Attention of a patient with a swollen joint and fever is a medical emergency due to the possibility of septic arthritis.
The sternoclavicular joint is a rare localization for septic arthritis in patients without risk factors (intravenous drug users [IDU]), immunocompromised patients, diabetes, etc.).1 In this type of involvement there are serious possible complications such as abscesses, mediastinitis, osteomyelitis and empyema.1
Here, we report the case of a patient with sternoclavicular septic arthritis and secondary empyema.
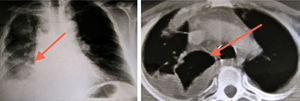
The patient, a 63-year-old male was admitted to our hospital for right shoulder pain lasting one week and three days with high fever. He had a painful tumor on the right sternoclavicular region and discrete pulmonary hypoventilation at the base of the same side. The rest of the examination was unremarkable and revealed no history of risk factors. He had leukocytosis with neutrophilia, elevated erythrocyte sedimentation rate (ESR) and fibrinogen, no other laboratory abnormalities. Chest X-ray showed a condensing image in the right upper lobe and a diffuse condensation of the right base (Fig. 1). Shoulder X-rays showed no abnormalities. The chest CT observed disintegration of the articular margins and periarticular fluid collection which continued to the subclavicular region, anterior pleural and right lung base (Fig. 1).
We performed arthrocentesis of the acromioclavicular joint, isolating Staphylococcus aureus (S. aureus) in the synovial fluid and in blood cultures. According to the antibiogram, the patient was treated with intravenous cloxacyllin. We performed a thoracocenthesis and obtained a liquid with data of infection and an analytical result with a high suspicion of empyema, so we placed a chest drainage tube. With both treatments there was a significant improvement and resolution of the problem.
The incidence of septic arthritis appears to increase in certain types of population (prosthetic infections, immunocompromised, IDU, etc.).2
The sternoclavicular joint may be affected by 9% of cases of septic arthritis.3
The clinical presentation is usually insidious, with pain localized to the shoulder or paracervical region, which may delay diagnosis, increasing the percentage of local complications, abscesses and even the extension of the process within the thorax.1
One study 1 describes the target population for this type of septic arthritis as a young population. In our case, the patient exceeded the average age suggested by these authors (45 years).
In all age groups at risk the most common organisms identified was S. aureus, as in our case, as well as in other gram positive agents.2 In the case of sternoclavicular septic arthritis, S. aureus causes half of the cases.1 However, we must not forget other organisms such as Pseudomonas aeruginosa, which is a major cause of septic arthritis in certain patient groups such as IVDU.1
Given the potential for serious complications described above, a chest CT should be performed after a chest X-ray and at any abnormality of the latter. Our patient had no clear respiratory symptoms, except for a mild dry cough three days before admission, as well as fever and malaise during the same days, so one must be guided not only by the clinical data. From the onset we started antimicrobial therapy against S. aureus with oxacyllin or vancomycin, due to the risk of resistance to methicillin. If the patient belonged to a different risk group we would have covered gram-negatives with cephepime or piperacyllin-tazobactam, for example, or in case of carbapenem resistance.1
We report a patient with sternoclavicular septic arthritis and secondary empyema, with no risk factors and who started as a painful shoulder. These facts have encouraged us to communicate the clinical features, diagnosis and treatment, having thought about the possibility of sternoclavicular arthritis when we observed fever accompanied by severe pain in the shoulder or paracervical region.
Please cite this article as: Moreno Martínez MJ, et al. Artritis séptica esternoclavicular y empiema. Reumatol Clin. 2012;8(2):102-103.