Right ventriculoarterial coupling (RVAC) is altered early before presenting right ventricular dysfunction and pulmonary hypertension, its measurement in patients with RA has been barely studied.
ObjectivesTo determine if there is a difference in right ventricular arterial coupling (RVAC) in patients with RA. Analyze if there are differences in patients with normal vs abnormal right RVAC. To investigate if there is an association in patients with RA to present abnormal RVAC.
MethodsA single-center, analytical, cross-sectional, observational study was performed. Patients with a diagnosis of RA were included according to the ACR/EULAR 2010 classification criteria, without any other comorbidity, the echocardiograms were made at the Hospital Civil de Guadalajara “Fray Antonio Alcalde”. An ACUSON SC 2000 echocardiogram was used. Patients were compared with healthy controls matched by age and gender. The clinical, laboratory and echocardiographic variables were contrasted. The RVAC was determined with the right ventricular free wall longitudinal strain (RVFWLS) / pulmonary artery systolic pressure (PSAP) ratio.
ResultsFifty one patients were included in each group. Among the echocardiographic variables, it was found that patients with RA had a greater right ventricular diastolic area and the PASP; while the RV FAC, the RVFWLS and the RVAC were lower. RA was independently associated to an abnormal RVAC.
ConclusionThe right ventricular subclinical myocardial damage, determined by the RVAC, is present in patients with rheumatoid arthritis, and it was associated with an abnormal ventriculoarterial coupling.
El acoplamiento ventriculoarterial derecho puede alterarse precozmente antes de presentar disfunción del ventrículo derecho e hipertensión pulmonar, su medición en pacientes con Artritis Reumatoide ha sido poco estudiado.
ObjetivosDeterminar si existe diferencia en el acoplamiento ventriculoarterial derecho en pacientes con AR. Investigar si existe la asociación en pacientes con AR para presentar acoplamiento ventriculoarterial anormal.
MétodosSe realizó un estudio unicéntrico, analítico, transversal, observacional. Se incluyeron los pacientes con diagnóstico de AR según los criterios de clasificación de la ACR/EULAR 2010, sin ninguna otra comorbilidad, que se les realizó un ecocardiograma en el Hospital Civil de Guadalajara “Fray Antonio Alcalde”. Se compararon los pacientes con controles sanos pareados por edad y género. Se contrastaron las variables clínicas, de laboratorio y ecocardiográficas. El acoplamiento ventriculoarterial derecho se determinó con la relación strain de la pared libre del ventrículo derecho (SLPLVD)/presión sistólica de arteria pulmonar (PSAP).
ResultadosSe incluyeron 51 pacientes en cada grupo. Dentro de las variables ecocardiográficas, se encontró que los pacientes con AR tenían mayor área telediastólica del VD, la PSAP; mientras que fue menor la FAC VD, el SLPLVD y el AVAD. Se asoció que el padecer AR era un factor asociado de manera independiente a la disminución del AVAD.
ConclusiónEl daño miocárdico subclínico del ventrículo derecho, determinado por el acoplamiento ventriculoarterial, está presente en los pacientes con Artritis reumatoide. El padecer artritis reumatoide se asociaron a presentar un acoplamiento ventriculoarterial anormal.
Rheumatoid arthritis (RA) is a multisystem inflammatory disease that manifests primarily as symmetrical peripheral polyarthritis; however, the extra-articular condition has been widely described. Specifically, the cardiovascular manifestations that have been reported are ischemic heart disease, pericardial alterations, valvular heart disease, and pulmonary hypertension.1 The pathophysiology of cardiovascular disease can be explained by immunological abnormalities, systemic inflammation, small vessel disease, accelerated atherosclerosis, and a procoagulant state.2,3
The multiple alterations that RA can cause in the heart have been previously cited, the most described being ischemic heart disease, heart failure, valvular heart disease, diastolic dysfunction, pericardial alterations, and pulmonary hypertension.4 Recently, there have been multiple studies which have observed how patients with RA have reduced myocardial strain compared to healthy controls, demonstrating subclinical myocardial damage long before any complication such as heart failure, ischemic heart disease, or pulmonary hypertension could occur.5–11
Right ventriculoarterial coupling (RVAC is the relationship between the right ventricle and the afterload generated by lung pressure. It is a marker of subclinical damage, in addition to being a predictor of mortality in patients with pulmonary hypertension and heart failure.12
The aim of the study was to determine whether patients with RA have greater subclinical myocardial damage caused by a decreased RVAC compared to healthy controls, in addition to determining whether there was an association between RA and decreased RVAC.
MethodsA single-centre, analytical, cross-sectional, observational study was conducted. Patients diagnosed with RA according to the classification criteria of the ACR/EULAR 2010, without any other comorbidity, who had undergone an echocardiogram at the Fray Antonio Alcalde Civil Hospital of Guadalajara, were included. Patients with a known concomitant disease or who had a diagnosis of structural heart disease, ischemic heart disease, interstitial lung disease, or COPD were excluded. Patients were compared with healthy controls matched by age and gender. Clinical, laboratory and echocardiographic variables were contrasted. The echocardiograms were analysed by 2 cardiologists highly specialised in echocardiography, for whom the clinical data of the patients were blinded. The echocardiogram used was a Siemens ACUSON SC2000™ and myocardial strain was performed using the VVI technique.
The clinical variables were: gender, age, body mass index, time of evolution of RA, the physician-patient analogue visual scale, the Clinical Disease Activity Index (CDAI), the Simplified Disease Activity Index (SDAI), the Disease Activity Score (DAS28), the Health Assessment Questionnaire-Disability Index (HAQ-DI), the Physician's Global Approach (PhsGA) and the patient global approach (PxGA).
The laboratory variables were: haemoglobin (g/dL), leukocytes (109/L), creatinine (mg/dL), total cholesterol (mg/dL), HDL-C (mg/dL), LDL-C (mg/dL), C-reactive protein (CRP) (mg/L), rheumatoid factor (U/mL) and anti-CCP antibodies. The cardiovascular risk of all patients was calculated using the American Heart Association/American College of Cardiology (AHA/ACC) and the Cardiovascular Risk Score (QRISK) scales.
The echocardiographic variables that were determined were: left ventricular ejection fraction, left ventricular indexed volume, left atrium indexed volume, right ventricular diastolic area, right ventricular shortening fraction, right atrium volume, pulmonary artery systolic pressure (PASP), right ventricular free wall longitudinal strain (RVFWLS), and global longitudinal strain (GLS) of the right atrium; RVAC were determined with the SLPLVD/PSAP ratio.
Myocardial strain refers to what percentage each myocardial fibre shortens or lengthens during the cardiac cycle; specifically, SLPLVD refers to how much the myocardial fibres of the free wall shorten longitudinally, that is, the movement of the base towards the tip of the right ventricle.
Quantitative variables were contrasted with the Student's t or Mann-Whitney U tests by the normality of the variables; qualitative variables were compared with χ2. The association with abnormal RVAC was determined with multiple regression analysis; Variables with p < 0.1 were passed on to the next model.
Statistical analysis was run using MedCalc version 15.0 software. Statistical significance was determined with a p < 0.05.
The Fray Antonio Alcalde Civil Hospital of Guadalajara Ethics Committee rules were followed, and the study was approved with folio CEI 272/23, based on the Declaration of Helsinki.
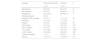
ResultsA total of 51 patients with a diagnosis of RA were collected, matched by age and gender with healthy controls (Table 1). The mean age was 46 years; there was a higher proportion of female, with 4 out of 5 patients being women. Patients with RA had a higher degree of cardiovascular risk according to the AHA/ACC and QRISK scales.
Comparison of clinical and laboratory characteristics of patients.
| Variable | Rheumatoid arthritis | Controls | p |
|---|---|---|---|
| n = 51 | n = 51 | ||
| Age (years) | 46 (±12) | 50 (±12) | .2 |
| Sex (female) | 39 (76%) | 40 (80%) | .8 |
| BMI (kg/m2) | 27.2 (±4.5) | 25.8 (±4.7) | .1 |
| Evolution (years) | 8 (±7) | ||
| AHA/ACC RA corrected | 3.0 (±2.1) | 1.7 (±1.5) | .03 |
| AHA/ACC | 2.1 (±1.8) | 1.7 (±1.5) | .4 |
| QRISK | 4.9 (±3) | 3.2(±4.2) | .03 |
| CRP (mg/L) | 10.7 (±6) | 3.2(±2.3) | .001 |
| HDL-c (mg/dL) | 47 (±12) | 41 (±10) | .02 |
| TC (mg/dL) | 172 (±33) | 144 (±37) | <.001 |
| c-LDL (mg/dL) | 103 (±28) | 85 (±33) | .003 |
| Creatinine (mg/dL) | .7 (±.1) | 0.8 (±.2) | .09 |
| Hb (g/L) | 13.2 (±1.7) | 13.8 (±1.4) | .08 |
AHA/ACC: American Heart Association/American College of Cardiology; BMI: body mass index; CRP: C-reactive protein; Hb: haemoglobin; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol; TC: total cholesterol; QRISK: Cardiovascular Risk Score; RA: rheumatoid arthritis.
Within the biochemical parameters, a significant difference was found in haemoglobin values, these being lower in patients with RA. Total cholesterol values were higher in patients with RA, in addition to having a higher atherogenic risk due to higher levels of LDL-C.
The median time of evolution for RA was 8 years, with a mean of DAS28, CRP of 3.3, and 65% had criteria for disease activity (Table 2).
Parameters of patients with rheumatoid arthritis.
| Variable | Value |
|---|---|
| FRI | 48 (94%) |
| Anti-CCP | 28 (65%) |
| PhsGA | 3.7(±2.2) |
| PxGA | 3.8(±2.6) |
| CDAI | 11.3 (±9) |
| SDAI | 13.7 (±10) |
| DAS28 | 3.3 (±1.2) |
| Activity | 33 (65%) |
| HAQ | .75 (±.6) |
Anti-CCP: anti-cyclic citrullinated peptide antibodies; CDAI: clinical disease activity index; DAS28: disease activity score; HAQ: health assessment questionnaire; PhsGA: physician’s global approach; PxGA: patient global approach; RF: rheumatoid factor; SDAI: simplified disease activity index.
As regards echocardiographic variables (Table 3), no difference was found in the left ventricular ejection fraction, left ventricular indexed volume, right atrium volume, or in the right atrium SGL; on the other hand, there was a difference in the end-diastolic area and PASP, these being higher in patients with RA, while the right ventricular shortening fraction, SLPLVD and RVAC were lower in RA.
Comparison of echocardiographic variables.
| Variable | Rheumatoid arthritis | Controls | P |
|---|---|---|---|
| Indexed LV volume (mL/m2) | 49 (±13) | 53 (±9) | .08 |
| LVEF (%) | 62 (±6) | 63 (±3) | .2 |
| Volume RA (mL/m2) | 39 (±14) | 29 (±2) | <.001 |
| RV SF (%) | 39 (±8) | 52 (±9) | <.001 |
| PASP (mmHg) | 33 (±11) | 25 (±4) | <.001 |
| RV telediastolic area (cm2) | 18 (±5) | 15 (±3) | .01 |
| SLPLVD (%) | −21.8 (±7) | −24.3 (±4) | .02 |
| RA Strain (%) | 49 (±13) | 56 (±2) | .07 |
| Ventriculoarterial coupling (%/mmHg) | .72 (±.3) | 1 (±0.2) | <.001 |
LV: left ventricle; LVEF: left ventricular ejection fraction; PASP: pulmonary artery systolic pressure; RVFWLS: right ventricular free wall longitudinal strain; RA: right atrium; RV: right ventricle; SF: shortening fraction.
When running multiple regression (Table 4) in search of an association with a decreased RVAC, we were able to find that RA was an associated factor, as well as CRP and total cholesterol levels, whereas in model 2, only RA was an independent factor associated with decreased RVAC.
Association of clinical variables with abnormal right ventriculoarterial coupling.
| Variable | Model 1 | Model 2 | ||
|---|---|---|---|---|
| β | p | β | p | |
| RA | −.467 | <.0001 | −.376 | .0001 |
| Age | .029 | .8 | ||
| Sex (female) | .079 | .4 | ||
| BMI | −.155 | .1 | ||
| Evolution | −.185 | .2 | ||
| RA corrected AHA/ACC | −.087 | .4 | ||
| AHA/ACC | −.052 | .6 | ||
| QRISK | .069 | .5 | ||
| C-reactive protein | −.299 | .002 | −.184 | .07 |
| c-HDL | −.144 | .2 | ||
| Total cholesterol | −.205 | .04 | −.055 | .06 |
| c-LDL | −.136 | .3 | ||
| Creatinine | .133 | .2 | ||
| Hb | .155 | .3 | ||
| Rheumatoid factor | −.176 | .2 | ||
| Anti-CCP | .001 | .9 | ||
| PhsGA | −.191 | .2 | ||
| PxGA | −.259 | .07 | −.107 | .3 |
| CDAI | −.130 | .4 | ||
| SDAI | −.149 | .3 | ||
| DAS28 | −.216 | .1 | ||
| HAQ | −.216 | .1 | ||
AHA/ACC: American Heart Association/American College of Cardiology; Anti-CCP: anti-cyclic citrullinated peptide antibodies; BMI: body mass index; CDAI: clinical disease activity index; DAS28: disease activity score; HAQ: health assessment questionnaire; Hb: haemoglobin; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol; PhsGA: physician’s global approach; PxGA: patient global approach; QRISK: Cardiovascular Risk Score; RA: rheumatoid arthritis; SDAI: simplified disease activity index.
The main finding in this study was the presence of an abnormal RVAC, characterised by a decrease in the SLPLVD PASP ratio in patients with active RA with no history of cardiovascular disease, compared to a normal control group. In addition, the presence of changes in the dimensions of the right chambers (ventricle/atrium) was found, characterised by an increase in end-diastolic volume and lower systolic function, determined by the shortening fraction and longitudinal strain.
Although until a few years ago the right ventricle was considered the "forgotten ventricle", the trend towards its study has been increasing due to the clinical implication it entails. This is the reason why this cavity was chosen as the target of the study, taking the SLPLVD/PASP ratio as a method to determine subclinical myocardial damage. Fine et al. found impaired biventricular GLS in 59 RA patients compared to normal subjects.13
In addition, another study run with the Mexican population with RA carried out by Azpiri-Lopez et al.14 showed that the systolic function determined by the systolic excursion of the tricuspid annulus was decreased in patients with RA, and RVAC were also investigated, using the systolic excursion of the tricuspid ring/PASP relationship, which was also lower in this patient population.
Left ventricular systolic function, determined by the ejection fraction, was normal in both groups, confirming the usefulness of the strain methodology for early detection of myocardial damage. This finding was supported by Naseem et al.,15 who studied 120 patients with active RA and assessed the relationship of the degree of disease activity with left and right ventricular function by echocardiogram with the strain method, and reported a statistically significant association between the disease score and the prediction of subclinical right ventricular dysfunction (r = −0, 682, p ≤ 0.001 and r = −0.731, p ≤ 0.001) value for SDAI and DAS28 scores, respectively.
In previous studies, the chronic systemic inflammatory state inherent in RA has been associated with a mechanism of subclinical myocardial dysfunction due to the cellular and microvascular fibrotic process. In our study, the elevation of the inflammatory markers studied (CRP) maintained a clear statistical significance with the previously mentioned echocardiographic findings. This was supported by Løgstrup et al.,16 who evaluated left ventricular function in relation to serum anti-CCP levels, finding a significant correlation between the deterioration of the GLS and anti-CCP titres during the 2-year follow-up. This is contrary to the data reported by Magda et al.,17 who found no significant relationship in the biological markers of inflammation and myocardial fibrosis (CRP, interleukins 6 and 10, P selectin) due to the apparent adequate therapeutic control of their study group.
An important aspect to mention, due to the clinical implications this entails in late stages of the disease, is PASP. Although in both groups of our study this remained within normal ranges, statistical significance was observed for the increase found in patients with RA, which demonstrates the usefulness of the echocardiogram as a diagnostic tool in the early stages of pulmonary hypertension. Ünlü et al.,18 through retrospective analysis of echocardiograms in patients with precapillary pulmonary arterial hypertension, showed that the RVFWLS/PASP ratio showed adequate prediction with a sensitivity of 92% and a specificity of 82.5%. Although there is no validation of this method in the context of RA, it gives rise to further research around finding non-invasive tools.
As shown in our results, the risk scales (AHA/ACC adapted for RA and QRISK) demonstrated a statistically significantly increased cardiovascular risk, confirming that RA is considered a cardiovascular risk factor in people who suffer from it. In their study, Magda et al.17 found the same association, represented by the presence of subclinical right ventricular dysfunction in patients with no known cardiovascular or pulmonary disease. Multiple studies2,8,19–24 have shown that patients with RA are at increased risk of atherosclerosis, as well as having higher levels of total cholesterol and LDL-C compared to healthy controls, so it is not surprising that this association was seen in our cohort of patients.
According to the statistical analysis performed, a statistically significant association was observed for abnormal RVAC in patients with active RA disease, evaluated by the Physician's Global Assessment of Disease Activity and with positive CRP and total cholesterol levels. This coincides with what was observed by Midtbø et al.25 when studying 78 patients and noting greater shortening of the GLS in patients with active disease, compared to patients with RA in remission (49). Total cholesterol levels were another marker that showed a significant association (β = −0.205, p ≤ 0.04), a fact to be considered since in the study carried out by Naseem et al.15 no greater association was found.
Among the limitations of the study is the fact that it was a single-centre study with a relatively small sample of patients. Another point to take into account is that most of the patients had disease activity.
To our knowledge, this is the first study to document the clear association of RA with a decrease in RVAC, this being a relevant fact since it tells us about the subclinical myocardial damage of this patient population, which may be an early marker of increased pulmonary pressures. The present study and its results may serve as a background for future multicentre studies with a larger number of patients and variables, depending on the different demographic contexts observed in the evolution of the disease, before determining the routine clinical use of this echocardiographic method.
An important point to consider in prospective studies that has not been taken into account so far is the association and influence of therapy for the disease with the results obtained to determine a possible containment of myocardial damage, or the definitive use of cardiovascular therapy. This leads us to the question of whether giving more intensive treatment early in patients with RA could alter the course of myocardial damage. This study opens the doors to clarifying these questions in future lines of research to reduce cardiovascular morbidity and mortality in patients with RA.
ConclusionsPatients with RA have an abnormal RVAC, determined by a decreased RVFWLS/PASP ratio, in addition to an association of RA with abnormal RVAC. This value indicates the subclinical myocardial damage that is present in patients with RA, this being an early marker of right ventricular dysfunction at increased pulmonary pressures.
The authors declare that they have no conflict of interest.