Psoriatic arthritis (PsA) is a chronic inflammatory disorder that primarily affects the joints and entheses. In addition, it is associated with depressive syndrome (DS), cardiovascular disease, hypertension (HT), diabetes mellitus (DM), obesity and psoriasis (Pso). There are few studies aimed to analyze the association of the involvement of the musculoskeletal system with sexual function (SF).
MethodsA cross-sectional observational study was proposed in patients diagnosed with PsA, to whom self-administered validated questionnaires were applied to determine alterations in SF: MGH-SFQ and CSFQ-14, which assess the 4 domains of sexual function; Qualisex and DLQI designed for joint and dermatological pathology respectively, which explore sexual aspects. The objective was to describe the existence of altered sexual function in patients with PsA; analyze the association between sociodemographic characteristics, comorbidities (Pso, DS, cardiovascular risk factors) and the treatments of patients on SF; and describe differences of SF according to gender.
Results72 patients were evaluated. It was observed that the variables of patients with PsA that were associated with lower scores in SF were gender and age in the CSFQ-14 and MGH-SFQ; annual incomes, treatment with NSAIDs, DL and depression were associated with worse results in some domains of the sexual sphere.
ConclusionsPatients with PsA had impaired SF, especially women, elder patiens, those with low annual incomes, DL and emotional disorders. Anti-inflammatory treatments were associated with better SF. Globally, the chronic disease and the psychological burden behaved as factors associated with sexual dysfunction.
La artritis psoriásica (APs) es un trastorno inflamatorio crónico que afecta principalmente a las articulaciones y las entesis. Además, se asocia con el síndrome depresivo (SD), la enfermedad cardiovascular, la hipertensión (HTA), la diabetes mellitus (DM), la obesidad y la psoriasis (Pso). Existen pocos estudios dirigidos a analizar la asociación de la afectación del aparato locomotor con las alteraciones de la calidad sexual (CS).
MétodosSe propuso un estudio observacional transversal en pacientes diagnosticados de APs a los que aplicaron cuestionarios validados autoaplicados para determinar alteraciones de la CS: MGH-SFQ y CSFQ-14, que valoran los 4 dominios de la función sexual; Qualisex y DLQI diseñados para patología articular y dermatológica respectivamente, que exploran aspectos sexuales. El objetivo fue describir la existencia de alteraciones sexuales de pacientes con APs; analizar la asociación entre las características sociodemográficas, comorbilidades (Pso, SD, factores de riesgo cardiovascular) y los tratamientos de los pacientes sobre la CS; y describir diferencias de CS en función del género.
ResultadosSe valoraron 72 pacientes y se observó que las variables de los pacientes con APs que se asociaron con mayor fuerza con puntuaciones más bajas en CS fueron ser mujer y la edad en el CSFQ-14 y MGH-SFQ; el nivel de ingresos, el tratamiento con AINE, la DL y la depresión se asociaron a peores resultados en algunos dominios de la esfera sexual.
ConclusionesLos pacientes con APs presentaban una CS deteriorada, especialmente mujeres, de mayor edad, bajo nivel de ingresos y DL. Los tratamientos antiinflamatorios se asociaron con mejor CS. Globalmente, la enfermedad crónica y la carga psicológica de padecerla, se comportaron como factores predisponentes de disfunción sexual.
Psoriatic arthritis (PsA) is a chronic inflammatory disorder mainly affecting the joints and entheses of the locomotor system. Its prevalence ranges from .3% to 1% of the general population,1 with a higher prevalence in patients with psoriasis (Pso)2 of 6%–42%. Psoriasis is also associated with depressive syndrome, cardiovascular disease, hypertension, diabetes mellitus, and obesity.3,4 There is little evidence linking locomotor system involvement with sexual dysfunction (SD). Although most of the published studies that analyse the influence of joint pathology on sexuality have been conducted on patients with rheumatoid arthritis (RA),5,6 it is known that other rheumatic diseases, including PsA, affect sexuality and intimacy in sexual relations, either due to involvement of the locomotor system or the emotional system.7,8
Sexual response is defined as the sequence of physical and emotional changes occurring when a person becomes sexually aroused and engages in sexually stimulating activities such as intercourse or masturbation. The four stages of the sexual response cycle are excitement, plateau, orgasm, and resolution. The largest study to date assessing various sexual aspects of personal relationships, the Global Study of Sexual Attitudes and Behaviors,9 included more than 29 countries and 27,500 individuals. This study showed discretely different SD figures between genders, with 39% of women and 28% of men reporting at least one SD. The most frequently described SDs were premature ejaculation and erectile dysfunction in men, and lack of sexual interest, inability to reach orgasm and lubrication difficulties in women.9,10 In addition, a large proportion of women experience multiple SDs. Finally, there is less comorbidity among SDs in men compared to women.10 In patients with PsA who have concomitant skin involvement in the form of Pso, there is a higher prevalence of sexual disturbances.7,11 In particular, it has been observed that patients with Pso have a higher risk of SD and erectile dysfunction than healthy individuals, regardless of physical and psychological comorbidities. Among patients with Pso, those with anxiety, depression, genital PsA and, therefore, poorer quality of life, have a higher risk of SD,12 but these data have not been corroborated in PsA.
Numerous scales or indices are used in routine clinical practice to assess inflammatory disease activity and the impact on patients' quality of life, but these do not include any specific section aimed at assessing the sexual sphere. The ASAS Health Index questionnaire (ASAS-HI),13 which measures the effect on health in spondyloarthropathies and refers to sex life in one item: “I have lost interest in sex”, is worth mentioning. However, it does not go into the impact that inflammatory joint disease may have on sexuality.
The aim of our study was to examine the prevalence of altered sexual functioning in patients with PsA, and to determine associations with sociodemographic variables, comorbidities and characteristics of psoriatic disease.
Material and methodsWe conducted a cross-sectional observational study in the rheumatology clinics of a university hospital. We included patients over 18 years of age of both sexes and any sexual orientation, diagnosed with PsA, according to CASPAR criteria, with a minimum time from diagnosis of one year and having at least two registered clinical visits. Patients who refused to participate in the study or did not meet the inclusion criteria were not included.
Demographic data, comorbidities, clinical symptoms and treatments used for PsA were collected from the electronic medical record. In addition, socio-demographic variables were collected from a patient self-completed questionnaire.
The main variable of the study was alteration in the sexual sphere in patients diagnosed with PsA, which was assessed by means of specific validated questionnaires, which are detailed below:
- •
Changes in Sexual Functioning Questionnaire (CSFQ).14,15 A short version, the CSFQ-14, is available and consists of 14 questions. It assesses the domains of pleasure, desire, arousal, and orgasm. Questions 10 (on loss of interest after arousal in women, and priapism in men) and 14 (on painful orgasm) are only included in the total score. The theoretical maximum total score is 70, a score of less than 41 indicates SD.16
- •
Massachusetts General Hospital-Sexual Functioning Questionnaire (MGH-SFQ).17 The questionnaire includes five items that assess sexual functioning in the past month, associated with sexual desire, arousal, erection (in men), orgasm, and sexual satisfaction. A higher score indicates better sexual functioning.17 Scores of less than two on any item may be indicative of SD.
- •
Qualisex18,19 consists of 10 questions where 0 indicates not at all and 10 indicates very much so. The questionnaire is scored by averaging the results of the 10 questions, therefore a higher score denotes poorer quality of sexual life.
- •
Dermatology Life Quality Index (DLQI).20 One health domain the index explores refers to interpersonal relationships including sexuality. The higher the score, the greater the impact on the patient's quality of life.21
For statistical analysis, quantitative variables were summarised by their mean and standard deviation. Categorical variables were described by absolute and relative frequencies. Sociodemographic variables, comorbidities and PsA-specific variables were compared according to CSFQ-14, MGH-SFQ, Qualisex, and DLQI scores, where categorical variables were compared with each other using the χ2 statistic, and quantitative variables were compared with categorical variables (two or three groups) using an ANOVA if the applicability hypotheses were met or the Mann-Whitney U test otherwise. A linear regression model was used to assess the effect of sociodemographic variables, comorbidities, and variables specific to PsA on the results of the questionnaires. The applicability hypotheses were tested by checking the normality of the residuals of the model with the Shapiro-Wilk test and the homogeneity of variances by graphically observing the residuals of the model. Finally, a logistic regression model was used to analyse the effect of sociodemographic variables, comorbidities, and variables specific to PsA on the subjects’ SD. The goodness of fit of the model was tested with the Hosmer-Lemeshow test.
In both models, variables were selected stepwise, starting from a model without variables, introducing and eliminating them to minimise the Akaike information criterion (AIC), an algorithm that selects which model best explains the response variable (questionnaire score or sexual dysfunction). The significance level chosen for the analysis was α=.05.
The project met the ethical principles contained in the Declaration of Helsinki, including the Oviedo convention. The confidentiality of the data was respected at all times, through data anonymity in the database, in accordance with Royal Decree 1720/2007, enacting Organic Law 3/2018, of 5 December, on Personal Data and Guarantee of Digital Rights. The study protocol was approved by the Research Ethics Committee (REC) prior to its implementation.
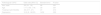
ResultsSeventy-eight patients were registered, of whom 72 agreed to answer the questionnaires. The demographic and clinical characteristics of the group are shown in Table 1. The employment status variable was reclassified: the levels ‘temporary work’ and ‘full-time work’ were merged into one level (work). ‘Poor’ and ‘very poor’ levels of perceived health were merged into the ‘poor’ level, and ‘very good’ and ‘good’ into ‘good’.
Baseline socio-demographic and clinical characteristics of the patients with PsA.
| Mean±SD | |
|---|---|
| Age | 52.2±10.9 |
| Number of children | 1.33±.904 |
| n (%) | |
| Women | 27 (37.5%) |
| Perceived health | Good 28 (38.89%) |
| Fair 36 (50%) | |
| Poor 8 (11.11%) | |
| Disease duration | ≤1 year 11 (14.67%) |
| 1–5 years 26 (36%) | |
| >5 years 35 (49.33%) | |
| Marital status | Married 48 (66.67%) |
| In a couple 12 (16.67%) | |
| Single 6 (8.33%) | |
| Divorced 6 (8.33%) | |
| Educational level | Primary 28 (38.89%) |
| Secondary 17 (23.61%) | |
| Baccalaureate or vocational training 15 (20.83%) | |
| University or doctorate 12 (16.67%) | |
| Employment status | Employed 47 (65.28%) |
| Unemployed 14 (19.44%) | |
| Retired 11 (15.28%) | |
| Annual household income | <16,000 є/year 13 (28.26%) |
| 16,000−24,000 є/year 21 (45.65%) | |
| 24,000−66,500 є/year 12 (26.09%) | |
| Psoriasis | 63 (87.5%) |
| Genital psoriasis | 23 (31.94%) |
| Axial involvement | 25 (34.72%) |
| Peripheral involvement | 69 (95.83%) |
| ATN | 31 (43.01%) |
| DL | 18 (25.35%) |
| DM | 4 (5.63%) |
| Smoking | 21 (29.33%) |
| Obesity | 19 (26.67%) |
| Treatment with glucocorticoids | 7 (9.72%) |
| Treatment with NSAIDs | 23 (31.94%) |
| Treatment with methotrexate | 41 (56.94%) |
| Treatment with anti-TNFα | 20 (27.78%) |
| Treatment with anti-IL17 | 8 (11.11%) |
| Other biologic treatments | 0 (0%) |
| History of depression | 8 (11.11%) |
| History of psychological treatment | 10 (13.89%) |
| History of psychiatric treatment | 11 (15.28%) |
anti-IL17: Anti-interleukin 17; anti-TNFα: Anti-tumour necrosis factor alpha; ATN: Arterial hypertension; DL: Dyslipidaemia; DM: Diabetes mellitus; NSAIDs: Non-steroidal anti-inflammatory drugs.
No significant differences were observed between sociodemographic variables, health perception, comorbidities, clinical variables of psoriatic disease, presence of Pso and genital Pso, frequency of axial and/or peripheral joint involvement, or disease-modifying treatments received by patients, according to gender.
Sexual functionTable 2 shows a descriptive summary of the scores of the questionnaires applied. It is worth noting the high percentage of patients with impaired sexual function according to the CSFQ-14 (45.33%). Significant differences in scores according to gender were observed in all the questionnaires to the detriment of women, except in the “personal relationships” domain of the DLQI.
Scores obtained in the sexual functioning questionnaires.
| Total score mean±SD | Women mean±SD | Men mean±SD | P-value | |
|---|---|---|---|---|
| MGH-SFQ | 11.71 (1.35) | 6.93 (6.52) | 14.76 (5.94) | .0001 |
| Qualisex total | 2.98 (.3) | 3.28 (2.72) | 2.75 (2.09) | .44 |
| DLQI total | 26.55 (.18) | 27.71 (3.45) | 24.73 (5.61) | .0083 |
| DLQI personal relations | 5.65 (.57) | 5.74 (1.0) | 5.48 (1.09) | .31 |
| CSFQ-14 total | 38.8 (.24) | 31.79 (11.32) | 43.66 (8.43) | < .001 |
| CSFQ-14 pathological | 45.33 (34) | 64.71 (22) | 35.29 (12) | < .001 |
| CSFQ-14 desire | 13.59 (.45) | 10.5 (4.42) | 15.86 (3.17) | <. 001 |
| CSFQ-14 arousal | 9.71 (.38) | 7.21 (3.27) | 11.5 (2.98) | < .001 |
| CSFQ-14 orgasm | 9.59 (.55) | 8 (3.22) | 10.5 (2.54) | < .001 |
| CSFQ-14 pleasure | 2.94 (.45) | 2.5 (1.2) | 3.25 (.84) | .0026 |
CSFQ: Changes in Sexual Functioning Questionnaire; DLQI: Dermatology Life Quality Index; MGH-SFQ: Massachusetts General Hospital-Sexual Functioning Questionnaire.
Values in bold indicate statistically significant results.
Question 10 of the CSFQ-14 scored a mean 2 (SD 1.05) for the women and 1.36 (SD .81) for the men, which means that loss of interest after arousal in the women was rare, as was priapism. Secondly, question 14 of the CSFQ-14 scored a mean 1.57 (SD .79) in the women and 1.18 (SD .39) in the men (P=.007), reflecting that orgasm never or rarely becomes painful. Finally, question 4 of the MGH-SFQ in males scored a mean of 3.07 (SD .2), equivalent to minimal to moderate altered sexual functioning associated with erection.
The patients with a family income of less than 16,000 euros per year scored significantly lower in the MGH-SFQ than the other groups (mean 6.92, SD 6.84, P=.037), and scored higher than the other groups in Qualisex (mean 4.76, SD 2.5, P=.017). Scores in the health group perceived as “poor” scored lower in the MGH-SFQ compared to the “good” group (mean 10.31 vs. 13.83 respectively, P=.049). No differences were observed in the means of the questionnaires according to marital status, number of children, level of education, employment status, physical exercise, or disease duration.
The comorbidities AHT and DL were significantly associated with lower scores in the CSFQ-14 and the orgasm and arousal domains, as was DL in the MGH-SFQ. Depression was associated with lower scores in the orgasm domain of the CSFQ-14 and the MGH-SFQ (P=.04 and .01, respectively). Finally, obesity was associated with lower scores in the arousal domain (P=.02) and in the arousal domain of the CSFQ-14 (P=.004).
Pso and genital Pso were associated with lower scores in the desire domain (P=.02) and the pleasure domain of the CSFQ-14 (P=.04).
The mean scores obtained in the CSFQ-14 questionnaires and the desire, arousal and orgasm domains were significantly higher in the patients treated with NSAIDs.
Effect of sociodemographic variables, comorbidities, and psoriatic diseaseAnalysis of the effect of the variables studied on the questionnaire scores is shown in Table 3.
summary of multiple linear regression model relating the questionnaire scores to the variables studied.
| Variables | b coefficient | Standard error | P-value |
|---|---|---|---|
| CSFQ-14 | |||
| Sex: male | 12.37 (7.56, 17.18) | 2.39 | < .001 |
| Age | −.24 (−.35, −.14) | .054 | < .001 |
| Dyslipidaemia | −9.98 (−17.4, −2.57) | 3.68 | .009 |
| CSFQ-14 desire | |||
| Sex: male | 5.83 (3.4, 7.67) | .91 | .001 |
| Household income/year | −.99 (−1.96, −.01) | .48 | .047 |
| Dyslipidaemia | −3.76 (−6.6, −.94) | 1,4 | .01 |
| NSAIDs | 2.96 (.76, 5.16) | 1,09 | .01 |
| CSFQ-14 pleasure | |||
| Sex: Male | .78 (.21, 1.35) | .28 | .008 |
| CSFQ-14 arousal | |||
| Sex: male | .29 (2.77, 5.82) | .76 | < .001 |
| Dyslipidaemia | −3.05 (−5.4, −.70) | 1.16 | .012 |
| CSFQ-14 orgasm | |||
| Sex: male | 2.81 (1.42, 4.19) | .69 | < .001 |
| Dyslipidaemia | −2.64 (−4.77, −.51) | 1.06 | .016 |
| Depression | −2.61 (−5.05, −.17) | 1.21 | .036 |
| Qualisex | |||
| Dyslipidaemia | 2.37 (.62, 4.13) | .87 | .009 |
| MGH-SFQ | |||
| Sex: male | 7.06 (3.89, 10.24) | 1.58 | < .001 |
| Dyslipidaemia | −5.17 (−10.05, −.3) | 2.42 | .038 |
| Depression | −6.56 (−12.19, −.93) | 2.8 | .023 |
| DLQI personal relationships: no associations were observed | |||
Only significant results are shown.
CSFQ: Changes in Sexual Functioning Questionnaire; DLQI: Dermatology Life Quality Index; MGH-SFQ: Massachusetts General Hospital-Sexual Functioning Questionnaire.
The following was deduced from the results obtained:
- •
CSFQ-14: the men scored a mean 12.37 points higher than the women. Patients with DL scored a mean 9.98 points lower.
- •
CSFQ-14 desire: the men scored a mean 5.83 points higher than the women. Patients with lower annual household income scored a mean .99 points lower, those with DL scored a mean 3.76 points lower, and those receiving NSAID treatment scored a mean 2.96 points higher than the untreated patients.
- •
CSFQ-14 arousal: the men scored a mean 4.29 points higher than the women. Patients with DL scored a mean 3.05 points lower.
- •
CSFQ-14 orgasm: the men scored a mean 2.81 points higher than the women. Subjects with DL scored a mean 2.64 points lower, and those with depressive problems scored a mean 2.61 points lower.
- •
CSFQ-14 pleasure: the men scored a mean .78 points higher than the women.
- •
MGH-SFQ: the men scored a mean 7.06 points higher than women. Patients with depression scored a mean 6.56 points lower, and those receiving NSAID treatment scored a mean 5.74 points higher than the untreated patients.
- •
Qualisex: Patients with DL scored a mean 2.37 points higher, which translates into poorer sexual function.
Finally, the relationship between the SD of the patients was determined according to the variables studied (Table 4). From this model it was possible to determine:
- •
The odds ratio (OR) of having SD among the women was 18.54 times higher than in the men.
- •
For each one-year increase in age, a subject’s OR of having SD increased by 10%.
- •
The patients treated with NSAIDs had an OR of less likelihood of SD of 16.67.
- •
The subjects with depression had a 10.9-fold greater OR of having SD.
Logistic regression model relating SD to the variables studied.
| Pathological CSFQ | Odds ratio [95% CI] | Standard error | P-value |
|---|---|---|---|
| Sex: male | .05 (.01, .16) | .66 | .001 |
| Age | 1.11 (1.05, 1.19) | .03 | .031 |
| Treatment with NSAIDs | .06 (.017, .47) | .07 | .013 |
| Depression | 10.9 (.8, 148.33) | 14.52 | .032 |
CSFQ: Changes in Sexual Functioning Questionnaire; NSAIDs: Non-steroidal anti-inflammatory drugs SD: Sexual dysfunction.
There is little evidence on the difficulties experienced by patients with PsA in their sexual life. We conducted this original, descriptive, analytical, and comparative study to learn more about sexual health in this group. Our results show that nearly half of the patients with PsA presented some degree of altered sexual function, which should alert us to the magnitude of the problem. Previous studies in patients with pathologies such as RA or Pso have shown that these patients are at higher risk of altered sexual function compared to healthy individuals.8,12,22,23 Inflammatory disease may not be the only cause, but the presence of other comorbidities such as psycho-affective disorders or cardiovascular risk factors probably increase the risk.12,22 The data observed in the present study are consistent with the results of other publications in patients with Pso,8,12,24 which show that SD in patients with PsA is multifactorial and probably attributed to chronic organic and psychological damage.
Among the characteristics associated with SD, age is a very important biomarker in both women and men, as in the general population and in patients with chronic diseases.25,26 It has also been associated with worse scores on the CSFQ and its domains, and with the MGH-SFQ, results similar to those published in previous studies. However, Qualisex was not determined by this biomarker, a fact already described in the process of its development and validation.18
The second most important biomarker of SD is female sex, as observed in the studies conducted in the general population by McCabe et al.9,10 The proportion of studies conducted on sexuality and Pso in which men predominate in relation to women with Pso is striking, perhaps because it is assumed that penile involvement is more severe than vulvar involvement, or for cultural reasons. After evaluating our results, we can state that PsA significantly affects all dimensions of sexual function, and more markedly so in women. This phenomenon occurs partially in the general population and there are differences between genders, where premature ejaculation and erectile dysfunction are more frequent in men, and in women there is a lack of sexual interest, inability to reach orgasm, and lubrication difficulties.9,10
Of the socio-demographic markers, it is worth mentioning the significant association between a low level of income and the desire domain. These data reflect a situation also described in the general population where SF is determined by the degree of development of the country of residence.27
In a patient with a chronic disease, the accumulation of other organic and psycho-affective risk factors may be determinants of SD.12,24 We observed that the results of SF questionnaires are globally determined by the biomarkers age and gender, together with patient comorbidities and the treatments used for their disease. Dyslipidaemia, not other cardiovascular risk factors, is predominantly associated with worse SF rates. This result is important to highlight because it has not been specifically studied to date. Therefore, surveillance and even treatment of cardiovascular risk factors may have a positive outcome not only in preventing premature deaths, but also in improving SF.
Alterations in the psycho-affective sphere, such as depression or anxious-depressive syndrome, are present in our population in 12% of cases, similar to that observed in other series of patients with PsA, where this emotional disorder has been found in around 14%–17%.28 Emotional disorders in patients with PsA have been associated with a higher risk of SD7,12,24 and in our study they were shown to be associated with SD in the orgasm domain of the CSFQ-14, and the MGH-SFQ score, and therefore the quality of sexual relations in these patients may be affected. This is similar to the results found by the group of Mercan et al.29 where the orgasmic experience was worse in patients with PsA than in controls. In this sense, rheumatologists should pay more attention to patients with cardiovascular and psycho-affective comorbidities, because this patient profile is more likely to suffer from a sexual disorder.
We were able to determine that the presence of Pso in PsA is also associated with worse SF, regardless of its location, in contrast to numerous previous studies that describe the association between genital Pso and SD.12,18,24 A reason for this difference may be the emotional impact of having more extensive disease, with skin and joint involvement and associated comorbidities, which are determining factors in overcoming two major obstacles for the patient: concern whether it may cause their sexual partner to reject them, and secondly, whether the joint involvement will limit performance of the sexual act. In short, the psoriatic disease will determine the patient's experience.
Finally, treatments used for psoriatic disease control chronic inflammation, pain, and associated morbidity. Specifically, the use of NSAIDs acts as a protective factor on sexual health, probably associated with the beneficial effect of symptom control.
Of the questionnaires used, the CSFQ-14 offers the most information on sexual health and allows for a broad study of sexuality, and therefore we believe to be the questionnaire of choice for inclusion in the rheumatology consultation. The therapeutic approach to patients diagnosed with SD remains to be determined, as currently most rheumatology practices do not have a psychology service that meets this need, therefore we believe that patients should be referred to an external psychology office.
Our study has several limitations. It does not collect information on menopausal status in women of a mean age above 51, the mean age of menopause in Spanish women.30 This factor was not directly considered.
We did not collect data on PsA activity, a variable that would have allowed us to compare the sexual health of patients in remission or with low disease activity with those not in that situation.
Finally, we did not have a group of healthy controls to compare the two populations, as the primary objective was to describe the presence of alterations within the pathology under study, despite the fact that the CSFQ-14 questionnaire has a cut-off point that allows SD to be diagnosed. However, after evaluating the results, we plan to conduct a case-control study in the near future.
In conclusion, these are patients with PsA presenting overall deterioration in SF, they are primarily women, older, with low income, and DL, where the psychological burden of a chronic disease behaves as a factor favouring SD and where anti-inflammatory treatments have a beneficial effect on sexuality.
FundingThis study was awarded the “Beca de Ayuda a la Investigación en Reumatología 2021”, supported by the Fundación Valenciana de Reumatología, Spain.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all the patients who agreed to participate in the study.