Isolated extrapulmonary involvement in sarcoidosis is uncommon and reported in 5–9% of systemic sarcoidosis, this constitutes a clinical challenge due to its extensive differential diagnosis. Extrapulmonary sarcoidosis affecting more than three organs is rarely reported and there are scarce literature data published on diagnosis, clinical course and management in those cases.
We hereby discuss a case of a 41-year-old female with systemic non-pulmonary sarcoidosis affecting lacrimal gland, peripheral lymph nodes, parotid gland and the liver.
La afectación extrapulmonar aislada en la sarcoidosis es infrecuente y se reporta en el 5 al 9% de las sarcoidosis sistémicas, lo que constituye un desafío clínico debido a su extenso diagnóstico diferencial. La sarcoidosis extrapulmonar que afecta a más de tres órganos es raramente reportada y hay pocos datos publicados sobre el diagnóstico, la evolución clínica y el manejo de estos casos. Presentamos el caso de una mujer de 41 años con sarcoidosis sistémica no pulmonar que afecta a la glándula lacrimal, los ganglios linfáticos periféricos, la glándula parótida y el hígado.
Sarcoidosis is a chronic, idiopathic multisystemic granulomatous disease. The incidence varies widely throughout the world, probably because of differences in environmental exposures, predisposing HLA alleles and other genetic factors. The higher incidence has been observed in northern European countries and the adjusted annual incidence among black Americans is approximately three times that among Caucasian Americans, with a preponderance of cases in females across racial and ethnic groups.1,2
Sarcoidal granulomas can involve any organ, but in more than 90% of patients is manifested as intrathoratic lymph-node enlargement and pulmonary involvement.1 Extrapulmonary organ involvement occurs in up to 50% of patients, while only 5–9% have extrapulmonary disease without pulmonary sarcoidosis.3 In regards to specific organ involvement, the non-pulmonary sarcoidosis patients have a higher prevalence of skin involvement (49.3%) in comparison to those with pulmonary sarcoidosis (25%). After skin, the distribution by organ involvement in those patients with non-pulmonary sarcoidosis is eye (23.6%), liver (20.7%), extrathoracic lymph-node (13.7%), parotid/salivary (5.7%) and bone/joint (1.4%).3
Criteria for diagnosing systemic sarcoidosis require symptoms showing the involvement of at least two organ systems, supporting histology and valid exclusion of other granulomatous disease.1
Multi-organ involvement in non-pulmonary sarcoidosis affecting more than three organs are rarely reported and constitute a clinical challenge. There are scarce literature data published on diagnosis, clinical course and management in those cases.
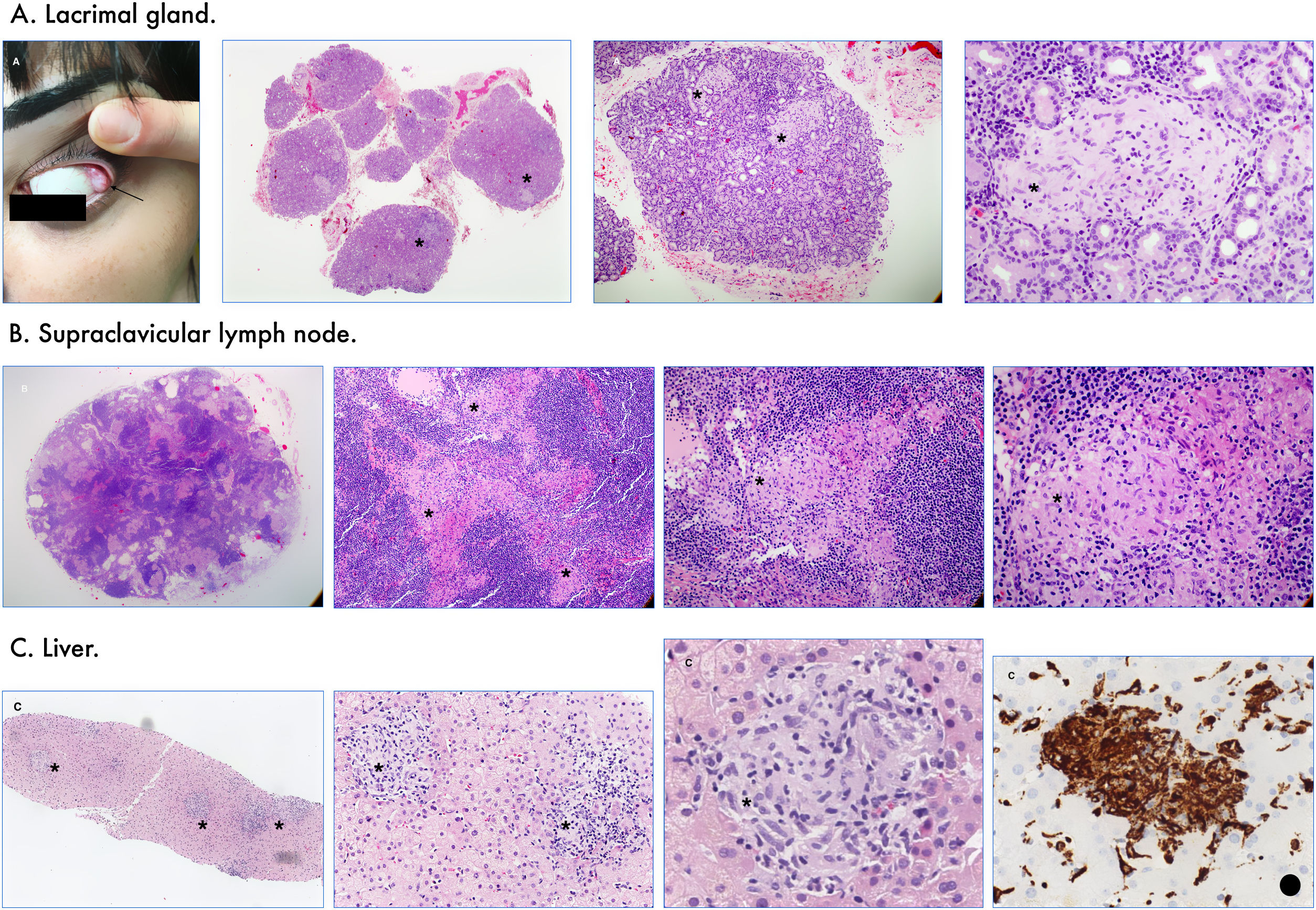
Case presentationA 41-year-old Turkish woman, was referred to our department presenting severe asthenia, xerophthalmia, xerostomia, inflammatory arthralgias and recurrent bilateral parotid enlargement. On physical examination, the eversion of the upper eyelids showed a lacrimal gland enlargement (Fig. 1A, arrow). Supraclavicular lymph nodes were enlarged as well and palpable. There were no skin lesions at any anatomical area. The initial blood test showed an increase in C-reactive protein of 1.03mg/dL (<0.5mg/dL) associated to elevated liver enzymes with a total bilirubin of 0.5mg/dL (0.2–1.2mg/dL), AST/GOT 56IU/L (0–32IU/L), ALT/GPT 75IU/L (0–33IU/L), GGT 112IU/L (5–36IU/L), alkaline phosphatase 157IU/L (35–104IU/L). No alteration of the cell count or hypergammaglobulinemia were observed. Infectious serologies including the most prevalent viral, bacterial and fungal entities were negatives. Antinuclear, anti-SSA/Ro, antineutrophil cytoplasmic, anti-myeloperoxidase and anti-proteinase 3 antibodies were all negatives. A computed tomography (CT) of the thorax and abdomen was performed to rule out malignancy. The thoracic CT scan did not show pulmonary parenchymal abnormalities and neither mediastinal or hilar lymphadenopathy. The abdominal CT scan showed enlarged periceliac and periportal lymph nodes without hepatomegaly. A lacrimal gland and supraclavicular lymph node biopsy were performed showing confluent epithelioid granulomas without necrosis (Fig. 1A and B*). On suspicion of sarcoidosis with involvement of the lacrimal glands and peripheral lymph nodes, systemic corticosteroids (GC) were initiated at a dose of 0.5mg/kg/day, gradually taper during the following eight months to a maintenance dose of 15mg/day. During the follow-up and once the patient finished the systemic GC therapy, isolated hepatic progression was observed with progressive and worsening of the liver function tests characterized by dissociated cholestasis and cytolysis. Thus, an hepatic biopsy was performed which supported the diagnosis of hepatic sarcoidosis (Fig. 1C). A new course of systemic GC was initiated at 1mg/kg/day gradually taper during the following ten months with fluctuation of the liver enzymes showing a mild dissociated cholestasis without cytolysis and with no hepatic sign or symptoms of disease progression.
Discussion and conclusionSarcoidosis is a granulomatous systemic autoimmune disease of unknown and probably multifactorial aetiology; whose typical histopathological finding is the presence of non-necrotizing granulomas. Its prevalence is estimated between 0.02 and 0.14%, being more prevalent in Nordic countries and African-Americans.1,2 In addition, sarcoidosis occurrence varies greatly by age and gender with a peak age of onset closer to 30–55 years-old, earlier in men than in women.2,4 The difference in age between gender at diagnosis suggests that could be related to genetic factors or environmental exposures, although what causes this variation is unknown.2
Between 5 and 9% of patients with sarcoidosis have isolated extrapulmonary disease without pulmonary involvement.3,5 According to the affected organ, ocular involvement is found in 23.6%, parotid/salivary gland in 5.7%, hepatic involvement in 20.7% and extrathoracic lymphadenopathy in 13.7% of the patients with non-pulmonary sarcoidosis.3
We report an uncommon presentation of non-pulmonary sarcoidosis with multi-organ involvement (lacrimal gland, peripheral lymph nodes and liver). To our knowledge, this is the first reported case of non-pulmonary sarcoidosis involving hepatic, lymph nodes and lacrimal gland at the same time. In addition, our patient presented bilateral parotid gland enlargement; however, the biopsy was avoided to prevent iatrogenesis. After a careful diagnostic work-up, infectious agents, drug-induced hypersensitivity, connective tissue diseases such as vasculitis and Sjögren syndrome, primary immunodeficiencies and sarcoid-like reaction to malignancy were excluded.
In our case, the prognosis of the disease will be marked by the liver therapeutic response. The therapeutic approach for hepatic involvement should be focus in avoiding disease progression and hepatic complications. The first-line treatment is based on systemic GC; however, some patients have not a complete clinical response.6 Alternative agents, such as methotrexate, despite the potential risk of hepatotoxicity has showed improve in the liver function test abnormalities and also, it is helpful as corticosteroid sparing.6,7
The relative infrequency of sarcoidosis, accompanied by its wide clinical heterogeneity, leads to a complex diagnostic process that poses a great challenge in routine clinical practice.
Conflict of interestAll named authors declare that they have no conflict of interest to disclose.
We are thankful to Dr. Naranjo from de Department of Anatomical Pathology for their help in the preparation of the histological sections for the presented case. Also, we thank to Juan Vilches for assistance in technique support.