We report the case of a 64-year-old woman with rheumatoid arthritis and Sjögren's syndrome, treated during 48 months with hydroxychloroquine that was removed after an ophthalmological evaluation showed bilateral vision loss associated with paracentral scotoma in the visual field, fundoscopic macular pigmentary changes, and severely impaired central multifocal electrorretinogram (mfERG). Twelve months after treatment withdrawal, visual acuity and central mfERG had surprisingly improved. This is an unusual case of functional recovery after treatment withdrawal. We consider that central mfERG is a more sensitive test than pattern electrorretinogram in the detection of retinal toxicity and functional vision recovery after hydroxychloroquine treatment cessation.
Presentamos un paciente de 64 años, del sexo femenino, con artritis reumatoide y síndrome de Sjögren, tratada durante 48 meses con hidroxicloroquina, a la que se le suspendió dicho tratamiento tras una revisión oftalmológica, en la que se detectó pérdida de la visión en ambos ojos asociada a defecto campimétrico paracentral, alteraciones fundoscópicas maculares pigmentarias y electrorretinograma multifocal (ERGmf) central disminuido en ambos ojos. A los 12 meses de la retirada del tratamiento, la agudeza visual y el ERGmf central habían mejorado sorprendentemente. Se trata de un caso inusual de recuperación funcional tras la retirada del tratamiento. Consideramos que el ERGmf central es una prueba más sensible que el electrorretinograma patrón en la detección de toxicidad retiniana y en la detección de mejorías visuales funcionales tras la retirada del tratamiento con hidroxicloroquina.
The irreversible loss of visual function caused by the toxicity of antimalarials, and even subsequent deterioration despite discontinuation of therapy, has been known for many years and currently there is still a running series of cases that corroborate it.1 There are no reported cases of visual improvement after discontinuation of therapy with hydroxychloroquine, although we have found an isolated case of slight improvement in the electroretinogram2 (ERG). We describe a patient whose visual function considerably improved after detection of toxicity and immediate discontinuation of therapy. This case had some good prognostic factors, such as a low cumulative dose of hydroxychloroquine and early detection of ocular toxicity, something that could be taken into account.
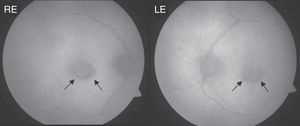
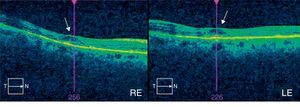
Clinical CaseThe patient was a 64-year-old woman being treated for rheumatoid arthritis, who had ingested a cumulative total dose of 112g of hydroxychloroquine at a rate of 400mg daily for the first 60 days and 200mg daily for the remaining 1380 days. She had a history of chronic liver disease, so was undergoing semi-annual follow up visits in our ophthalmology department since the start of treatment. At the time of diagnosis of antimalarial maculopathy, she exhibited a 0.7 best corrected visual acuity in both eyes. Perimetry showed bilateral paracentral scotoma and fundoscopy observed concentric hypopigmentation and hyperpigmentation appreciated in both macula, most evident in the retinography with autofluorescence (Fig. 1). The optical coherence tomography (OCT) image showed characteristic “flying saucer” lesions in both eyes (Fig. 2) and the central multifocal electroretinography (ERGmf) appreciated a decrease in amplitude, definition and density of electrical waves (Fig. 3A). We immediately suspended hydroxychloroquine treatment and the patient was started one tablet daily of a complex of antioxidants and vitamins, usually employed in macular degeneration associated with age. An ERGmf at 12 months after the discontinuation of therapy detected a surprising improvement (Fig. 3B) with an increase in the amplitude of the central hexagon of 67% in the right eye and 104% in the left. Similarly, the amplitude ratio between the central and pericentral ring, increased from 1.2 to 2.3 in the right eye and 1.9 to 3.1 in the left. The defective resolution of ERGmf waves obtained at the time of detection of the antimalarial maculopathy (Fig. 3A) prevents a reliable determination of the implicit times and their comparison with the record made after one year. The improvement was reflected in a recovery of best corrected visual acuity in the right eye, with maintenance of vision in the left eye at 0.7. The fundus images and the “flying saucer” lesions on the OCT were not modified.
Hydroxychloroquine retinal toxicity is very rare when the drug is taken at low doses. It is considered that the risk is low during the first 5 years in individuals who take a dose inferior to 3mg/kg/day, except when there is concomitant nephropathy, liver disease or low body mass.3 When it occurs, the toxic effect is considered irreversible, but what is unique in our patient is that she presented improvement in visual function after treatment suspension. To analyze and document this case we paid special attention to the central ERGmf, which is the test that provides more detailed and objective information.4 For the differential diagnosis with other macular diseases we have relied on OCT (Cirrus, Carl Zeiss) ruling other causes of maculopathy out and documenting the characteristic “flying saucer” image of maculopathy, so far unique to this disease.
We emphasize the utility of central ERGmf in the early detection of functional visual changes due to antimalarials toxicity compared to traditional ocular electrophysiological testing. The ERGmf, under the conditions in which it was performed, detects associated cone and bipolar cell abnormalities, while the ERG pattern localizes it to the inner retina, especially ganglion cells.
This cloroquinic maculopathy was detected after 48 months of hydroxychloroquine treatment at normal doses, which can be considered a relatively early toxicity, probably due to a history of chronic liver disease. We believe that visual recovery was mainly due to the early withdrawal of the drug. Antioxidants used in treating macular degeneration are unlikely to have had some beneficial role.5
ConclusionsFunctional visual recovery may occur in cases of retinopathy due to antimalarials if detected early. The central ERGmf is the most sensitive test for early detection and to assess early signs of functional recovery.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors state that no patient data appears in this article.
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Rodríguez-Hurtado FJ, Sáez-Moreno JA, Rodríguez-Ferrer JM. Toxicidad ocular y recuperación visual funcional en una paciente tratada con hidroxicloroquina. Reumatol Clin. 2015;11:170–173.