We read the publication by Nieto-González and Monteagudo1 in Reumatología Clínicawith interest, where a narrative review is undertaken of the literature in connection with the practice of using intra-articular infiltrations with corticoids (IAIC) in patients with juvenile idiopathic arthritis (JIA). We would like to describe the results of a survey of all of the members of the Spanish Paediatric Rheumatology Society (SERPE) in 2017, in which they were asked about their habitual practice in connection with several aspects of the said technique.
The survey consisted of 10 questions devised by the Scientific Committee of the 2017 National Congress of the said society. The questions refer to the medical speciality of the staff who perform IAIC (rheumatologist, paediatrician, rehabilitation doctor or orthopaedic surgeon); the type of JIA used in the said procedure; indication of analgesia and/or sedation during the process; drug(s) used; details of the IAIC technique (asepsis, washing in saline solution, dilution of the corticoid and others); maximum number of joints infiltrated in a single session; maximum number of IAIC in the same joint in one year; recommendations after infiltration; complications after infiltration; and differences between children according to their age. The “SurveyMonkey” platform was used, which makes it possible to create online surveys, (https://es.surveymonkey.com). This platform interprets the replies to surveys and creates basic descriptive statistics for them.
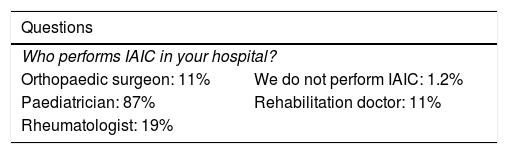
Eighty-five of the 120 members contacted replied. The survey results showed the heterogeneity of the range of professionals who perform IAIC for JIA, as other authors have reported in the past.2 The appended table shows the said results. In general, the answers to the survey reflect the absence of recognised treatment guides for this technique, showing the existence of practice that is “based on art” in the hospitals that treat young people and children with rheumatic diseases. A North American study that was also based on a survey reached similar conclusions.3
This study has several limitations, the chief one of which may be the fact that only 85 or 70% of 120 members responded to the survey. Additionally, not all of the doctors who treat rheumatic diseases in children in our country belong to the SERPE, although the majority do. On the other hand, one potentially interesting analysis was not carried out: to evaluate whether, within the heterogeneous nature of the replies, they could be found to be more homogeneous if classified according to the speciality of the respondent (rheumatologist, paediatrician, rehabilitator or orthopaedic surgeon).
There are other relevant aspects in connection with IAIC technique which we believe were included in the survey. One of these is the increasing importance of ultrasound scan imaging in paediatric rheumatology, as in recent years it has come to be included as another tool4 for use when infiltrating several locations that are considered to be “difficult” (the temporomandibular joint,5 tenosynovitis,6 the tarsal joint7). On the other hand, in all fields of paediatrics sedation-analgesic techniques are being adopted to improve the quality of care for paediatric patients; including IAIC, according to several recent publications.8–10
Although IAIC is not a technique that involves important adverse events and does not require long training to be performed in a sufficiently expert way, the authors believe it necessary to prepare guides or recommendations for the technique, for paediatric and young patients (Table 1).
Results of the survey of 120 members of the SERPE with replies from 85 of them
| Questions | |
|---|---|
| Who performs IAIC in your hospital? | |
| Orthopaedic surgeon: 11% | We do not perform IAIC: 1.2% |
| Paediatrician: 87% | Rehabilitation doctor: 11% |
| Rheumatologist: 19% | |
| Never | Sometimes | Often | Always | |
|---|---|---|---|---|
| In what clinical situations do you perform IAIC? | ||||
| Monoarthritis, % | 2,3 | 1,2 | 35 | 62 |
| Oligoarthritis, % | 0 | 18 | 71 | 11 |
| Polyarthritis, % | 2,4 | 47 | 45 | 6 |
| Relapse, % | 1,2 | 27 | 61 | 11 |
| What about analgesia and sedation? | ||||
| Chlorethyl spray, % | 60 | 17 | 13 | 10 |
| EMLA, % | 27 | 25 | 25 | 22 |
| Nitrous oxide, % | 17 | 28 | 46 | 9 |
| Benzodiazepines, % | 28 | 42 | 28 | 2,6 |
| Fentanyl, % | 69 | 20 | 12 | 0 |
| General anaesthetic, % | 42 | 27 | 30 | 1,3 |
| Local anaesthesia, % | 45 | 30 | 12 | 12 |
| Which drug do you use? | ||||
| Triamcinolone acetonide, % | 3.6 | 17 | 35 | 45 |
| Triamcinolone hexacetonide, % | 31 | 37 | 22 | 9 |
| Betamethasone, % | 75 | 15 | 10 | 0 |
| Hyaluronic acid, % | 68 | 29 | 3 | 0 |
| Itrium, % | 64 | 35 | 0 | 0 |
| What dose do you use depending on joint size? | ||||
| 0,5mg/kg in small joints and 1mg/kg in large joints: 50% | ||||
| 20mg in small joints and 40mg in large joints: 50% | ||||
| In respect of the technique | Never | Sometimes | Often | Always |
|---|---|---|---|---|
| Guided by ultrasound scan, % | 13 | 50 | 31 | 5 |
| Sterile gloves WITH surgical field, % | 6 | 8 | 13 | 72 |
| Sterile gloves WITHOUT surgical field, % | 53 | 17 | 16 | 14 |
| Only skin sterilisation, % | 89 | 4 | 5 | 2,5 |
| Dose calculated according to weight, % | 23 | 34 | 19 | 23 |
| I consider the total dose, % | 14 | 18 | 25 | 4 |
| I obtain informed consent, % | 15 | 13 | 18 | 54% |
| How many joints do you infiltrate in the same session? | Two | Three | Four | More than four |
|---|---|---|---|---|
| 30% | 31% | 35% | 4% | |
| Do you think that the same joint should not be infiltrated >3 times per year? | Yes: 76% | No: 24% | ||
| In connection with joint locations | ||||
| I infiltrate for tenosynovitis | Yes: 63% | No: 33% | ||
| I infiltrate the tarsal joint | Yes: 61% | No: 33% | ||
| I infiltrate TMJ | Yes: 30% | No: 70% | ||
| I infiltrate for IFP, MCF | Yes: 71% | No: 29% | ||
| I infiltrate for dactylitis | Yes: 50% | No: 50% | ||
| I infiltrate the hips | Yes: 60% | No: 40% | ||
| I infiltrate the sacroiliac | Yes: 6% | No: 94% | ||
| In post-filtration recommendations | Never | Sometimes | Often | Always |
|---|---|---|---|---|
| I recommend normal life without excessive effort, % | 28 | 25 | 23 | 23 |
| I recommend rest for 12-24hrs., % | 7 | 7 | 13 | 73 |
| I recommend oral analgesia, % | 14 | 41 | 24 | 21 |
| I make an appointment for them in 1-2 weeks for evaluation, % | 0 | 22 | 20 | 58 |
| I do not evaluate again, they contact in case of no improvement, % | 74 | 14 | 7 | 5 |
| Have you seen these complications? | Never | Rarely (<1/100) | Often (1/10-1/100) |
|---|---|---|---|
| Cutaneous atrophy, % | 8 | 64 | 27 |
| Septic arthritis, % | 95 | 4 | 0 |
| Vasovagal reaction, % | 55 | 41 | 3.5 |
| Haemorrhage due to arterial puncture, % | 90 | 9.4 | 0 |
| Do you establish differences for the smallest patients (< 5 years)? | Yes | No |
|---|---|---|
| I use ultrasound scan more often, % | 49 | 51 |
| I use more sedation/analgesia methods, % | 95 | 5 |
| I reduce the maximum number of IAIC, % | 35 | 64 |
| I use a lower dose of steroid in large joints, % | 63 | 37 |
EMLA: Eutectic Mixture of Local Anaesthetic; IAIC: intra-articular infiltration with corticoids; IFP: proximal interphalangeal; MCF: metacarpophalangeal; SERPE: Sociedad Española de Reumatología Pediátrica; TMJ: temporomandibular joint.
Please cite this article as: Murias Loza S, Graña Gil G. Respuesta a: Estado actual del tratamiento con infiltraciones intra-articulares en la artritis idiopática juvenil. Reumatol Clin. 2021;17:179–181.