG).
ResultadosLa edad media (± DE) de las pacientes era de 66,6 años (9,5) y el tiempo medio desde el diagnóstico era de 5,1 años (4,9). El tratamiento más prescrito fueron los bisfosfonatos (82% de las pacientes) y sólo un 52% recibía suplementos de calcio y vitamina D. El análisis del nivel de cumplimiento muestra que el 68,7% fue incumplidora según el test de MG, y el 11,2% fue incumplidora según el test de CA.
ConclusionesUn porcentaje importante de las mujeres con osteoporosis posmenopáusicas atendidas en AP en España presenta un elevado incumplimiento terapéutico.
Osteoporosis is the most common metabolic bone disease, but it is difficult to establish its real prevalence, since it is asymptomatic until the onset of complications. The management of osteoporosis in individuals at high risk of fracture include the identification of such risk factors,1–3 the choice of optimal therapy, and given its chronic and asymptomatic nature, the promotion of long-term compliance,4 defined as the extent to which the patient takes the advice given by the physician or medical personnel regarding lifestyle habits and pharmacological treatment.5,6 Although, in general, it is considered that the degree of compliance varies between 20% and 90%, the most accepted rates are between 40% and 60%.7–9
The assessment of compliance is not easy, and although there are multiple methods for its analysis, there is not a single one that allows for a safe clinical measurement. Different methods,10 which can be divided into direct determination based on blood or urine of active substances or metabolites; and indirect, less reliable but less expensive and easier to implement, reflect the behavior of patients and are most useful in primary care (PC), and include pill counts and clinical interviews. The interview-based methods most commonly used are the Sackett–Haynes11 clinical test, or self-reported compliance (SC) and the Morisky test–Green12 test (MG). Although the SC test tends to overestimate compliance and MG test tends to overestimate it, a review of the literature shows that they are often used together when assessing compliance through indirect methods. Adherence to therapy has been widely discussed in hypertension (HT), diabetes and dyslipidemia.13,14 However, despite the chronicity and high prevalence of osteoporosis, studies of compliance, particularly in Spain are scarce. For this reason, the present study's objective was to evaluate the compliance with osteoporosis treatment in women in PC, through the use of such questionnaires, and analyze the degree of agreement between those measuring instruments.
Patients and MethodsThis was an observational, cross sectional and multicenter study performed in PC Health Centers of the17 Spanish regions over a period of 4 months. The study was approved by the Research Ethics Committee of the Hospital Clínic de Barcelona. 150 researchers participated. Each was asked to include 10 consecutive postmenopausal women with osteoporosis who had started drug treatment for this condition at least 3 months before attending for any reason in the consultation and, after being informed, signed consent to participate the study.
The variables collected during a single visit were: demographic and anthropometric (age, height, weight, body mass index [BMI], educational level and cohabitation data), clinical characteristics of osteoporosis (date of diagnosis, clinical/densitometric diagnostic criteria, past values of bone mineral density [BMD] available, number and type of fracture if appropriate, date of start of treatment and reviews).
The level of awareness of the disease was assessed by the Batalla15 test, a questionnaire of three questions that can distinguish between three knowledge levels: acceptable (if the patient knows that osteoporosis is a chronic, treatable condition, and experiences a complication), unacceptable (if not aware of any complications) and moderately acceptable (in other cases).
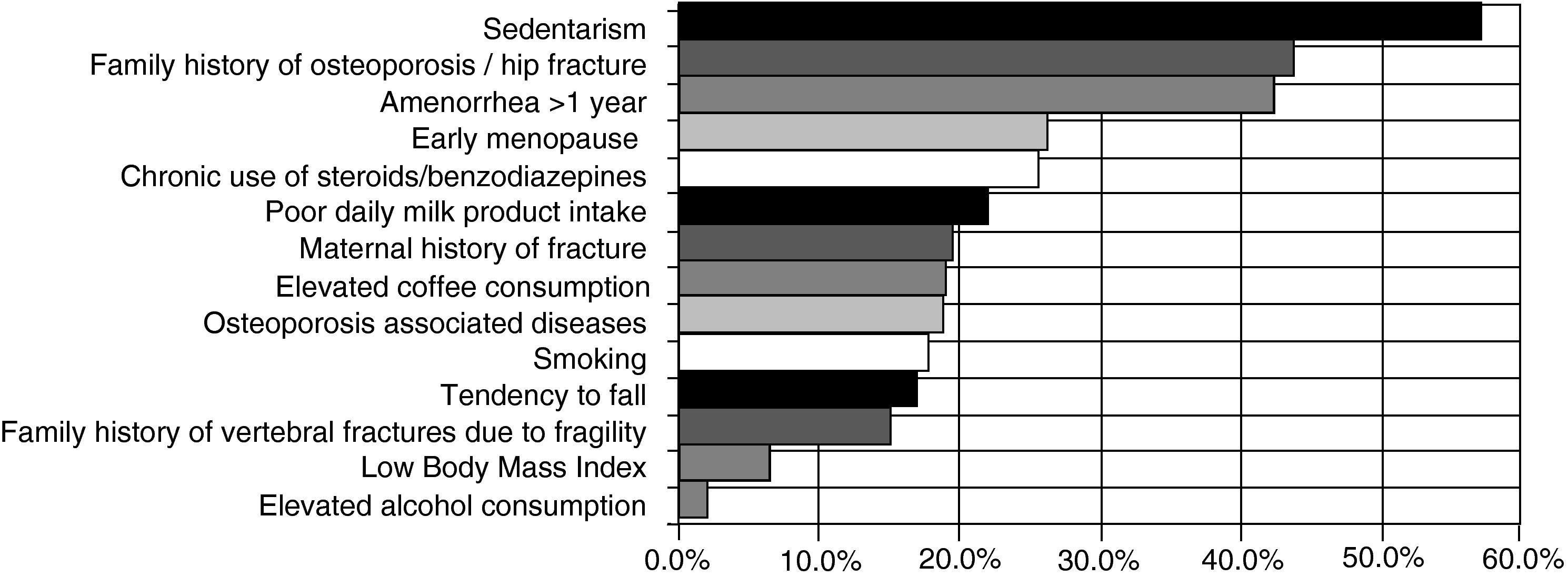
Risk factors for osteoporosis considered were smoking, categorizing the patient as a nonsmoker, ex-smokers (smoking cessation at least 1 year before) or currently smoking (≥10 cigarettes/day regularly), in which case we recorded the number of cigarettes a day and age at onset of consumption, heavy alcohol consumption (>50g/day) and/or coffee (>4cups/day), sedentary lifestyle (dedicating <30–40min 3–4 times a week for walking, running or swimming), early menopause (<45 years), amenorrhea >1 year, BMI <19, daily consumption of milk, personal history of fragility fracture (starting at age 40), a maternal history of femur fracture, a family history of osteoporosis and/or hip fracture, chronic use of corticosteroids and/or benzodiazepines; osteoporosis associated diseases, and a tendency to fall, indicated by the number of falls during the past year. Also recorded were the presence of other comorbidities, with particular emphasis on hypertension, cerebrovascular disease, heart disease, dyslipidemia and diabetes.
Concerning drug treatment at the time of the visit, we recorded the number of daily drugs (anti-osteoporotic and others), the prescribed drug group, the active ingredient, duration of treatment, dosage and frequency of administration. We also collected information in supplements such as calcium and/or vitamin D. Finally, to assess compliance with treatment for osteoporosis, we administered the MG12 and AC11 test and questionnaire:
- -
The MG test considers those who correctly answer the four questions of the questionnaire as compliant patients, that is, they never forget to take medication, do so at the times indicated and do not stop taking it regardless of how they feel. An adequate response to two or three questions is considered an acceptable level of compliance.
- -
The AC questionnaire serves to determine if patients have difficulty taking their medication and then asks about these difficulties. If so, it questions the number of pills taken in the last month, considering that a compliant patient will have a percentage between 80% and 110%.
These two indirect methods of measuring compliance have been validated in other diseases in the Spanish population such as hypertension,16–20 dislipidemias21 and diabetes.22 To avoid the bias of patients wishing to be qualified positively23 by health personnel and to avoid the potential underestimation of non-compliant patients, questionnaires were given to patients in a sealed envelope with the patient self-administering it, without the researcher having access to them.
Statistical AnalysisQuantitative variables were expressed by measures of central tendency and dispersion (mean and standard deviation) and qualitative variables as absolute and relative frequencies, including the respective confidence interval (CI) of 95%.
The percentage of compliance obtained by both methods was compared with Chi square test and the degree of agreement among them calculated as the simple proportion of agreement and kappa statistics (κ), which applies a correction to take into account random correlation.
SAS software version 8.2 was used for statistical analysis and a prefixed a significance level of 5% was set.
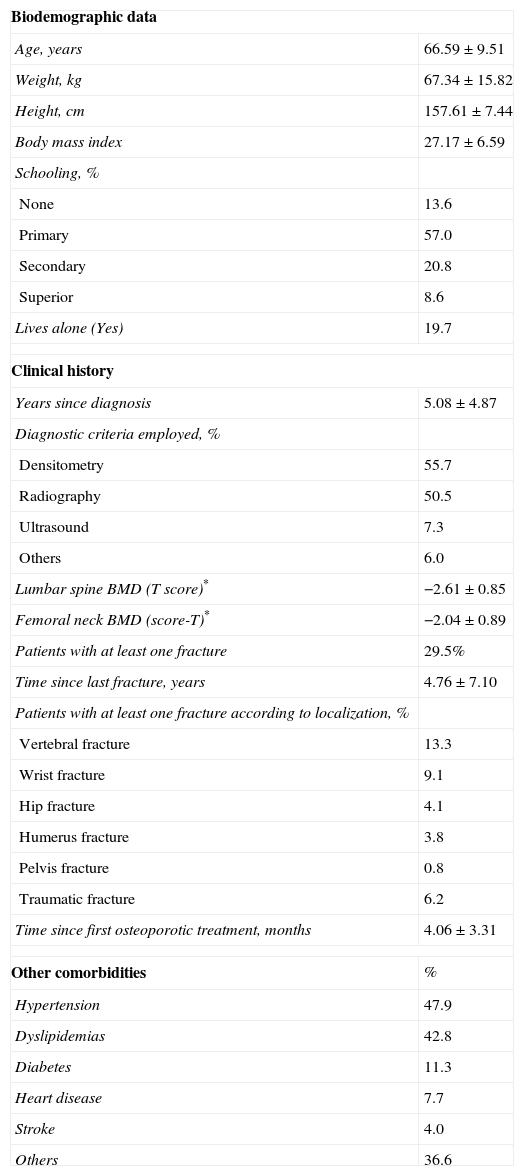
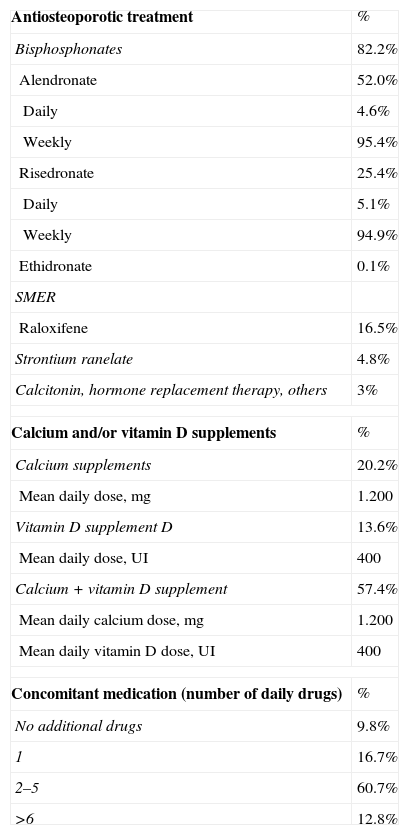
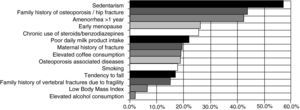
ResultsA total of 1649 patients were enrolled for evaluation. The mean age (±SD) of the patients was 66.6 years (9.5) (Table 1), average time from diagnosis was 5.1 years (4.9). The remaining clinical and demographic characteristics are shown in Table 1. Fig. 1 shows the prevalence of different risk factors assessed. Anti-osteoporotic treatment at the time of the visit (Table 2) was led by bisphosphonates, which accounted for over 80% of the total.
Characteristics of the Studied Population of Postmenopausal Women With Osteoporosis Treated in Primary Care.
| Biodemographic data | |
| Age, years | 66.59±9.51 |
| Weight, kg | 67.34±15.82 |
| Height, cm | 157.61±7.44 |
| Body mass index | 27.17±6.59 |
| Schooling, % | |
| None | 13.6 |
| Primary | 57.0 |
| Secondary | 20.8 |
| Superior | 8.6 |
| Lives alone (Yes) | 19.7 |
| Clinical history | |
| Years since diagnosis | 5.08±4.87 |
| Diagnostic criteria employed, % | |
| Densitometry | 55.7 |
| Radiography | 50.5 |
| Ultrasound | 7.3 |
| Others | 6.0 |
| Lumbar spine BMD (T score)* | −2.61±0.85 |
| Femoral neck BMD (score-T)* | −2.04±0.89 |
| Patients with at least one fracture | 29.5% |
| Time since last fracture, years | 4.76±7.10 |
| Patients with at least one fracture according to localization, % | |
| Vertebral fracture | 13.3 |
| Wrist fracture | 9.1 |
| Hip fracture | 4.1 |
| Humerus fracture | 3.8 |
| Pelvis fracture | 0.8 |
| Traumatic fracture | 6.2 |
| Time since first osteoporotic treatment, months | 4.06±3.31 |
| Other comorbidities | % |
| Hypertension | 47.9 |
| Dyslipidemias | 42.8 |
| Diabetes | 11.3 |
| Heart disease | 7.7 |
| Stroke | 4.0 |
| Others | 36.6 |
Values expressed as mean±SD.
BMD: bone mineral density.
Antiosteoporotic Treatment and Concomitant Medication Used by Patients at the Time of Visit.
| Antiosteoporotic treatment | % |
| Bisphosphonates | 82.2% |
| Alendronate | 52.0% |
| Daily | 4.6% |
| Weekly | 95.4% |
| Risedronate | 25.4% |
| Daily | 5.1% |
| Weekly | 94.9% |
| Ethidronate | 0.1% |
| SMER | |
| Raloxifene | 16.5% |
| Strontium ranelate | 4.8% |
| Calcitonin, hormone replacement therapy, others | 3% |
| Calcium and/or vitamin D supplements | % |
| Calcium supplements | 20.2% |
| Mean daily dose, mg | 1.200 |
| Vitamin D supplement D | 13.6% |
| Mean daily dose, UI | 400 |
| Calcium+vitamin D supplement | 57.4% |
| Mean daily calcium dose, mg | 1.200 |
| Mean daily vitamin D dose, UI | 400 |
| Concomitant medication (number of daily drugs) | % |
| No additional drugs | 9.8% |
| 1 | 16.7% |
| 2–5 | 60.7% |
| >6 | 12.8% |
Percentages calculated over total patients under evaluation.
SMER: selective modulators of estrogen receptors.
Regarding the level of knowledge of the disease, 24.1% of patients showed unacceptable knowledge of osteoporosis, while the percentages of acceptable and moderately acceptable knowledge were similar (40.9% and 35% respectively).
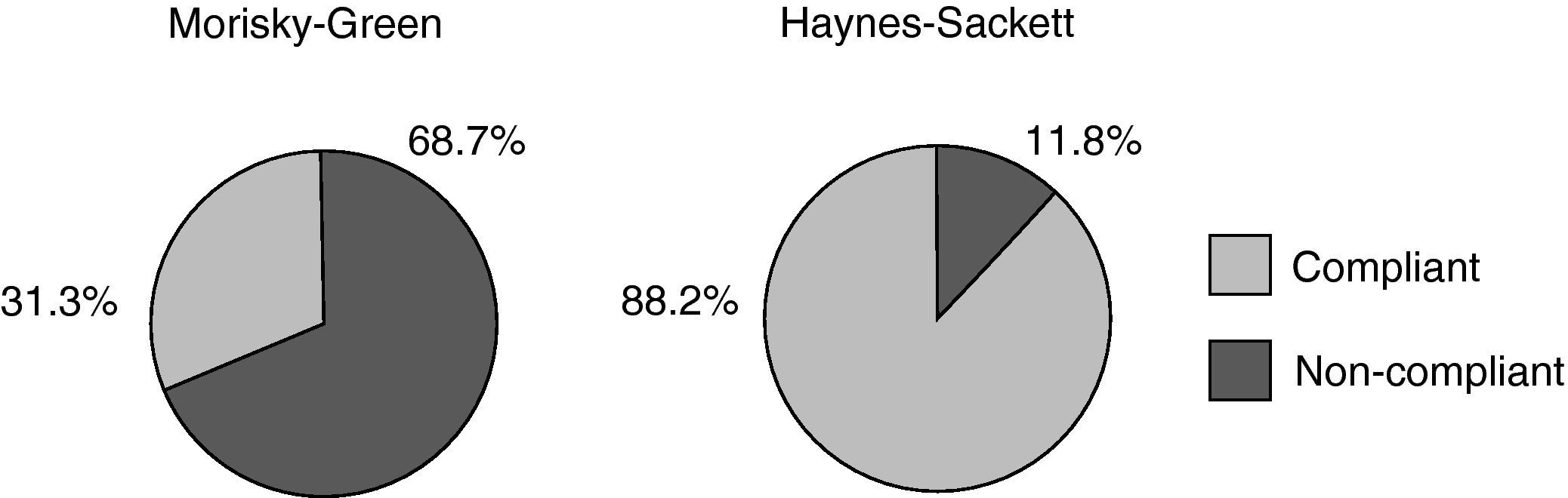
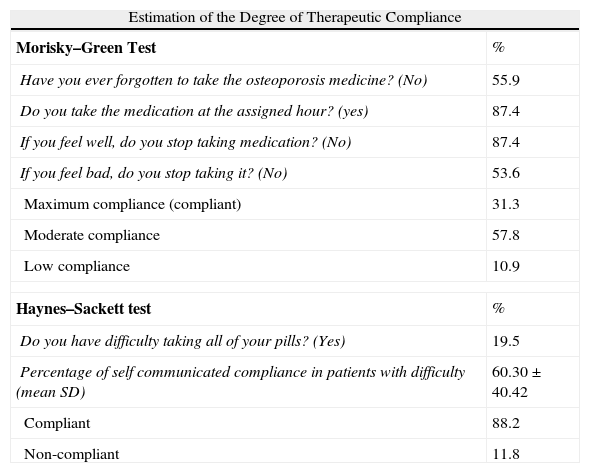
When we analyzed the level of compliance with anti-osteoporotic treatment, 31.3% was considered compliant when applying the MG test (Table 3, Fig. 2), while the remaining two thirds (68.7%) were classified as non-compliant (the 57.8% compliance in the category of moderate and 10.9% in the low compliance category.) The AC test, however, estimated a rate of 88.2% compliance.
Comparison of Indirect Compliance Evaluation Methods.
| Estimation of the Degree of Therapeutic Compliance | |
| Morisky–Green Test | % |
| Have you ever forgotten to take the osteoporosis medicine? (No) | 55.9 |
| Do you take the medication at the assigned hour? (yes) | 87.4 |
| If you feel well, do you stop taking medication? (No) | 87.4 |
| If you feel bad, do you stop taking it? (No) | 53.6 |
| Maximum compliance (compliant) | 31.3 |
| Moderate compliance | 57.8 |
| Low compliance | 10.9 |
| Haynes–Sackett test | % |
| Do you have difficulty taking all of your pills? (Yes) | 19.5 |
| Percentage of self communicated compliance in patients with difficulty (mean SD) | 60.30±40.42 |
| Compliant | 88.2 |
| Non-compliant | 11.8 |
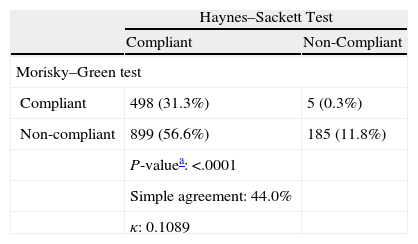
Agreement between the results of different methods was not significant24 (κ<0.2) (Table 4). Differences observed between the results of the MG and AC tests were statistically significant (p<.0001), although agreement was greater in the case of non-compliance; 97.4% of non-compliant according to the AC test were also non-compliant according to the MG test.
Agreement Between the Results of Different Compliance Measuring Methods.
| Haynes–Sackett Test | ||
| Compliant | Non-Compliant | |
| Morisky–Green test | ||
| Compliant | 498 (31.3%) | 5 (0.3%) |
| Non-compliant | 899 (56.6%) | 185 (11.8%) |
| P-valuea: <.0001 | ||
| Simple agreement: 44.0% | ||
| κ: 0.1089 | ||
Simple agreement=[(compliant+non-compliant on both tests)/totals]×100.
κ=(Po−Pe)/(1−Pe), where Po proportion of observed agreement and Pe the proportion of random agreement (in this case, 0.5).
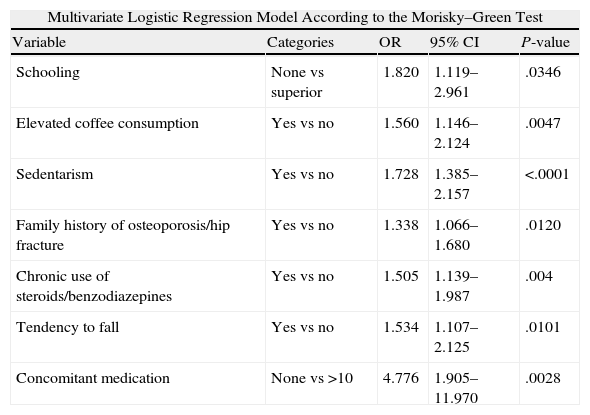
Table 5 shows the results of the different variables included in multivariate models for poor compliance as defined by the methods of MG and CA. The first includes the educational level, high coffee consumption, physical inactivity, family history of osteoporosis and/or hip fracture, chronic use of corticosteroids and/or benzodiazepines, falls and concomitant medication. Thus, patients with no education or primary education are, respectively, 82% and 57% more likely to be non-compliant than women with higher education, the patients who take fewer pills are 3–5 times more likely to fail treatment than those taking more than 10, and the presence of all other factors increases the probability of non-compliance, including a sedentary lifestyle, which reaches 73%. The second model, however, includes knowledge of the disease, high coffee consumption, sedentary lifestyle, dairy consumption, diabetes, treatment with calcitonin and concomitant medication. However, 95% showed inconclusive results for the degree of knowledge and concomitant medications. Patients who do not consume dairy products are 1.62 times more likely to be non-compliant, as well as diabetics, whose tendency to not comply with treatment is 63% larger. As regards consumption of coffee and a sedentary lifestyle, the only common factor in both models, it increases the probability of non-complying with the treatment to 54% and 87% respectively.
Multivariate Logistic Regression Models Used to Predict the Degree of Non-Compliance According to the Morisky–Green and Haynes–Sackett Tests.
| Multivariate Logistic Regression Model According to the Morisky–Green Test | ||||
| Variable | Categories | OR | 95% CI | P-value |
| Schooling | None vs superior | 1.820 | 1.119–2.961 | .0346 |
| Elevated coffee consumption | Yes vs no | 1.560 | 1.146–2.124 | .0047 |
| Sedentarism | Yes vs no | 1.728 | 1.385–2.157 | <.0001 |
| Family history of osteoporosis/hip fracture | Yes vs no | 1.338 | 1.066–1.680 | .0120 |
| Chronic use of steroids/benzodiazepines | Yes vs no | 1.505 | 1.139–1.987 | .004 |
| Tendency to fall | Yes vs no | 1.534 | 1.107–2.125 | .0101 |
| Concomitant medication | None vs >10 | 4.776 | 1.905–11.970 | .0028 |
| Multivariate Logistic Regression Model According to the Haynes–Sackett Test | ||||
| Variable | Categories | OR | 95% CI | P-value |
| Level of knowledge of the disease | Unacceptable vs acceptable | 0.719 | 0.453–1.142 | .0346 |
| Elevated coffee consumption | Yes vs no | 1.540 | 1.063–2.232 | .0047 |
| Sedentarism | Yes vs no | 1.868 | 1.316–2.653 | <.0001 |
| Daily milk-product consumption | Yes vs no | 0.382 | 0.274–0.534 | .0120 |
| Diabetes | Yes vs no | 1.633 | 1.045–2.553 | .004 |
| Concomitant medication | None vs >10 | 0.743 | 0.146–3.777 | .0028 |
OR: odds ratio; CI: confidence interval.
Adherence to treatment in clinical practice is difficult and complex to measure by the diversity of factors involved. This study shows that the range of compliance for osteoporosis in a sample of 1649 postmenopausal women in the area of PC is wide and varies according to the indirect method used for evaluation.
The results show that the MG test, which generally overestimates poor compliance, classifies 31.3% of patients as compliant and 68.7% as non-compliant. The AC test, which tends to overestimate good compliance, classifies 88.2% of patients as compliant and 11.8% as non-compliant.
The rate of non-compliance using AC (11.8%) is close to 13.3%, obtained using the same method in a preliminary study, conducted on 83 Spanish male and female osteoporotic patients, attended at the Metabolic Bone Pathology Unit,24 and 10.5% obtained in a study of 240 patients with postmenopausal osteoporosis treated in Rheumatology.25 Instead, non-compliant patients with the GM test in a previous work represented 44.6% and 45% respectively, compared with 68.7% in our study. These differences could be explained by the higher level of education for the population studied and the scope of the study (PC vs Specialty Care). Similarly, a previous study26 that compared the compliance of postmenopausal women treated with alendronate or raloxifene, found a 9.4% and 46% of non-compliant patients according to CA and MG tests, respectively, among patients receiving alendronate, which most of the population evaluated took as treatment (82.2%).
The low correlation between these two methods for assessing compliance is a common phenomenon seen in studies of chronic diseases.9 The MG test assesses whether the patient takes the right attitudes regarding therapy, but the concept of compliance is very strict and does not include patients with moderate compliance, and it is considered to underestimate compliance. The opposite occurs with the CA test, which has a high specificity but low sensitivity, so it tends to underestimate non-compliance. It would therefore be highly recommended in future studies that methods are identified to lower rates of validity for the detection of osteoporosis treatment non-compliance, especially considering the discrepancy found between the methods used in this study and others. Considering the results of the MG and CA tests, we observed that the lack of understanding of many patients (42.6%) that osteoporosis can be prevented by changing the lifestyle, and the stoppage of medication when the patient feels bad (46.4%) are issues that can influence non-compliance, but can be addressed through educational strategies that contribute to improving compliance to treatment.
When analyzing multivariate logistic regression models developed for the prediction of non-compliance by the MG and AC methods, we see a match of high coffee consumption and physical inactivity as predictors. It is difficult to interpret these data, which nonetheless is present in a high percentage of the population tested. It probably indicates a behavior or lifestyle associated with poor compliance.
The main limitation of this study was the use of indirect methods for assessing compliance when they are not the most reliable. But, in the field of PC, they fulfill the premise of being simple and easy to apply, and that, at least, produce information that can help the clinician to recognize the problem and later approach it. It can be concluded that a significant percentage of women with postmenopausal osteoporosis treated at PC in Spain have a high non-compliance rate for osteoporosis therapy. Improved educational measures should be performed in patients, emphasizing the level of knowledge and the importance of optimal adherence.
Role of the Funding SourceGlaxoSmithKline and Roche Farma financed this study.
Conflict of InterestThe authors have no conflict of interest to declare.