To calculate the prevalence and describe the main demographic characteristics of Sjögren's syndrome in adults in Colombia.
Material and methodsDescriptive cross-sectional study which utilised data from the Integral Information System of Social Protection of the Ministry of Health of the Republic of Colombia during the years 2012 to 2016.
Results58,680 cases of Sjögren's syndrome were identified, with a prevalence in those over 18 years of age of 0.12%; 82% were women, with a female:male ratio of 4.6:1, with a higher prevalence in the age group of 65–69 years. The departments with the highest numbers of cases were Bogotá DC (24,885), Antioquia (9040) and Valle del Cauca (5277); however, the departments with the highest prevalences were Caldas (0.42%), Bogotá DC (0.32%) and Antioquia (0.14%).
ConclusionsWe present demographic and epidemiological information on Sjögren's syndrome in Colombia. There are very few epidemiological studies of this disorder. However, a prevalence similar to that reported in countries of the region such as Brazil (0.17%) and Argentina (0.17%) was documented.
Calcular la prevalencia y describir las principales características demográficas del síndrome de Sjögren en Colombia.
Material y métodosEstudio descriptivo de corte transversal en el que se tomaron los datos del Sistema Integral de Información de la Protección Social del Ministerio de Salud de Colombia, durante los años 2012 a 2016.
ResultadosSe identificaron 58.680 casos, calculándose una prevalencia en mayores de 18 años de 0,12%. El 82% son mujeres, con una relación mujer:hombre de 4,6:1, con prevalencia mayor entre el grupo etario de 65 a 69 años. Los departamentos con mayor número de casos son Bogotá DC (24.885), Antioquia (9.040) y Valle del Cauca (5.277), sin embargo, los departamentos con mayor prevalencia fueron Caldas (0,42%), Bogotá DC (0,32%) y Antioquia (0,14%).
ConclusionesSe presenta información demográfica y epidemiológica del síndrome de Sjögren en Colombia. Existen muy pocos estudios epidemiológicos de esta enfermedad, sin embargo, se documentó una prevalencia similar a la reportada a países de la región como Brasil (0,17%) y Argentina (0,17%).
Sjögren's syndrome (SS) is a chronic autoimmune epithelitis characterised by lymphocytic infiltration of the salivary and tear glands as well as other exocrine glands. It causes dryness of the skin and mucosa, especially in the eyes and mouth, together with the circulation of antinuclear antibodies against extractable nuclear antigens in a high proportion of patients, specifically SS-A (anti Ro) and SS-B (anti La).1 The disease involves mechanisms which lead to tear and salivary gland inflammation and B lymphocyte hyperactivity. It is the result of a complex interaction between genetic and environmental factors that give rise to immune tolerance alteration and exocrine gland inflammation. SS is heterogeneous in terms of its clinical expression and severity, which involves different pathogenic pathways in patient subgroups.2 Epidemiological studies link rheumatological clinical practice to society, making it possible to establish an overview of the frequency and clinical and demographic characteristics of the disease, so that preventive, therapeutic and rehabilitation work can be targeted. This work seeks to establish the prevalence of SS in Colombia and describe the basic demographic characteristics of the patients with this disease.
Material and methodsThis is a descriptive and transversal study based on information from the Social Protection Integrated Information System (SISPRO) of the Ministry of Health of Colombia. The demographic information available in the Individual Registry of Service Supply to patients diagnosed SS (code CIE 10 M350) from 2012 to 2016 was used. Five-year groups were used to calculate prevalence in Colombia, as well as analysis of each one of the 32 Departamentos during the five-year period analysed, evaluating the population according to projections by the National Administrative Department of Statistics, based on the data of the last national census in the year 2005.3 Subsequently a description of the resulting data was created in terms of frequencies and a percentage for qualitative variables. This work was approved by the Clinical Research and Ethics Committee of the Pontificia Universidad Javeriana, Bogotá, Colombia.
ResultsIn the period from 1 January 2012 to 31 December 2016 58,680 cases were identified, giving a total prevalence of .12%, with a female to male ratio of 4.63:1 respectively. The prevalence of SS among women amounted to 0.31%, while for men it stood at 0.07%. The age group in which prevalence was highest corresponded to those aged 65–69 years old (.5%) (Table 1). In the analysis according to Departamento the highest numbers of cases were recorded in Bogotá DC (24,885), Antioquia (9040) and Valle del Cauca (5277). Likewise, the Departamentos with the highest prevalence were Caldas (.42%), Bogotá DC (.32%) and Antioquia (.14%).
Prevalence of Sjögren's Syndrome according to age group in Colombia from 2012 to 2016.
| Age group | Total patients | Prevalence |
|---|---|---|
| 0–4 | 513 | .012 |
| 5–9 | 550 | .013 |
| 10–14 | 627 | .015 |
| 15–19 | 877 | .020 |
| 20–24 | 1470 | .035 |
| 25–29 | 2053 | .053 |
| 30–34 | 3054 | .088 |
| 35–39 | 3654 | .116 |
| 40–44 | 4438 | .154 |
| 45–49 | 6214 | .217 |
| 50–54 | 8232 | .316 |
| 55–59 | 8707 | .408 |
| 60–64 | 7751 | .466 |
| 65–69 | 6280 | .502 |
| 70–74 | 4183 | .465 |
| 75–79 | 2834 | .422 |
| 80 or over | 2136 | .319 |
| Total | 58,680 | .12 |
Prevalence is calculated by dividing the total number of patients per age group in the average population of the period per age group as the denominator×100 inhabitants.
Epidemiological studies are essential to describe the burden of this disease on society and to clarify any possible factors associated with its aetiology. SS is one of the most common autoimmune conditions, with an estimated worldwide prevalence within a range from .05% to 4.6%.4,5 The results of prevalence studies of SS are heterogeneous because of the different classificatory criteria used in each study and the different geographical areas and ethnic populations in which they were performed.6,7 The disease occurs more frequently in women, with a ratio of up to 1:10 in comparison with men, and it mainly manifests in the decades of life from 40 to 70 years old, corresponding to women in peri- and postmenopausal ages.8 The incidence of SS in patients with rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis has been estimated to stand at 17.1%, 8%, 20% and 14%, respectively.9 The prevalence of polyautoimmunity among patients with SS was evaluated in a Colombian population of 410 patients, among whom it was found to coexist with rheumatoid arthritis (8.3%), systemic lupus erythematosus (7.6%), antiphospholipid syndrome (2.6%), systemic sclerosis (1.4%) and vasculitis (1.1%).10
Table 2 shows prevalence data from around the world according to region.8,11–13 There have been very few epidemiological or prevalence studies of SS in Latin America. An initial prevalence study was conducted in Brazil in 2013, reporting a prevalence of .17%.14 Three years later, in Argentina, the same percentage of prevalence was obtained in a study using COPCORD methodology in an indigenous population in the province of Rosario.15 In Colombia, the same methodology was used to survey 3146 men and 3547 women over 18 years old, recording a prevalence of SS of .08% in the first preliminary report from this study.16 The higher rate of involvement of the female sex is similar to that reported by other studies, and likewise a concentration of patients was recorded in older age groups (65 to 69 years old). More recently reported prevalence studies generally find lower rates than those in earlier studies, and this may be the result of increased rigour in the latest epidemiological studies, selection distortions and the small sample sizes in previous studies.17 SS prevalence data in Latin America exist for high complexity hospitals, as is the case in Mexico. In a population of 300 patients corresponding to rheumatology and internal medicine clinics of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, the prevalence of SS is estimated to stand at 13.3% (CI 95%: 9.5%-17.1%).18 It is important to have SS prevalence studies in Latin America, given that patients in our region may show differences in its manifestation and subphenotypes in comparison with patients from other latitudes or ethnic groups. This was demonstrated by a study which included 8310 patients with SS in 20 countries in 5 continents. It found that patients in South America showed alterations more frequently in ocular evaluation tests (the Schirmer and Rose Bengal tests) as well as positivity in the results of salivary gland biopsy in comparison with North American patients. Nevertheless, they show lower positivity for rheumatoid factor, antinuclear antibodies, anti Ro and anti La antibodies, as well as lower C4 consumption.19 In the same way different responses to treatment are also possible, as well as in terms of the harm accumulated over time, as was shown in a cohort of 377 patients with SS in 3 Latin American countries. In these patients the use of antimalerial drugs was found to be a possible protective factor against accumulated harm due to the disease, especially in terms of pleuro-pulmonary involvement.20
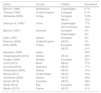
Prevalence of Sjögren's Syndrome in different countries of the world.
| Author | Country | Criteria | Prevalence |
|---|---|---|---|
| Bjerrum (1989) | Switzerland | Copenhagen | 2.7% |
| Thomas (1998) | United Kingdom | European | 2.1% |
| Kabasalak (2006) | Turkey | European | 1.56% |
| AECG | .72% | ||
| Zhang et al. (1995) | China | Copenhagen | .77% |
| San Francisco | .34% | ||
| Bjerrum (1997) | Denmark | European | .6% |
| Copenhagen | .2% | ||
| Dafni (1997) | Greece | European | .6% |
| Bowman (2004) | United Kingdom | AECG | .4% |
| Birlik (2009) | Turkey | European | .35% |
| AECG | .21% | ||
| Miyasaka (1995) | Japan | .33% | |
| Anagnospoulos (2010) | Greece | AECG | .23% |
| Haugen (2008) | Norway | European | .22% |
| Valim (2013) | Brazil | AECG | .17% |
| Quintana (2016) | Argentina | AECG | .17% |
| Andrianakos (2005) | Greece | AECG | .15% |
| Maciel (2015) | United States | AECG | .13% |
| Alamamos (2006) | Greece | AECG | .09% |
| Santos (2016) | Colombia | AECG | .08% |
| Sardu (2012) | Italy | European | .03% |
| Maldini (2013) | France | AECG | .01% |
A limitation of this work is that of possible mistaken registration or sub-registration by the doctors when entering the CIE10 code in clinical histories. However, this is the datum that is legally recorded when treating patients in Colombia, and it merits analysis such as the one performed in this study. Another deficiency of our study is that, given the nature of the available information, it is not possible to establish the time during which the disease developed or to estimate the incidence or severity of the same, the demand for specialist services in connection with the disease, and mortality. Given the acknowledgement of only one CIE10 code for each surgery in the majority of treatments recorded in SISPRO, our study is unable to determine the prevalence of secondary Sjögren's syndrome or the other autoimmune diseases with which SS is most frequently associated. Finally, it should be clarified that the code CIE10: M350 refers to the dry syndrome, while the SS is emphasised in brackets, so that different specialities such as maxillofacial surgery, ear, nose and throat, ophthalmology, gynaecology and endocrinology, among others, may use this same code when evaluating patients with dry symptoms due to other causes. This is therefore not necessarily a “mistake”, but rather shows that the code is very broad, and this may explain the higher prevalence reported by our study in comparison with the one undertaken in our country using COPCORD methodology.16
This study shows the prevalence of SS in terms of the report and registration available in the SISPRO of the Colombian Ministry of Health, which is one of the different ways of calculating prevalence and evaluating a disease epidemiologically, supplying information complementary to that of other methodological approaches, such as the one undertaken in our country using COPCORD methodology.16 These different approaches to prevalence data may be useful within the scientific field.
ConclusionThis study shows epidemiological and demographic information on SS in Colombia. The data agree with those reported in worldwide literature. Our study shows information gathered from the Colombian Government Ministry of Health database. This data was used to perform a demographic and epidemiological analysis of the population, and to make projections for treating patients with SS in our country.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the doctoral (PhD) programme in Clinical Epidemiology of the Pontificia Universidad Javeriana, Bogotá, Colombia, in which Doctor Daniel G. Fernández-Ávila is registered as a candidate for the title of Doctor in Clinical Epidemiology.
Please cite this article as: Fernández-Ávila DG, Rincón-Riaño DN, Bernal-Macías S, Gutiérrez Dávila JM, Rosselli D. Prevalencia y características demográficas del síndrome de Sjögren en Colombia, según información del Sistema Integral de Información de la Protección Social. Reumatol Clin. 2020;16:286–289.