To perform an extensive clinical and epidemiological characterization of our fibromyalgia patients.
Patients, material, and methodTwo-year observational study in 3 primary care centers in Terrassa, Spain. We recruited a sample of 235 individuals diagnosed with fibromyalgia being treated in primary care or rheumatology clinics who, when offered inclusion in a multidisciplinary program, agreed to provide the initial data we requested. The main measures were sociodemographic data, unhealthy habits and physical activity, comorbidities, treatment for fibromyalgia, Fibromyalgia Impact Questionnaire (FIQ), Hospital Anxiety and Depression Scale (HADS), and a family functioning scale (family APGAR).
Main resultsIn all, 97.8% were women and the average age was 54.6 years. Most of the patients had a primary school education and the majority was on sick leave. Ninety-four percent had associated comorbidity and only 3% were not taking any medication for their disease. Many were taking drugs with no proven efficacy in fibromyalgia. The majority had intermediate scores on the FIQ, the HADS showed that 63% and 53% had an anxious and/or probable depressive disorder, respectively, and, according to the family APGAR score, 62% received proper family support.
ConclusionsIn agreement with the literature, the major findings in our fibromyalgia patients were a marked predominance of women, a high incidence of comorbidities—mainly psychiatric disorders—a moderate impact of the disease and widespread use of drugs with no demonstrated efficacy.
Realizar una amplia caracterización clínica y epidemiológica de nuestra población afectada de fibromialgia.
Pacientes, material y métodoEstudio observacional a lo largo de 2años realizado en 3 centros de atención primaria de Terrassa. Muestra de 235 personas diagnosticadas de fibromialgia visitadas en consultas de atención primaria o de reumatología a las que se ofrece la asistencia al programa multidisciplinar y aceptan completar los datos iniciales del programa. Las mediciones principales fueron: datos sociodemográficos; hábitos tóxicos y ejercicio físico; comorbilidades; tratamientos para la fibromialgia; cuestionario de impacto de la fibromialgia (FIQ); escala hospitalaria de ansiedad-depresión (HADS), y cuestionario de funcionalidad familiar (APGAR familiar).
Principales resultadosEl 97,8% son mujeres; edad media, 54,6años. Predominio de pacientes con estudios primarios y en situación de baja laboral. El 94% tienen comorbilidad asociada y solo el 3% no consumen ningún fármaco para su patología, a la vez que hay un elevado consumo de fármacos sin evidencia de efectividad en la fibromialgia. La mayoría puntúan como nivel moderado en el cuestionario de Impacto de la fibromialgia (FIQ); tienen patología ansiosa y/o depresiva probable en el 63 y el 53%, respectivamente, según la Escala hospitalaria de ansiedad y depresión (HADS) y soporte familiar correcto en el 62%, según el test APGAR familiar.
ConclusionesSe confirman como datos principales y coincidiendo con la bibliografía la gran prevalencia de la fibromialgia en mujeres, con elevada comorbilidad especialmente psiquiátrica-psicológica, con moderado impacto de la enfermedad y con importante consumo de fármacos sin eficacia demostrada.
Fibromyalgia (FM) is a disorder characterized by chronic widespread pain and the presence of tenderness in defined anatomic locations.1 Incorporated in 1991 into the tenth revision of the international classification of diseases of the World Health Organization (WHO) as a nonarticular rheumatism,1,2 it is the third most common rheumatic disease and one of the most frequent causes of pain. It affects 2.4% of the population (1.5–3.2), with a maximum prevalence between 40 and 49 years of age (4.9%), and is 6–8 times more frequent among women.1,2 It is the reason for 10%–20% of visits to a rheumatologist and for 5%–8% of those to primary care clinics.1 The main symptoms are chronic pain and extreme fatigue or exhaustion. There can be many other symptoms, such as sleep problems, muscle stiffness, headache, irritable bowel syndrome, cold extremities, intolerance to drugs and chemical substances, dry mouth and eyes, frequent and/or painful urination, paresthesias, dizziness and impaired concentration and memory, which are increasingly important for the diagnosis of FM, as is shown by the new preliminary criteria drawn up in 2010 by the American College of Rheumatology (ACR)3 and subsequently modified in 2011.4 Fibromyalgia is a significant cause of disability for patients and involves high expenses, both directly, with medical visits and medication, and indirectly, with time off from work or disabilities.5–8 The major change in FM seems to be a central sensitization of the system for transmitting and producing pain of an unknown etiology. The recognized risk factors for its development would include sex (a great number of women), familial aggregation (first-degree relatives have an 8-fold higher likelihood of developing FM than the general population) and the previous presence of chronic regional pain such as headache, low back pain, myofascial pain or irritable bowel disease, with which, moreover, there is familial coaggregation. Other risk factors could be stress, hepatitis C virus (HCV) or a history of physical or psychological trauma.9–11 Patients with FM usually have considerable comorbidity, and the presence of psychiatric or psychological disorders is stressed, with an open debate on whether their presence is equivalent to that which develops in any process with chronic pain, or whether FM is a psychiatric condition.12–14 This comorbidity could also be influenced by the perception of limited general social support provided to these patients, who perceive greater support from their families and partners.15
The objective of our study was to characterize from the epidemiological and clinical points of view a series of FM patients in our area of reference, especially emphasizing the comorbidities, treatments and the impact of the disease.
Material and MethodsWe conducted a cross-sectional descriptive study in 3 primary care clinics (PCC) in Terrassa. The population studied included all the persons who attended the welcome visit that introduced them to the multidisciplinary Fibromyalgia Care Program over a period of a little more than 2 years (2011–2013). All had been seen in the rheumatology department of Hospital Mútua of Terrassa, where the diagnosis of FM had been confirmed on the basis of the 1990 ACR criteria. Attendance was totally voluntary, and the participants were asked to provide verbal consent to employ their data. In turn, the researchers involved in the study ensured complete anonymity and confidentiality in their utilization. The information collected consisted of sociodemographic data (age, sex, marital status, number of children, ethnicity, level of education, current employment, professional standing and disability); data on lifestyle (tobacco use, alcohol consumption and regular physical activity); data on their disease (time since onset of pain and fatigue, years since diagnosis, use of drugs for FM, alternative therapies, treatment at the time of the interview and familial history of FM); and comorbidity (chronic physical or psychological disorders). The information was obtained in an interview with each participant and a review of the electronic medical record. The questionnaires used were: the Fibromyalgia Impact Questionnaire (FIQ), which evaluates the impact of the disease on the activities of daily living of the patients, with a score of 0–100, the higher the score reflects a greater impact16; Family Apgar (Adaptation, Partnership, Growth, Affection and Resolve), which assesses the perception of family support, considering the family to be functionally normal if the score was 7 or more, over a maximum of 10 points17; and the Hospital Anxiety and Depression Scale (HADS), which deals with the possible coexistence of psychiatric disorders like anxiety and/or depression, which is very probable when the score it higher than 10 and not very probable when it is under 8.18 The logbook could be self-completed, but patients had the constant support of the organizers of the program to resolve doubts, and it could be done jointly if the level of education was very low.
DefinitionsSmoker: person who had had at least 1 cigarette a day over the previous year.
Habitual alcohol consumption: person who consumed at least 1 standard drink per day.
Regular physical activity: at least 1 hour of physical activity (not job-related) per day at least 3 days a week.
Concomitant or associated chronic disease: any condition reported in the patient history as an active process with a duration of over 3 months. Those considered were physical disease, whether symptomatic (osteoarthritis, hypothyroidism or disc herniation) or asymptomatic (diabetes mellitus, hypertension or dyslipidemia), and psychiatric/psychological disorders (depression, anxiety or phobias).
Statistical AnalysisDescriptive analysis, using frequencies and percentages for categorical variables and means and standard deviations for continuous variables, was done with the SPSS statistical software package, v.10 (Chicago, IL, United States).
ResultsWe collected data on 235 persons with FM, and invited 295 to participate in the multidisciplinary program (80% decided to attend).
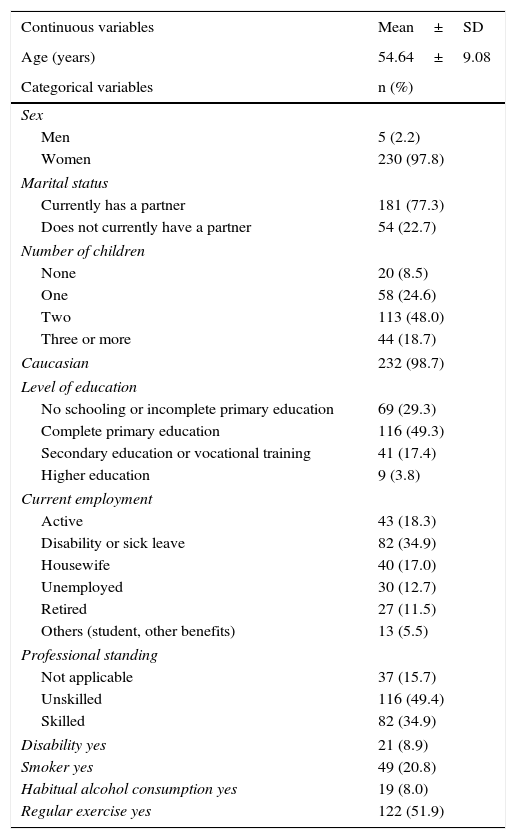
Sociodemographic data and information on lifestyle are shown in Table 1. The mean age was 54.64±9.08years, and 97.8% were women. Concerning number of children, 48.1% had 2 and 18.7% had 3 or more. In all, 77.3% had a partner. The majority of our population had completed primary studies (49.3%), and only 3.8% had a university education. At the time of the interview, 18.3% were working, most of them in positions that did not require skilled workers, whereas nearly 40% were on sick leave or had permanent disability. A very small number of them was considered to be disabled for another cause. In all, 21% were smokers, 8% had daily alcohol consumption and 52% ensured that they regularly engaged in physical activity (not job-related).
Sociodemographic Data on the Population With Fibromyalgia.
| Continuous variables | Mean±SD |
|---|---|
| Age (years) | 54.64±9.08 |
| Categorical variables | n (%) |
| Sex | |
| Men | 5 (2.2) |
| Women | 230 (97.8) |
| Marital status | |
| Currently has a partner | 181 (77.3) |
| Does not currently have a partner | 54 (22.7) |
| Number of children | |
| None | 20 (8.5) |
| One | 58 (24.6) |
| Two | 113 (48.0) |
| Three or more | 44 (18.7) |
| Caucasian | 232 (98.7) |
| Level of education | |
| No schooling or incomplete primary education | 69 (29.3) |
| Complete primary education | 116 (49.3) |
| Secondary education or vocational training | 41 (17.4) |
| Higher education | 9 (3.8) |
| Current employment | |
| Active | 43 (18.3) |
| Disability or sick leave | 82 (34.9) |
| Housewife | 40 (17.0) |
| Unemployed | 30 (12.7) |
| Retired | 27 (11.5) |
| Others (student, other benefits) | 13 (5.5) |
| Professional standing | |
| Not applicable | 37 (15.7) |
| Unskilled | 116 (49.4) |
| Skilled | 82 (34.9) |
| Disability yes | 21 (8.9) |
| Smoker yes | 49 (20.8) |
| Habitual alcohol consumption yes | 19 (8.0) |
| Regular exercise yes | 122 (51.9) |
SD, standard deviation.
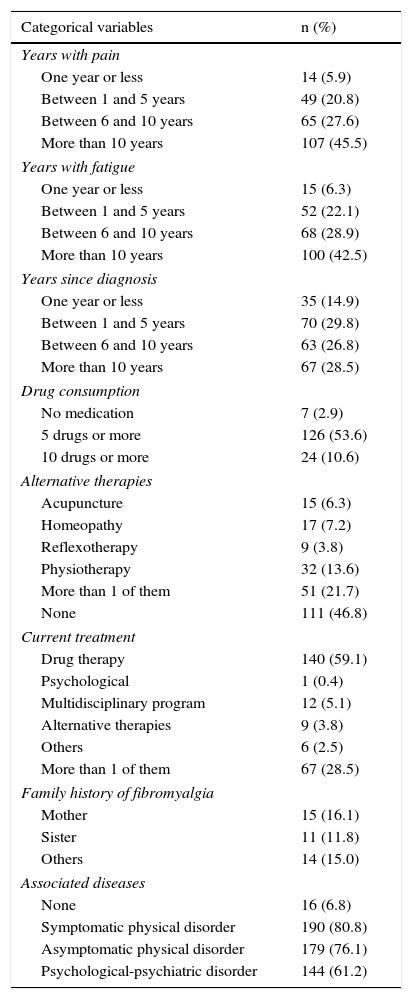
The findings related to the disease and comorbidity appear in Table 2. Most of the patients reported pain (45.5%) and fatigue (42.5%) that had begun more than 10 years ago, but 20% of these individuals had been diagnosed only 5 years earlier or less. Only 2.9% of the patients were taking no medication; in fact, taking the drug therapy was the only thing done on the part of 59% of the sample. The mean number of drugs was 5.2. Overall, 3.8% of the participants were utilizing some alternative therapy when the data was collected, but a much higher proportion (53.2%) had turned to them at some time. In all, 39.6% (93 individuals) had a family history of FM, affecting the mother, a sister or others in 16.1%, 11.8% and 15%, respectively, in those cases in which this datum was recorded. In our group, 93.2% of the patients had 1 or more associated diseases.
Associated Diseases and Data on Fibromyalgia.
| Categorical variables | n (%) |
|---|---|
| Years with pain | |
| One year or less | 14 (5.9) |
| Between 1 and 5 years | 49 (20.8) |
| Between 6 and 10 years | 65 (27.6) |
| More than 10 years | 107 (45.5) |
| Years with fatigue | |
| One year or less | 15 (6.3) |
| Between 1 and 5 years | 52 (22.1) |
| Between 6 and 10 years | 68 (28.9) |
| More than 10 years | 100 (42.5) |
| Years since diagnosis | |
| One year or less | 35 (14.9) |
| Between 1 and 5 years | 70 (29.8) |
| Between 6 and 10 years | 63 (26.8) |
| More than 10 years | 67 (28.5) |
| Drug consumption | |
| No medication | 7 (2.9) |
| 5 drugs or more | 126 (53.6) |
| 10 drugs or more | 24 (10.6) |
| Alternative therapies | |
| Acupuncture | 15 (6.3) |
| Homeopathy | 17 (7.2) |
| Reflexotherapy | 9 (3.8) |
| Physiotherapy | 32 (13.6) |
| More than 1 of them | 51 (21.7) |
| None | 111 (46.8) |
| Current treatment | |
| Drug therapy | 140 (59.1) |
| Psychological | 1 (0.4) |
| Multidisciplinary program | 12 (5.1) |
| Alternative therapies | 9 (3.8) |
| Others | 6 (2.5) |
| More than 1 of them | 67 (28.5) |
| Family history of fibromyalgia | |
| Mother | 15 (16.1) |
| Sister | 11 (11.8) |
| Others | 14 (15.0) |
| Associated diseases | |
| None | 16 (6.8) |
| Symptomatic physical disorder | 190 (80.8) |
| Asymptomatic physical disorder | 179 (76.1) |
| Psychological-psychiatric disorder | 144 (61.2) |
| Categorical variables | Mean±SD |
|---|---|
| Number of drugs | 5.20±3.19 |
SD, standard deviation.
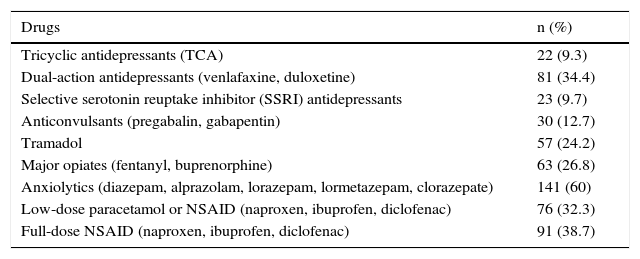
In Table 3, we specify the types of drugs that the participants had received for the treatment of FM or symptoms related to it. There was a marked use of benzodiazepine-like anxiolytics, taken by 60%, as well nonsteroidal anti-inflammatory drugs (NSAID), somewhat more than 60%. On the other hand, the use of tramadol in the therapeutic strategy was less common (25%). In all, 25% had used a major opiate. The most widely prescribed antidepressants were dual-action agents, taken in 34.4% of the cases.
Consumption of Drugs Prescribed for Fibromyalgia.
| Drugs | n (%) |
|---|---|
| Tricyclic antidepressants (TCA) | 22 (9.3) |
| Dual-action antidepressants (venlafaxine, duloxetine) | 81 (34.4) |
| Selective serotonin reuptake inhibitor (SSRI) antidepressants | 23 (9.7) |
| Anticonvulsants (pregabalin, gabapentin) | 30 (12.7) |
| Tramadol | 57 (24.2) |
| Major opiates (fentanyl, buprenorphine) | 63 (26.8) |
| Anxiolytics (diazepam, alprazolam, lorazepam, lormetazepam, clorazepate) | 141 (60) |
| Low-dose paracetamol or NSAID (naproxen, ibuprofen, diclofenac) | 76 (32.3) |
| Full-dose NSAID (naproxen, ibuprofen, diclofenac) | 91 (38.7) |
NSAID, non-steroidal anti-inflammatory drug.
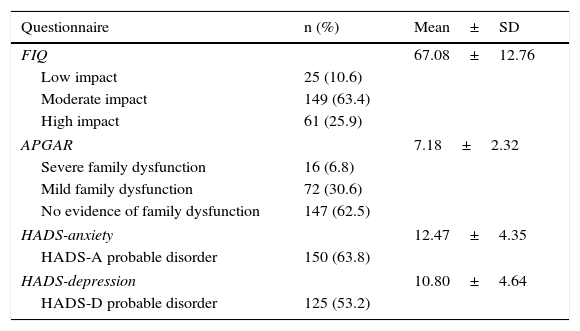
The results of the FIQ, family APGAR and HADS are shown in Table 4. More than 60% of the persons interviewed reported a moderate impact on their activities of daily living (FIQ score=50–75), with a mean of 67.08 points. The families of the patients were found to be functionally normal in 62.5% of the cases according to the APGAR, with a mean of 7.18 points, but we found that 6.8% of the families showed severe dysfunction. With respect to the detection of a psychiatric disorder using the HADS, 63.8% of the participants had probable anxiety (more than 10 points on the HADS anxiety scale), and 53.2% probable depression (more than 10 points on the HADS depression scale). The mean of these questionnaires was 12.47 and 10.80 points, respectively.
Fibromyalgia Impact Questionnaire (FIQ), Family Dysfunction (APGAR) and Associated Psychiatric Disorders (HADS).
| Questionnaire | n (%) | Mean±SD |
|---|---|---|
| FIQ | 67.08±12.76 | |
| Low impact | 25 (10.6) | |
| Moderate impact | 149 (63.4) | |
| High impact | 61 (25.9) | |
| APGAR | 7.18±2.32 | |
| Severe family dysfunction | 16 (6.8) | |
| Mild family dysfunction | 72 (30.6) | |
| No evidence of family dysfunction | 147 (62.5) | |
| HADS-anxiety | 12.47±4.35 | |
| HADS-A probable disorder | 150 (63.8) | |
| HADS-depression | 10.80±4.64 | |
| HADS-D probable disorder | 125 (53.2) | |
APGAR, Adaptation, Partnership, Growth, Affection and Resolve; FIQ, Fibromyalgia Impact Questionnaire; HADS, Hospital Anxiety and Depression Scale; SD, standard deviation.
Fibromyalgia is a prevalent disease, and our work actually corroborated many of the points that have been demonstrated in epidemiological studies in other settings, although there is not much literature on FM in Spain and few reports include as much data as this article. We confirm that it is much more common among women, and is comorbid with other chronic conditions, especially depressive and/or anxiety disorders. This disease has a moderate-to-severe impact on the activities of daily living of patients and there is a high consumption of drugs that have no demonstrated efficacy in the treatment. On the other hand, family support is clearly perceived. The prevalence in women is similar to that reported in most of the studies reviewed, exceeding 97%.19–21 The mean age is similar to that observed by Junyent et al.20 and Cerón et al.22 (57.4±10.7 and 54 years, respectively), but higher than in the populations of Gobbo et al.,21 Salgueiro et al.23 and Docampo et al.19 (approximately 49–50 years). In the majority of the reports, the proportion of persons with a university education is quite low (0.6% according to Mas et al.)2 and there is a predominance of individuals who have completed primary studies (Martín-Aragón et al.24 with 61%), as in our case. There are authors such as Docampo et al.19 or Mayorga et al.,15 whose patients have higher economic and cultural levels, that include a higher percentage of individuals who have attended a university. In other reports, there are elevated percentages of the population with very low levels of education, like Bosch et al.,25 who studied a group in which 52.3% of the participants had incomplete primary studies or no schooling. The data on the working population varies widely in the literature, from very high percentages of individuals who do not work (89% according to Cerón et al.)22 to a higher percentage of people with jobs, as in the samples of Gobbo et al.21 (56%), Docampo et al.19 (80%) and Junyent et al.20 (39%). The sample of the latter authors includes 15% of persons who cannot work because of their disease, and Ubago et al.,26 with 31.4% in the same situation, a percentage similar to ours. The EPISER study on rheumatic diseases which encompassed all of Spain showed that 15% of FM patients have transitory or permanent disability.27 The differences in age, of level of education and of professional standing shown in the literature are easily explained by the dissimilarities in the municipalities in which the studies are carried out and the selection of the patient samples (reference population, primary care or specialized clinics, population attended to or not, etc.). There is no data in the literature to compare the lifestyles of our FM patients. With respect to engaging in regular physical exercise, widely recommended in this population, Bosch et al.25 mention that 46.2% of their sample did participate in physical exercise, as did 51.5% in that of Ubago et al.,26 a finding similar to ours (51.9%). The time between the detection of symptoms and receiving the diagnosis of FM is highly variable, ranging from a mean of 4 years reported by Junyent et al.20 to more than 15 years according to Martín-Aragón et al.24 With respect to the use of drugs, the majority of the antidepressants (AD)—the treatment employed by most of these patients, as we mention in our results—are dual-action agents (venlafaxine, duloxetine), which in the most recent studies have been shown to relieve pain. Rivera et al.28 appear to demonstrate, in their work on prescription strategies, that the most effective approach would be the simultaneous prescription of an anticonvulsant and an AD. Many studies agree on the high consumption of anxiolytics, which may be explained by the marked prevalence of associated anxiety disorders. To mention one of these studies, Salgueiro et al.23 point out that 90% of the patients in their population are taking drug therapy, but that only 40% of them have scores that indicate the need for treatment. Bosch et al.25 also have a great majority of patients (92.3%) receiving medications, and 28.3% are taking more than 3. Finally, 79.9% of the sample of Ubago et al.26 are taking drugs, with 100% receiving a NSAID or paracetamol and 49.1% and 24.6% with AD and anxiolytics, respectively. A considerable percentage of our population had utilized an alternative therapy at some time to treat their disease, as did 6.2% of the patients of Ubago et al.26 and 40% of the population of Salgueiro et al.23 The evidence of the efficacy of these alternative therapies in FM is at this moment nearly inexistent. A relevant aspect that is dealt with more in the literature is the comorbidity in FM patients, especially the presence of psychiatric and psychological disorders. In all, 6.8% of our participants had no associated disease, according to their clinical history and interview. Junyent et al.20 point out the association with other rheumatic diseases in 56% of their patients, and Chamizo29 detected a possible relationship between FM and chronic viral disease (human immunodeficiency disease, HCV), as well as an increased risk of cancer and accidental death due to chronic generalized pain, whereas Mayorga et al.15 found an elevated prevalence of hypertension and diabetes mellitus (64% and 43%, respectively) in their sample. Again, in the study by Ubago et al.26 we encounter a reference to the possible association with endocrine (25.9%), cardiovascular (18.8%), rheumatic (15.2%) and gynecological (15.2%) diseases. The association with depressive and/or anxiety disorders in these patients is a widely debated subject and, as we mentioned in the introduction, there is no clear agreement as to whether depression develops as a consequence of the chronic disease, or if FM forms part of the psychiatric diseases. In any case, the prevalence of these disorders in patients with FM is highly elevated in all the literature reviewed, despite the use of different instruments to evaluate it. The 2004 study of the prevalence of mental disorders in Europe (ESEMeD/MHEDEA)30 referred to a higher risk of major depression throughout the lifetime of FM patients. In their review of studies from 2010, Revuelta et al.13 also found a higher frequency of adjustment disorders, with a depressive mood, dysthymia and major depressive disorder in patients with FM, as well as neurotic disorders (especially generalized anxiety disorder and phobias). Of the patients reported by Mayorga et al.,15 86% were diagnosed with depression and 82% with anxiety. Using the HADS, the questionnaire employed in the present report, Pareja et al.31 detected 25.5% and 44% of patients with depression and anxiety, respectively, as a probable clinical problem. Our sample somewhat surpassed those numbers. In all, 50.5% of the patients in the sample of Ubago et al.26 had a history of psychiatric disease which, in 36.4%, was present at the time of the interview. Salgueiro et al.23 detected high scores for depression and anxiety with the SCL90-R symptom checklist. Arnold et al.,12 who compared patients with FM and individuals without the disease, also found a greater risk of psychiatric comorbidity in the first group, from major depression (61.5%) to major mood disorder (74%), panic disorder (28.2%) and anxiety disorder (60.3%). The Beck Depression Inventory (BDI) has been used in several studies. Pérez et al.32 found no differences between patients with FM, patients with chronic pain for another cause and healthy patients with respect to the presence of depression with BDI, but did using the Spanish version of an inventory of situations and responses to anxiety (ISRA), in favor of patients with FM. Finally, Cerón et al.22 mention personality traits in FM patients, detecting a higher frequency of borderline personality disorder, obsessive-compulsive disorder and histrionic personality disorder. The impact of the disease in our sample is situated on the border of moderation (FIQ between 50 and 75 points). Mayorga et al.15 found a lower mean FIQ score (52.5±10.36 points) and Gelman et al.,33 somewhat higher (69.9±12.5 points). Finally, the data concerning social support mostly coincide with the literature, although the authors measure them in very different ways. We did not specifically evaluate overall institutional or social support, as the APGAR reflected only that the majority of the families functioned in a satisfactory way, and that could be the reflection of proper support of the person with FM on the part of the family. For example, Ubago et al.26 detected good support for around 71% of their patients and Mayorga et al.15 for 50%. Salgueiro et al.23 also mention a positive value of 48.9% of the patients with respect to their partners, but 49.3% were negative about their closest social setting.
In conclusion, FM mostly affects women, the mean age of whom is young. It is associated with marked comorbidity, especially involving psychological-psychiatric disorders. The consumption of medications is high and the disease has a considerable impact on daily life.
The limitations of the study are those that are common to cross-sectional observational studies, especially the inability to identify cause-effect relationships for some factors, although that was not our objective. On the other hand, the sample population has a clear selection bias since the patients are individuals with FM who at some moment came to the PCC, and were offered the possibility of participating in the multidisciplinary program. This depended on the professional with whom they talked; moreover, they attended the welcome visit. In any case, we feel that the sample is quite representative of our patient population given the high incidence, in accordance with reports in the literature. Logically, these data cannot be strictly extrapolated to other populations, given that we live in a highly specific region in the province of Barcelona in northeastern Spain. Although there is a great variability in the results in the literature, many studies involving primary care reflect trends similar to the variables reported here.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Mur Martí T, Llordés Llordés M, Custal Jordà M, López Juan G, Martínez Pardo S. Perfil de pacientes con fibromialgia que acuden a los centros de atención primaria en Terrassa. Reumatol Clin. 2017;13:252–257.