Sarcoidosis is a chronic, multisystemic, granulomatous disorder. Our patient was a 2-year-old girl with multiple airway conditions and a partial response to inhaled and systemic steroids. She was positive for acute phase reactants and negative for antibodies. Polymerase chain reaction revealed atypical Mycobacteria and she was negative for Mycobacterium tuberculosis. Laryngeal sarcoidosis was diagnosed by histopathology in a biopsy of larynx that revealed a chronic granulomatous inflammatory process with Langhans giant cells and acute and ulcerated areas with changes compatible with tuberculosis. Treatment consisted of monthly gammaglobulin for 6 months at doses of 2g/kg body weight, accompanied by Valmetrol™ and methotrexate. Immunomodulation with gammaglobulin was prescribed, with subsequent use of methotrexate-based immunosuppression. Currently, bronchoscopy shows no evidence of granulomas and she is negative for acute-phase reactants.
La sarcoidosis es un trastorno crónico, multisistémico y granulomatoso. Femenina de 2 años con múltiples cuadros de vías respiratorias, con esteroides inhalados y sistémicos presentando respuesta parcial, reactantes de fase aguda positivos, anticuerpos negativos, además de PCR de micobacterias atípicas con Mycobacterium tuberculosis negativa. Se diagnostica de sarcoidosis laríngea por histopatología biopsia de laringe con proceso inflamatorio crónico granulomatoso con células gigantes tipo Langhans, y áreas agudizadas y ulceradas con cambios compatibles con proceso fímico. Se inicia tratamiento con gammaglobulina mensual durante 6 meses a dosis de 2g/kg/peso, Valmetrol® y metotrexate. Se decidió la inmunomodulación con gammaglobulina y con posterior uso de inmunosupresión a base de metotrexate. Actualmente broncoscopia sin evidencia de granulomas y reactantes de fase aguda negativos.
Sarcoidosis is a chronic, multisystemic and granulomatous disorder with an incidence of .22–.27 per 100,000 children per year. Involvement of the larynx is described less frequently, and represents .33%–2.1% of cases.1
Diagnosis is established by histological evidence of non-caseous granulomas in affected tissue, as well as exclusion of other granulomatous diseases such as tuberculosis, histoplasmosis, blastomycosis. It is characterised by the formation of non-necrotising epithelioid cell granulomas as a result of underlying immune deregulation, and there is typically multiorgan involvement.2 Laryngeal sarcoidosis, a rare extrapulmonary manifestation of sarcoidosis, occurs infrequently as a complication of complete airway obstruction.3 The estimated incidence of laryngeal involvement in patients with sarcoidosis ranges from 1% to 5%.4 Initial clinical presentation includes fever, weight loss, fatigue, bone and joint pain, anaemia, hepatomegaly and lymphadenopathy.5 In children under 5 years old, skin, eyes and joints are affected, whereas in older children, involvement of the lungs, lymph nodes and eyes predominates.6 Several treatment modalities are reported for laryngeal sarcoidosis, including systemic corticosteroids, intralesional corticosteroid injection, and surgical removal.7
Aim: Presentation of a case of sarcoidosis in a child.
Clinical observationA 2-year-old female who started with viral croup, with multiple respiratory tract symptoms, under treatment with inhaled and systemic steroids with partial response.
No significant family history, incomplete vaccination schedule and no other pathological signs.
The diagnostic approach involves a search for infectious aetiology which might predispose to an inflammatory state. General laboratory data with normal parameters, acute phase reactants ESR maximum peak of 63mm/h, negative antibodies in addition to PCR of atypical mycobacteria with negative Mycobacterium tuberculosis (Table 1) and chest X-ray (Fig. 1) are requested.
Laboratory results.
| Studies undertaken | One month | 3 months | 6 months | 9 months |
|---|---|---|---|---|
| Erythrocyte sedimentation rate | 12mm/h | 63mm/h | 21mm/h | 6mm/h |
| Polymerase chain reaction | 0mg/dl | .043mg/dl | .098mg/dl | .024mg/dl |
| Antineutrophil cytoplasm antibodiesProteinase | Negative | Negative | ||
| Neutrophil perinuclear antibodyMyeloperoxidase | Negative | Negative | ||
| Antinuclear antibody-HEp-2 | Negative | Negative |
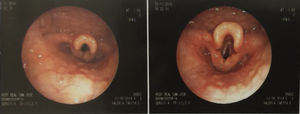
During the child's hospital stay she underwent endoscopy (Fig. 2) and laryngeal biopsy with histopathological report of chronic inflammatory granulomatous process with Langhans giant cells and acute and ulcerated areas with changes compatible with phymic process, resulting in a diagnosis of laryngeal sarcoidosis. Infectious granulomatous diseases, principally Mycobacterium tuberculosis, were ruled out by negative PCR. Management with monthly gamma globulin was initiated with doses of 2g/kg body weight. Valmetrol® 3 tablets every 24h.
Methotrexate at 15mg/m2/SC weekly. Steroids were not used because the patient had been refractory since the onset of symptoms. Follow-up was offered with bronchoscopy with no evidence of negatively reacting granulomas. The patient continues with methotrexate management at 15mg//m2/SC weekly, and folic acid 5mg/24h from Monday to Thursday.
DiscussionDiagnosis is based on a compatible clinical and radiographic picture, supported by histological evidence of non-caseous granulomas in affected tissue, and ruling out other granulomatous diseases. The condition is characterised by the formation of granulomas as a result of underlying immune dysregulation, and there is typically multiorgan involvement. Although early childhood sarcoidosis is manifested by the triad of skin rash, arthritis and uveitis, there are different forms of presentation in children, like our case, with signs of pulmonary involvement. FDG-PET/CT can be used to assess inflammatory activity accurately in patients with persistent symptoms and without biological inflammatory activity, especially in rare locations or when biopsy is not possible.8
ConclusionsIn this patient in particular and due to her age, immunosuppression as referred to in different management protocols was not possible. In addition, she had failed to respond to high doses of steroids; therefore immunomodulation with gamma globulin and then immunosuppression based on methotrexate were decided to maintain control of her baseline disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing has been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Vega-Cornejo G, Ayala-Buenrostro P. Sarcoidosis laríngea infantil: presentación de un caso clínico. Reumatol Clin. 2019;15:e102–e104.