We present the clinical and serological characteristics of four patients with rhupus (Simon's definition). The 4 patients with rhupus presented ACR criteria for SLE as well as for RA, ANA positive with titers ranging from 1/80 to 1/5250, and positive anti-DNA, with the predominance of symmetrical erosive polyarthritis. We found anti-CCP positivity and high titers in 3 of the 4 patients, and positive antiphospholipid antibodies in 2 (anticardiolipin and LA), without manifestation of antiphospholipid syndrome. One patient presented renal affection, and 2 with subcutaneous nodules. The 3 patients with RA preceded the manifestations of SLE by an average of 7.7 years. Two patients were refractory to conventional DMAR in combination, requiring biologic and mycophennolate mofetil.
Presentamos las características clínicas y serológicas de cuatro pacientes con diagnóstico de rhupus (definición de Simon). Presentaban criterios ACR tanto para LES como para AR, factor antinuclear (FAN) positivo a títulos desde 1/80 a 1/5.250 y anti-DNAn positivo, predominando como manifestación clínica una poliartritis simétrica erosiva. Se halló anti-CCP positiva y a títulos altos en 3 de los 4 pacientes y anticuerpos antifosfolípidos en 2 (anticardiolipina y anticoagulante lúpico), sin manifestación de síndrome antifosfolípido. Sólo un paciente presentó compromiso renal y 2 nódulos subcutáneos. En 3 de los pacientes el diagnóstico de AR precedió a las manifestaciones de LES en un promedio de 7,7 años. La mitad fue refractaria a fármacos antirreumáticos modificadores de la enfermedad (FAME) convencionales en combinación y requirió biológicos y micofenolato mofetil.
Joint compromise in systemic lupus erythematosus (SLE) is one of the most common manifestations of this disease, with only a small fraction of patients (∼5%) developing deformity in the form of Jaccoud's arthropathy. Less than one percent of patients with SLE develop erosive disease which is indistinguishable from rheumatoid arthritis (RA), an entity known as rhupus.1
If rhupus represents an overlap of SLE and RA, a subgroup of SLE with an intense joint expression or a completely different entity is still a matter of debate. There is evidence to sustain the existence of rhupus as a true overlap syndrome.2
Toone et al. performed the first clinical observations that helped to identify this disease,3 and the term rhupus was proposed by Schur in 1971.4
We present a series of cases that analyze clinical and serologic characteristics of patients with a diagnosis of rhupus.
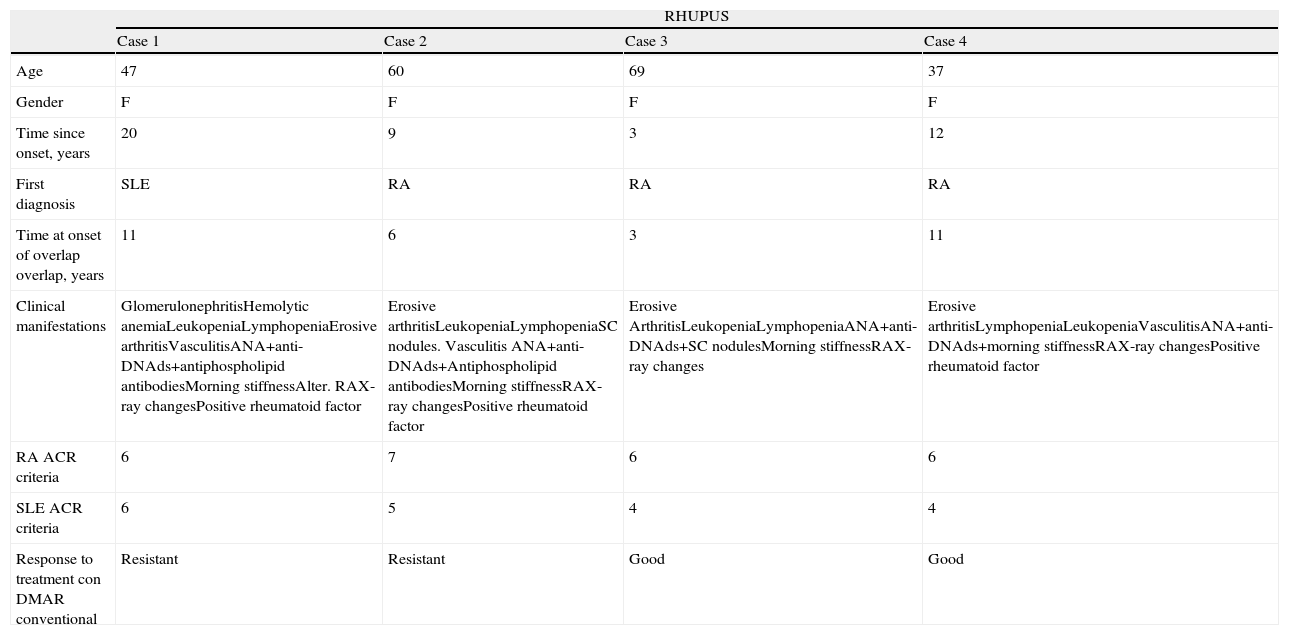
Patients and MethodsWe present 4 cases of rhupus, classified according to Simon et al.5,6 (symmetric and erosive polyarthritis with accompanying signs and symptoms of SLE, and the presence of highly specific anti-dsDNA or anti-SM antibodies). Demographic characteristics, forms of presentation, predominant manifestations are shown in Table 1, presence of classification criteria for SLE (ACR1997), as well as RA (ACR 1987), serologic markers and treatment.
Demographic and Clinical Characteristics.
| RHUPUS | ||||
| Case 1 | Case 2 | Case 3 | Case 4 | |
| Age | 47 | 60 | 69 | 37 |
| Gender | F | F | F | F |
| Time since onset, years | 20 | 9 | 3 | 12 |
| First diagnosis | SLE | RA | RA | RA |
| Time at onset of overlap overlap, years | 11 | 6 | 3 | 11 |
| Clinical manifestations | GlomerulonephritisHemolytic anemiaLeukopeniaLymphopeniaErosive arthritisVasculitisANA+anti-DNAds+antiphospholipid antibodiesMorning stiffnessAlter. RAX-ray changesPositive rheumatoid factor | Erosive arthritisLeukopeniaLymphopeniaSC nodules. Vasculitis ANA+anti-DNAds+Antiphospholipid antibodiesMorning stiffnessRAX-ray changesPositive rheumatoid factor | Erosive ArthritisLeukopeniaLymphopeniaANA+anti-DNAds+SC nodulesMorning stiffnessRAX-ray changes | Erosive arthritisLymphopeniaLeukopeniaVasculitisANA+anti-DNAds+morning stiffnessRAX-ray changesPositive rheumatoid factor |
| RA ACR criteria | 6 | 7 | 6 | 6 |
| SLE ACR criteria | 6 | 5 | 4 | 4 |
| Response to treatment con DMAR conventional | Resistant | Resistant | Good | Good |
Demographic and clinical characteristics of the four patients studied are seen in Table 1.
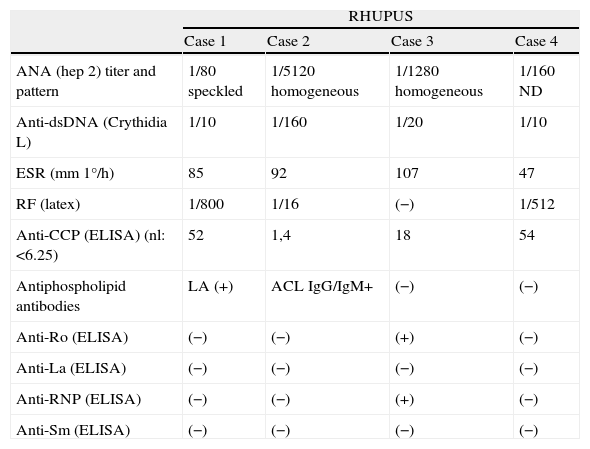
All the patients presented symmetric chronic bilateral and erosive polyarthritis, 2 of them with subcutaneous nodules. Only one patient presented an initial diagnosis of SLE. Three patients had 6 classification criteria for RA and one had all 7. All the others had 4 or more criteria for SLE. Serologic markers are shown in Table 2.
Serologic Characteristics.
| RHUPUS | ||||
| Case 1 | Case 2 | Case 3 | Case 4 | |
| ANA (hep 2) titer and pattern | 1/80 speckled | 1/5120 homogeneous | 1/1280 homogeneous | 1/160 ND |
| Anti-dsDNA (Crythidia L) | 1/10 | 1/160 | 1/20 | 1/10 |
| ESR (mm 1°/h) | 85 | 92 | 107 | 47 |
| RF (latex) | 1/800 | 1/16 | (−) | 1/512 |
| Anti-CCP (ELISA) (nl: <6.25) | 52 | 1,4 | 18 | 54 |
| Antiphospholipid antibodies | LA (+) | ACL IgG/IgM+ | (−) | (−) |
| Anti-Ro (ELISA) | (−) | (−) | (+) | (−) |
| Anti-La (ELISA) | (−) | (−) | (−) | (−) |
| Anti-RNP (ELISA) | (−) | (−) | (+) | (−) |
| Anti-Sm (ELISA) | (−) | (−) | (−) | (−) |
ACL: anticardiolipin; LA: lupus anticoagulant.
All the patients were treated with combined therapy. The most commonly used were hydroxychloroquine, methotrexate and leflunomide. Two patients achieved clinical remission (DAS 28<2.6); and the other 2 patients presented both clinical and radiologic progression and one was treated with abatacept and another with mycophenolate mofetil.
DiscussionThe coexistence of two or more connective tissue diseases in the same patient is a rare phenomenon, particularly for the coexistence of SLE and RA, which has been estimated between 0.01% and 2%.5–7
Since the first description of the term (1960), there have been difficulties in identifying these patients due to the lack of clear parameters used to define the entity. Simon et al. studied a group of 1500 patients with SLE and 2000 with RA, identifying 116 who presented both diagnoses; however, only 22 had enough data to support a diagnosis of rhupus. These authors defined it as an erosive symmetric polyarthritis, accompanied by signs and symptoms of SLE and the presence of high specificity autoantibodies (anti-dsDNA or anti-SM antibodies).5,6 These patients present with RA characteristics, developing SLE characteristics afterwards, few present it simultaneously and even less when SLE is the initial diagnosis.5,6
The diagnosis of RA preceded the manifestations of SLE (3 of 4 patients) by a mean of 7.7 years, which was later than that described by Amuezca-Guerra and Simon2,5 (around 4 years) and only one patient presented an SLE disease at onset, adding persistent, bilateral, symmetric, erosive and seropositive polyarthritis to the 4 year progression. Two patients were resistant to treatment with combination disease modifying antirheumatic drugs (DMARD) and required treatment with abatacept and mycophenolate mofetil.
RA characteristics dominate the clinical picture, with erosive symmetric polyarthritis being the commonest and rheumatoid nodules in 40% of these patients. The most common SLE characteristics in rhupus are usually skin related (malar rash, photosensitivity and alopecia), hematological (leukopenia, thrombocytopenia), serositis (pleural and pericardial effusion) and mucosal compromise.
Advances in diagnostic methods allowed for the observation of the presence of molecules currently considered as specific markers of one or the other disease separately, such as anti-dsDNA or anti-CCP. From the analysis of the HLA-DR molecules, the genetic characterization of patients with a diagnosis of rhupus showed cleared differences with those present in patients with RA and SLE, supporting the possibility of an independent entity.2,5,6 Taking into account the role of the HLA molecules on the physiopathology of rhupus needs more research; it was observed that these patients were distinguished by the presence of alleles HLA-DR4, DR2, DR6 and DR1, presenting a greater frequency of DR1 than patients with RA and less frequency of DR3 than patients with SLE.6
As in RA, 67% of patients with SLE and erosions have alleles of the shared epitope (SE), in contrast with 22% of those with non-erosive arthritis. The presence of two copies of SE increase the risk of erosive arthritis in SLE by a factor of 8.6
Two patients presented antiphospholipid antibodies; as has been described in Mexican patients, none presented clinical manifestations of antiphospholipid syndrome.5
Three of the four patients with rhupus had positive anti-CCP. The presence of elevated anti-CCP antibodies are highly specific (96%–98%) in patients with RA.3,5
Amezcua-Guerra and other authors observed that these antibodies are present in similar frequency and titers in rhupus and RA, but significantly higher than in patients with non erosive arthropathy in SLE.8
There is a strong association between these antibodies and rhupus, which would increase the risk of developing erosive arthritis in SLE between 18 and 28 times; this sustains the hypothesis that these antibodies have a direct pathogenic role (including the shared epitope) in the development of a severe erosive arthritis, without considering the underlying disease.9
Finally, patients with rhupus have a significantly higher CRP serum concentration than that of patients with non erosive arthritis due to SLE (14.5 vs 0.8mg/l respectively; P=001), suggesting that CRP may be an active pathogenic agent, in addition to its known serologic marker for an erosive arthritis pattern in SLE.10
Is rhupus an overlap, a subgroup of SLE with intense joint expression or a different entity? In response to treatment of RA and SLE separately, the presence of 4 or more SLE characteristics of SLE in patients with a prior diagnosis of RA (15.5%) duplicates the risk of death in these patients, and the presence of anti-CCP antibodies would constitute a predictor of erosive arthritis in patients with SLE and constitute more than enough reasons for the continued study of this disease.2
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article as: Benavente EPI, Paira SO. Rhupus: reporte de 4 casos. Reumatol Clin. 2011. doi:10.1016/j.reuma.2010.12.006.