Case history of a small girl outlet with epilepsy, followed by scleroderma skin damage and uveitis, neurovasculitis with white matter foci in brain on the side of skin lesion in two months, immunologic disease activity. Resistance to conventional immunosuppressive therapy forced us to initiate the treatment with tocilizumab. It was well tolerated and led to significant improvement of brain, ocular and skin manifestations.
Historia de la enfermedad de una niña con epilepsia, así como las lesiones cutáneas de la esclerodermia y la uveítis, la neurovasculitis con materia blanca se centra en el cerebro en el lado de la lesión de la piel en 2 meses, la actividad de las enfermedades inmunológicas. La resistencia a la terapia inmunosupresora tradicional nos hizo comenzar el tratamiento con tocilizumab. Fue bien tolerado y condujo a una mejoría significativa en las manifestaciones cerebrales, oculares y de la piel.
Linear scleroderma “en coup de sabre” (LSCS) is a subset of linear scleroderma, affecting frontopariental region, with frequent neurological and ophthalmological involvement. Neurological symptoms (NS) in LSCS are presented with epilepsy, headache, focal neurologic deficits, movement disorders, neuropsychiatric symptoms and ocular involvement including anterior uveitis, episcleritis, glaucoma and keratitis.1 Based on the most accepted hypothesis NS in LSCS are caused by neurovasculitis and focal cerebral inflammation.2–4
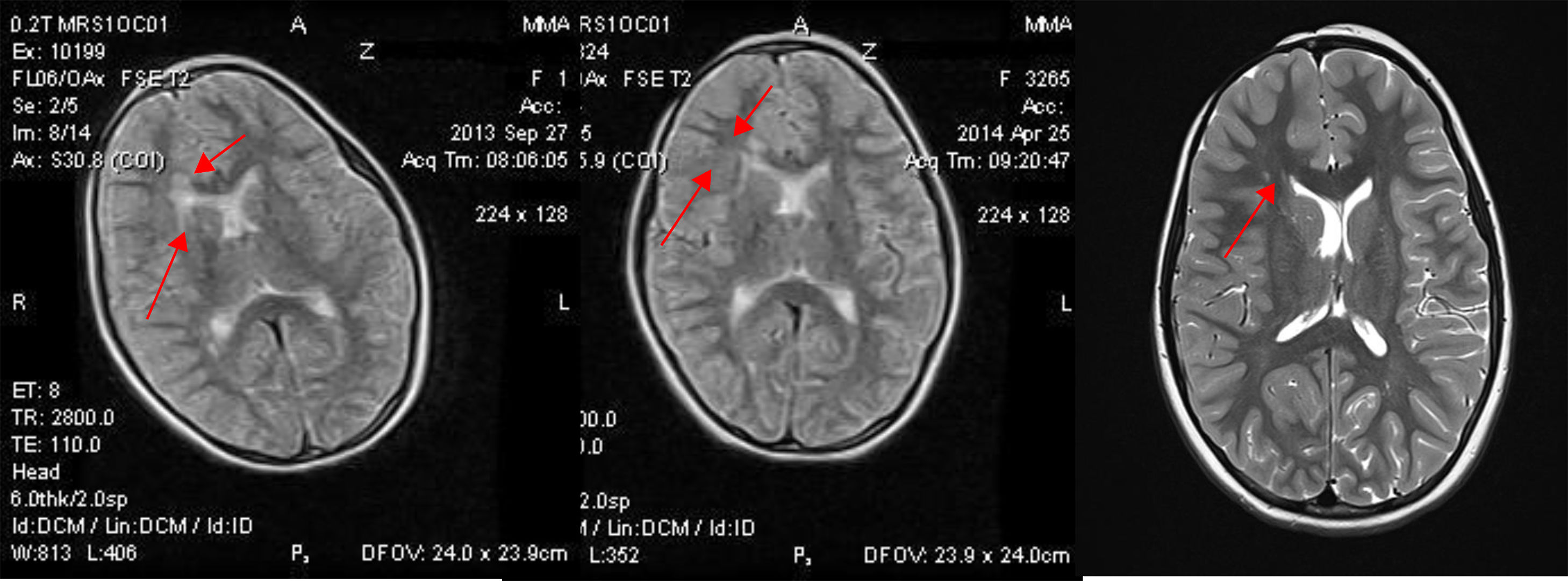
Case reportA Caucasian girl of 2 years 10 months developed vomiting, weakness in left hand, loss of consciousness, over a period of a month – partial clonic seizures with left clonic jerks and, loss of consciousness. Cerebral MRI revealed areas of hyperintense signals in white matter of the periventricular zone of the body, front and rear horn of the right lateral ventricle of the brain. Criptogenic focal epilepsy was diagnosed, she was given carbomazepine 16mg\kilo, and seizures stopped.
Two months later an ivory-colored skin spot with violaceous borders with induration and hyperpigmentation appeared on in the middle of forehead (Fig. 1). In four months asymmetry of her face, linear alopecia of the right frontoparietal zone were noticed. Seizures renewed and, the right iridocyclitis outbursted. The diagnose of LSCS was made. Physical and instrumental examination found no internal organ involvement but MRI and EEG showed brain lesions. Laboratory tests showed elevated serum Ig G level and rheumatoid factor.
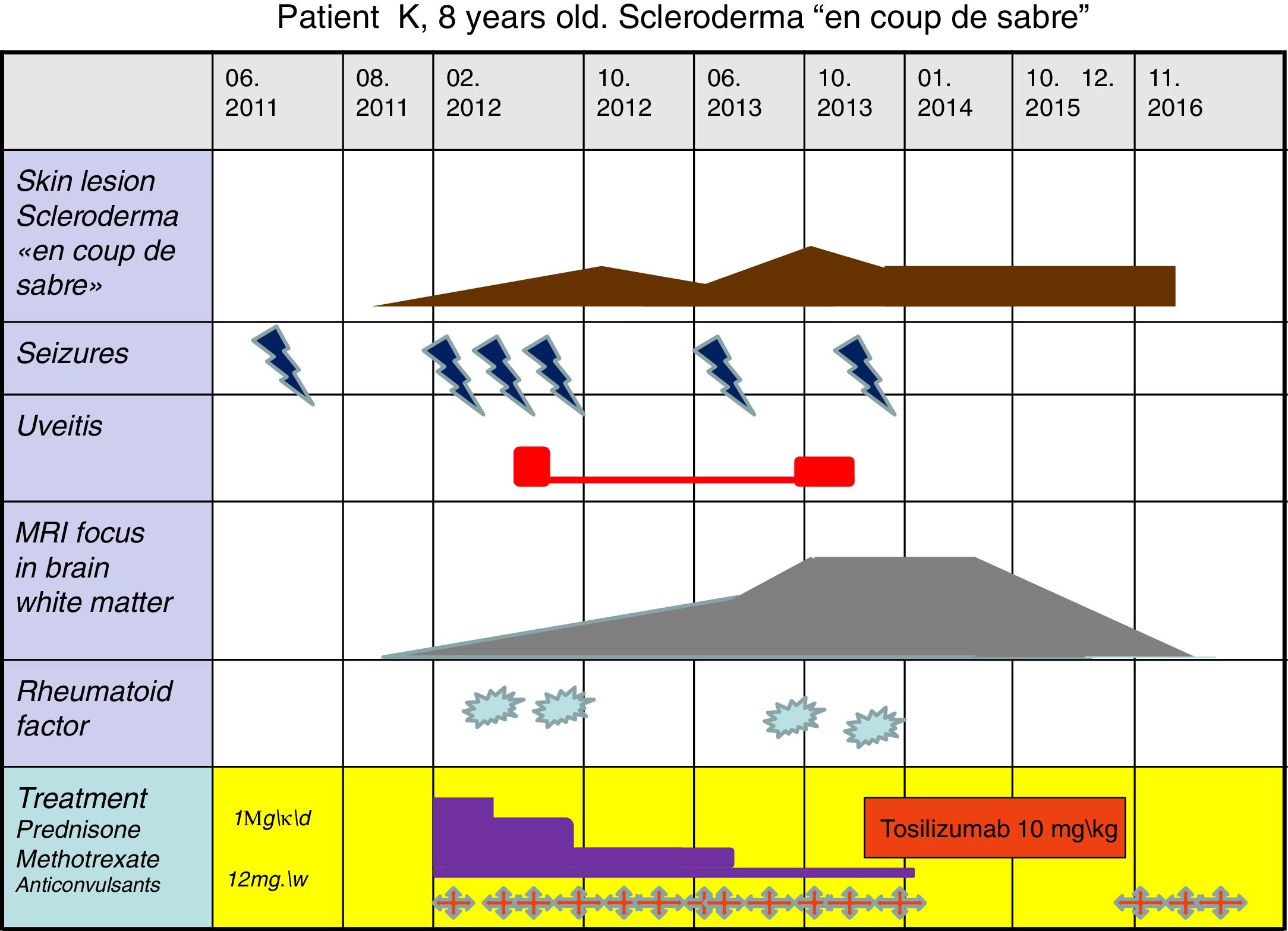
Treatment with oral prednisone 1mg\kg.b.w\daily was started for 10 weeks, then tapped and methotrexate (MTX) 10mg\b.sq.\weekly, carbomazepin retard 300mg daily, folic acid, local treatment of skin lesions. During the first 2 months the condition of the patient improved, she stopped seizures and skin progression. But, at the daily prednisone dose 17.5mg, skin process relapsed. MTX dose was increased to 12mg\b.sq. During the following 10 months the patients’ condition was stable. Nevertheless, in 16 months of treatment epileptic activity and skin progression restarted, uveitis activated. Brain MRI showed the enlargement of periventricular white matter lesion, up to 30×14mm (Fig. 2).
Disease development is shown in Fig. 1.
Uneffectiveness of immunodepressant treatment forced us to initialize a biologic agent. We started Tz infusions 10mg\kg once in 4 weeks, accompanied by prednisone 5mg\daily, MTX 12mg\b.sq\w., additionally – topiromat and valproic acid. Monthly infusions of Tz were continuated for 26 months, prednisone was stopped after 2 months and MTX in 4 months after initiation of Tz treatment. Thus, for the latter 20 months the patient received only Tz. Cerebral MRI performed after 6 months of Tz therapy showed diminution of periventricular focus in white matter to 27×13mm. Distinct reduction of foci (23×11mm) was found after 12 months of Tz treatment (Fig. 2).
Skin ivory colored spots and induration disappeared, the intensity of fibrotic lesions decreased, hair start to grow in the area of alopecia. There were no seizures, EEG pattern improved, so valproic acid was stopped, no relapses of uveitis were detected.
Therapy with Tz lasted for 26 months, when repeated cerebral MRI showed the absence of previous foci in the brain (Fig. 2). We stopped Tz infusions, but reinduced MTX injections weekly (12mg\b.sq). Follow up period of 12 months, shows no disease progression, the girl continue MTX treatment.
DiscussionThis case report shows dramatic improvement after Tz treatment in a girl with convention treatment resistant LCDS. Hyperintense lesions on T2-weighted MRI documented an acute inflammatory process in the brain,5 as a result the neurovasculitis – a part of systemic vascular disfunction in scleroderma. The severity of neurovasculitis was resistant to conventional immunodepressant therapy, but Tz produced strong antiinflammatory effect and the white matter lesions disappeared. The efficacy of Tz suggests, that neurovaculitis in scleroderma may be reversible, which correlates with the other publications.6
There are similar publications on promising results of Tz in scleroderma,7–9 further investigations are needed to evaluate indications for biologics in scleroderma with NS involvement.
FundingThere were no funding or granting of work.
Conflict of interestsThere is no conflict of interests among the authors.