Psoriatic arthritis (PsA) is a chronic immune-mediated inflammatory disease that affects the musculoskeletal system and skin, and manifests heterogeneously, with a variable course. In current clinical practice, variability and limitations in its follow-up have been observed. The aim of the CREA project was to agree on strategies to improve the initial assessment and follow-up of patients with PsA in Spain.
Materials and methodsA survey was conducted among a representative sample of expert rheumatologists in Spain, containing 33 questions on current clinical practice, available resources, and current limitations in the follow-up of patients with PsA. The results were discussed in regional meetings and 105 strategies were proposed and finally evaluated by 85 experts in a Delphi consensus.
ResultsThe most important limitations in the follow-up of PsA were lack of consultation time, lack of nursing staff, and delays in performing imaging tests. A total of 108 strategies were proposed related to the assessment of quality of life and disease-impact indices; comorbidities and extra-articular manifestations; laboratory tests; imaging tests; physical examination and metrology; and activity and function indices. Of the total, 53 were considered highly advisable, with no regional differences in consensus values.
Discussion and ConclusionsThe proposals offered in the current study are applicable to the entire country, respond to the unmet needs detected in the initial survey, form a minimum action framework, and ensure optimal follow-up of patients with PsA.
La artritis psoriásica (APs) es una enfermedad inflamatoria crónica mediada por el sistema inmune que afecta al sistema musculoesquelético y la piel, y se manifiesta de forma heterogénea y con un curso variable. En la práctica clínica habitual se ha observado variabilidad y limitaciones en su seguimiento. El objetivo del proyecto CREA fue consensuar estrategias de mejora para la valoración inicial y el seguimiento de los pacientes con APs en España.
Materiales y métodosSe realizó una encuesta a una muestra representativa de reumatólogos expertos del territorio español, que contenía 33 preguntas sobre la práctica clínica habitual, los recursos disponibles y las limitaciones actuales en el seguimiento de los pacientes con APs. Se discutieron los resultados en reuniones regionales y se propusieron 105 estrategias que, finalmente, fueron valoradas por 85 expertos en un consenso Delphi.
ResultadosLas limitaciones destacadas en el seguimiento de la APs fueron la falta de tiempo en consulta, de personal de enfermería, y el retraso en la realización de pruebas de imagen. Se propusieron 108 estrategias relacionadas con la evaluación de los índices de calidad de vida e impacto de la enfermedad; las comorbilidades y manifestaciones extraarticulares; las pruebas de laboratorio; las pruebas de imagen; la exploración física y metrología; y los índices de actividad y función. Entre todas, 53 se consideraron altamente aconsejables, sin diferencias regionales en los valores de consenso.
Discusión y ConclusionesLas propuestas ofrecidas en el estudio actual son aplicables a todo el territorio nacional, responden a las necesidades no cubiertas detectadas en la encuesta inicial, conforman un cuadro de actuación mínimo y aseguran un seguimiento óptimo de los pacientes con APs.
Psoriatic arthritis (PsA) is a chronic immune-mediated inflammatory disease that causes joint destruction and disability, with heterogeneous manifestations and a variable disease course1,2. It has a prevalence in Spain of around .6% of the population3.
PsA can affect the musculoskeletal (arthritis, spondylitis, enthesitis, or dactylitis) and extra-articular (skin and nail involvement, uveitis, or inflammatory bowel disease) levels4. It has been reported that 25%-70% of patients with PsA may have axial involvement, possibly exclusively in 5%5. As some dermatologists or primary care physicians may be unfamiliar with axial manifestations, it is important that they use symptoms, physical examination, and imaging tests to detect them6.
PsA is associated with a high prevalence of certain comorbidities including hypertension and diabetes mellitus7. The various manifestations of PsA8 and the associated comorbidities9 have a major impact on patients' quality of life (QoL) and require multidisciplinary management10,11.
The challenges emerging in the management of PsA have been addressed by a panel of experts at European level, and recommendations have been formulated to increase awareness of the disease among the specialists involved, improve early diagnosis, and promote multidisciplinary care12. In Spain, quality standards have been published to promote integrated multidisciplinary care and improve the quality of care offered to patients with PsA11,13, but their implementation has been variable and probably insufficient14,15. An action chart was developed to help in the assessment of patients with PsA16, and consensus was reached on which variables should be assessed in patients receiving biological therapy17.
This was the framework for the CREA project, which was conducted with two objectives: a) to understand usual clinical practice, the available resources, and current limitations in the follow-up of patients with PsA, and b) to develop and agree on strategies to optimise the diagnosis and follow-up of patients with PsA in Spain.
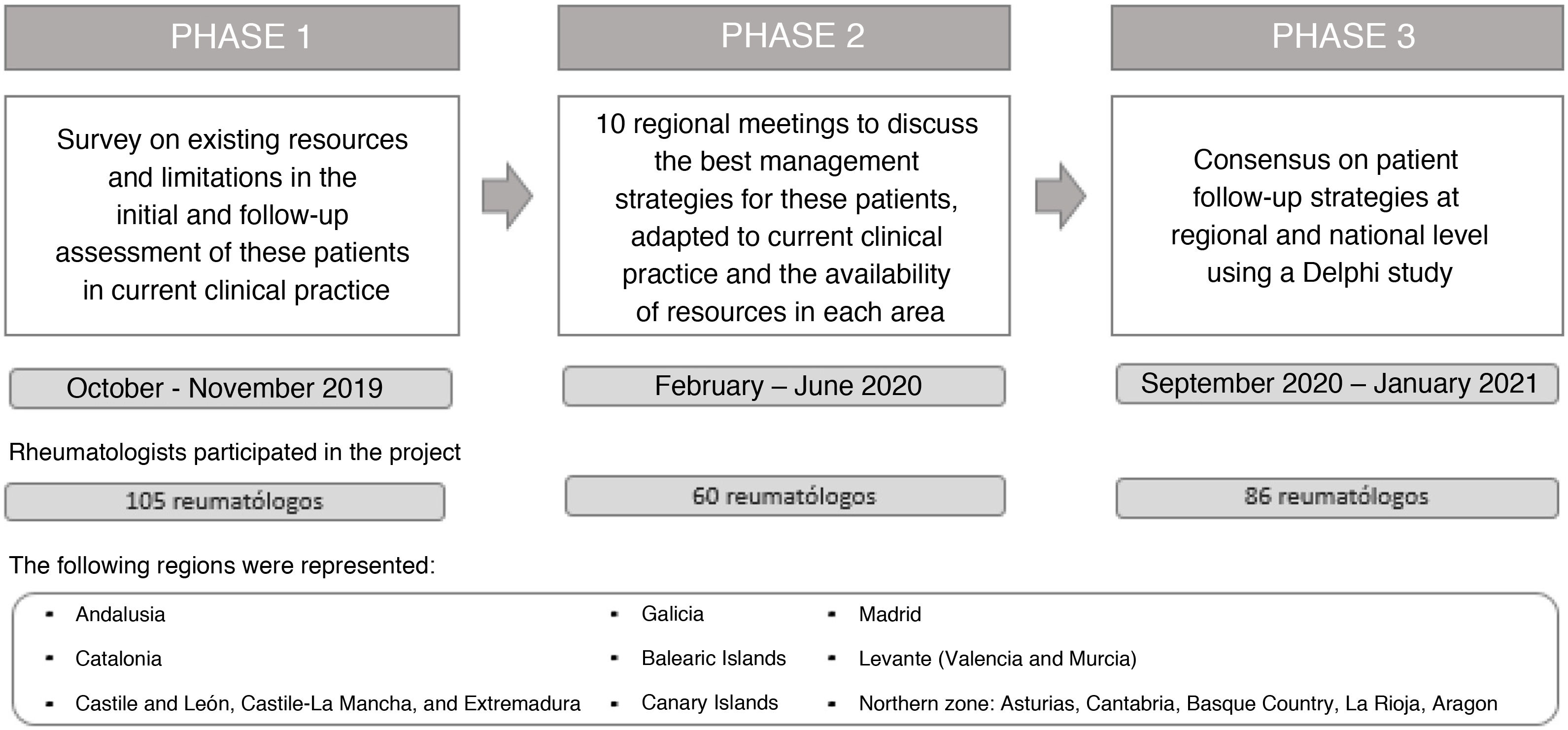
MethodsThe CREA project was developed in 3 distinct phases: a national survey; a series of meetings to discuss the results of the survey at regional level and propose strategies adapted to each territory; and a Delphi consensus to validate the proposed strategies (Fig. 1).
Survey of resources and limitationsA scientific committee composed of 10 experts designed a survey on the specialised care of patients with PsA, to determine the resources and limitations in routine clinical practice. The survey comprised 33 questions including different items, organised in 4 sections: a) Profile of the participating physician, b) Patient management in the practice, c) Patient assessment, and d) Limitations encountered in clinical practice (Appendix B Supplementary material 1). The survey was answered by a sample of 105 rheumatologists selected by the scientific committee, with proven interest and experience in the management of PsA, members of the Spondyloarthritis Study Group of the Spanish Society of Rheumatology (GRESSER) and representing the different regional areas, from October to November 2019 (Table 1).
Profile of participants and distribution of regional participation in the different phases of the CREA project.
| Total sample | Andalusia | Catalonia | Castile and Leon, Castile-La Mancha, and Extremadura | Galicia | Balearic Islands | Canary Islands | Madrid | Levantea | Northern Zoneb | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Participation by phase | |||||||||||
| Phase 1: Survey on resources and limitations, n (%) | 105 (100%) | 12 (11.4%) | 12 (11.4%) | 7 (6.7%) | 14 (13.3%) | 4 (3.8%) | 9 (8.6%) | 12 (11.4%) | 21 (20.0%) | 16 (15.2%) | — |
| Phase 2: Regional meetings, n (%) | 60 (100%) | 5 (8.3%) | 6 (10.0%) | 6 (10.0%) | 6 (10.0%) | 5 (8.3%) | 5 (8.3%) | 8 (13.3%) | 13 (21.6%) | 6 (10.0%) | — |
| Phase 3: Consensus on management strategies, n (%) | 85 (100%) | 9 (10.6%) | 13 (21.7%) | 6 (10.0%) | 9 (15.0%) | 1 (1.7%) | 8 (13.3%) | 10 (16.7%) | 19 (31.7%) | 10 (16.7%) | — |
| Description of participation | |||||||||||
| Age, mean (min., max.) | 48.3 (30, 67) | 48.6 (30, 67) | 48.7 (31, 65) | 50.7 (32, 60) | 49.9 (35, 65) | 53.3 (48, 63) | 48.9 (33, 61) | 48.8 (36, 60) | 44.7 (33, 67) | 48.4 (31, 60) | .722 |
| Type of centre | .873 | ||||||||||
| Public hospital | 94.0% | 100.0% | 100.0% | 100.0% | 93.0% | 100.0% | 89.0% | 92.0% | 95.0% | 88.0% | |
| Private hospital | 3.0% | .0% | .0% | .0% | .0% | .0% | 11.0% | 8.0% | .0% | 6.0% | |
| Specialty outpatient centre | 3.0% | .0% | .0% | .0% | 7.0% | .0% | .0% | .0% | 5.0% | 6.0% | |
| Years of experience, mean (min, max.) | 20 (5, 40) | 18.5 (6, 35) | 20.1 (5, 36) | 24.3 (8, 35) | 21.8 (7, 40) | 24.8 (20, 34) | 21.2 (7, 33) | 21.2 (10, 35) | 16.0 (5, 36) | 21.8 (7, 40) | .424 |
| Patients attended in one year, mean (min., max.) | 1517.4 (400, 5000) | 1245.8 (500, 4000) | 950 (800, 4400) | 1950 (450, 2800) | 1790 (150, 2600) | 1950 (100, 3100) | 1266.7 (500, 4000) | 1666.7 (100, 6300) | 1225.1 (720, 6300) | 2023.1 (200, 2125) | .163 |
| Patients with PsA attended in one year, mean (% with respect to total patients) | 250 (19.0%) | 351 (30.0%) | 273 (32.0%) | 231 (20.0%) | 372 (20.0%) | 304 (14.0%) | 390 (18.0%) | 290 (15.0%) | 246 (20.0%) | 243 (12.0%) | .999 |
| Available resources | |||||||||||
| PsA | |||||||||||
| Initial visit | |||||||||||
| Time available for consultation, % | 21-30 min, 46.7% | 16-20 min, 66.7% | 21-30 min, 75.0% | 21-30 min,57.1% | 21-30 min, 71.4% | 21-30 min, 50.0% | 21-30 min, 66.7% | 16-20 min, 41.7% | 16-20 min, 71.4% | 16-20 min, 50.0% | .009 |
| Optimal time, mean (min., max.) | 33.9 (15, 60) | 31.3 (20, 50) | 36.7 (30, 45) | 32.1 (30, 45) | 33.9 (25, 45) | 40.0 (30, 45) | 38.9 (30, 60) | 32.1 (20, 40) | 32.4 (20, 45) | 33.8 (15, 45) | .230 |
| Follow-up visit | |||||||||||
| Time available for consultation, % | 10-15 min, 66.4% | 10-15 min, 100.0% | 10-15 min, 75.0% | 10-15 min,42.9% | 10-15 min, 71.4% | 10-15 min, 50.0% | 16-20 min, 55.6% | 10-15 min, 58.3% | 10-15 min, 66.7% | 10-15 min, 62.5% | .056 |
| Optimal time, mean (min., max.) | 20.9 (10, 30) | 19.6 (15, 30) | 19.2 (15, 20) | 20.7 (15, 30) | 20.0 (15, 30) | 23.8 (20, 30) | 24.4 (20, 30) | 21.3 (15, 30) | 20.5 (10, 30) | 21.9 (15,30) | .169 |
| Rheumatology residents, Yes % | 54.0% | 92.0% | 83.0% | 14.0% | 36.0% | 0% | 78.0% | 67.0% | 29.0% | 63.0% | <.001 |
| Dedicated PsA consultation, Yes % | 43.0% | 66.7% | 58.3% | 28.6% | 21.4% | 50.0% | 22.2% | 41.7% | 52.4% | 37.5% | .281 |
| Type of dedicated consultation | .059 | ||||||||||
| Rheuma/dermatology | 76.0% | 88.0% | 71.0% | 100.0% | 100.0% | 100.0% | 100.0% | 40.0% | 82.0% | 50.0% | |
| Early PsA | 44.0% | 38.0% | 43.0% | 67.0% | 50.0% | 60.0% | 46.0% | 50.0% | |||
| Availability of rheumatology nurse, Yes % | 77.6% | 75.0% | 100.0% | 71.4% | 71.4% | 25.0% | 77.8% | 66.7% | 90.5% | 75.0% | .105 |
| Tasks carried out by rheumatology nurse | .068 | ||||||||||
| Education on treatments | 95.2% | 88.9% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 89.5% | 91.7% | |
| Analytical controls of treatments | 62.7% | 44.4% | 58.3% | 40.0% | 60.0% | 100.0% | 71.4% | 50.0% | 78.9% | 66.7% | |
| Measurement of cardiovascular risk factors (weight, BMI, abdominal circumference, BP) | 61.4% | 66.7% | 83.3% | 60.0% | 60.0% | 100.0% | 85.7% | 62.5% | 36.8% | 58.3% | |
| Using AxSpa, peripheral SpA and PsA assessment indices | 51.8% | 22.2% | 83.3% | 40.0% | 40.0% | 100.0% | 28.6% | 50.0% | 63.2% | 50.0% | |
| Joint examination and spinal metrology | 37.3% | 22.2% | 25.0% | 60.0% | 50.0% | 100.0% | 71.4% | .0% | 52.6% | 16.7% | |
| Patient training in group chats | 24.1% | .0% | 33.3% | .0% | 30.0% | .0% | 14.3% | 25.0% | 47.4% | 8.3% | |
| Computerised clinical records, Yes % | 99.1% | 100.0% | 85.7% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | .071 |
| Recording of PsA patient assessment in digital database, Yes % | 49.5% | 66.7% | 58.3% | 14.3% | 57.1% | 25.0% | 66.7% | 41.7% | 52.4% | 37.5% | .351 |
BMI: Body Mass Index; BP: Blood Pressure; PsA: Psoriatic arthritis.
Frequency tables were used to describe nominal variables and measures of central tendency and dispersion for continuous variables. The data obtained were analysed globally and by region.
Regional meetingsBetween February and June 2020, 10 regional meetings were held to discuss the results of the survey on resources and limitations, and to propose and discuss solutions adaptable to routine clinical practice, and the availability of resources in each geographical area. A total of 60 rheumatologists (approximately 6 experts per meeting) responded, who had previously participated in the survey. A total of 108 strategies applicable to the follow-up of patients with PsA were proposed and a Delphi questionnaire was developed. These strategies were organised into 6 distinct sections: a) Quality of life and disease impact indices, b) Physical examination and metrology, c) Assessment of comorbidities and extra-articular manifestations, d) Disease activity and function indices, e) Laboratory tests and f) Imaging tests (Appendix B Supplementary material 2).
Delphi consensusThe Delphi questionnaire was answered in 2 waves, between September 2020 and January 2021; 92 rheumatologists who had previously participated in the survey on resources and limitations participated in the first wave, and 85 of them participated in the second wave.
The proposed strategies were rated as "highly desirable", "desirable", and "dispensable", and the level of agreement and desirability were assessed using a Likert-type scale: ratings 1 to 3 were considered "disagree"; 4 to 6, "neutral"; and 7 to 9, "agree". It was established that 70% or more of the participants had to agree on the same answer for a strategy to be considered agreed.
ResultsProfile of the participantsThe mean age of the participants in the survey on resources and limitations was 48.3 years and they had an average of 20 years of experience in their specialty. A total of 55% were women; 94% worked in a public hospital.
The mean number of patients seen per year was 1517, 19.0% of whom were patients with PsA. Of the patients with PsA, 48% were from primary care and 32% from dermatology (Table 1).
Survey on resources and limitationsAvailable resourcesOf the participants, 54% had rheumatology residents, with notable differences between the different areas (78% in the Canary Islands, 0% in the Balearic Islands). Forty-three percent had a dedicated PsA practice and 78% had rheumatology nurses, who mostly oversaw patient education on treatments. Computerised medical records were available in 99% of the cases and a digital patient assessment database in 47% (Table 1).
Patient management in the practiceAccording to 47% of the participants, the time available for the first visits of patients with PsA was 21-30 min, although the mean time considered optimal was 33.9 min. Sixty-six percent stated that the time available for follow-up visits was 10-15 min and the mean time considered optimal was 19.3 min.
Forty percent of the participants agreed to assess patients with active PsA every 2 months, and 64% agreed to assess those with inactive or minimally active PsA every 6 months.
Patient assessmentHip examination, skin and nail assessment, and tender entheses count were performed in more than 80% of cases. However, more than 50% of participants did not perform the following tests: thoracic expansion, Schöber test. or its modified version, finger-to-floor distance, intermalleolar distance, lateral trunk flexion, or tragus-to-wall test. The physician generally performed physical examination and metrology of patients with PsA.
According to 61% and 63% of the participants, respectively, fibromyalgia points and abdominal circumference were not assessed. According to 21% and 37%, respectively, weight/height/body mass index (BMI) and blood pressure were not assessed.
Disease activity and function indices were generally assessed by the physician. More than 80% of the participants used the global and pain visual analogue scale (VAS). The DAPSA (Disease Activity in psoriatic Arthritis Index) was used by 67% of the participants. Less than half the participants used the following: BASFI (Bath Ankylosing Spondylitis Functional Index), BASDAI (Bath Ankylosing Spondylitis Disease Activity Index), BSA (Body Surface Area), ASDAS (Ankylosing Spondylitis Disease Activity Score), MDA (Minimal Disease Activity), PASI (Psoriasis Area Severity Index), and BASMI (Bath Ankylosing Spondylitis Metrology Index).
More than 90% reported using peripheral X-ray of the hands and feet, cervical/dorsal/lumbar lateral spine, and plain X-ray of the pelvis in patient assessment. The first was mostly used at the time of diagnosis; the second, according to symptoms; and the third, at the time of diagnosis, periodically or according to symptoms. Magnetic resonance imaging of the sacroiliac or spinal joints and ultrasound were used occasionally, usually depending on the patient's symptoms.
All the comorbidities and extra-articular manifestations proposed were evaluated by 60% or more of the participants.
The PtGA (Patient Global Assessment) was found to be the index used most frequently to assess the overall condition of the patient with PsA (by 49% of participants), while only 28% used the PsAID-12 (Psoriatic Arthritis Impact of Disease) questionnaire, generally every 6-12 months.
Limitations in clinical practiceLack of consultation time, lack of nursing and/or support staff, and delay in performing imaging tests were most highlighted as limitations in the management and assessment of patients with PsA, while lack of access to imaging tests and lack of knowledge of indices and questionnaires were the least (Table 2).
Limitations reported among the experts regarding the management and assessment of patients with AxSpA. Result so the national survey on resources and limitations.
| Total sample (N = 107) | Andalusia (n = 12) | Catalonia (n = 12) | Castile and Leon, Castile-La Mancha, and Extremadura (n = 7) | Galicia (n = 14) | Balearic Islands (n = 4) | Canary Islands (n = 9) | Madrid (n = 12) | Levantea (n = 21) | Northern Zoneb (n = 16) | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lack of time for consultation | 3.83 | 3.75 | 3.50 | 3.71 | 3.64 | 3.50 | 3.67 | 4.08 | 4.29 | 3.75 | .583 |
| Lack of nursing staff and/or support | 3.62 | 4.00 | 3.00 | 3.29 | 3.43 | 4.25 | 3.89 | 3.75 | 3.71 | 3.56 | .533 |
| Delay in performing imaging tests | 3.32 | 3.17 | 3.25 | 3.14 | 3.86 | 4.00 | 3.56 | 3.50 | 2.81 | 3.31 | .379 |
| Lack of access to imaging tests | 1.44 | 1.83 | 1.08 | 1.14 | 1.50 | 1.25 | 1.11 | 1.58 | 1.67 | 1.31 | .533 |
| Lack of knowledge of indices/questionnaires for patient assessment | 1.53 | 1.33 | 1.08 | 1.57 | 1.86 | 2.00 | 1.56 | 1.42 | 1.67 | 1.50 | .252 |
| Lack of adequate digital resources for data collection | 3.05 | 2.75 | 3.33 | 3.43 | 2.79 | 2.75 | 2.78 | 3.33 | 3.24 | 2.88 | .920 |
| Lack of communication with PCP | 2.9 | 3.08 | 2.92 | 3.29 | 2.79 | 2.75 | 2.33 | 3.50 | 2.76 | 2.75 | .216 |
| Lack of multidisciplinary communication with other specialties involved in these patient profiles | 2.47 | 2.83 | 2.00 | 2.71 | 2.64 | 1.75 | 2.33 | 3.08 | 2.24 | 2.38 | .113 |
| Other | 2.61 | 3.67 | 3.00 | 2.50 | 1.00 | 1.00 | 1.50 | 1.00 | 2.50 | 3.20 | .488 |
PCP: Primary Care Physician.
Ninety-seven specific strategies were defined for the follow-up of PsA patients and 11 for SpA (spondyloarthritis) patients, of which 64 (84%) and 10 (91%) were agreed respectively (Table 3). Of all of the strategies, 52 were considered highly advisable in the follow-up of the PsA patient (Table 4). In general, there were no significant differences in consensus in the different regional areas (supplementary Appendix B Material 2).
Consensus reached in each wave. Results of Delphi study
| Strategies for the follow-up of PsA | |||||||
|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | ||||||
| Totala | General | PsA | General | PsA | |||
| Total strategies | 202 (100%) | 11 (100%) | 97 (100%) | 202 (100%) | 11 (100%) | 97 (100%) | |
| Consensus reached (≥70% agreement) | 154 (76%) | 10 (91%) | 76 (81%) | 171 (85%) | 10 (91%) | 64 (84%) | |
| Consensus in agreement | 154 (76%) | 10 | 76 (81%) | 171 (85%) | 10 | 64 84%) | |
| Consensus in disagreement | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Consensus not reached (<70% agreement) | 48 (24%)b | 1 (9%) | 21 (22%) | 31 (15%) | 1 (9%) | 11 (12%) | |
PsA: Psoriatic arthritis.
Highly desirable strategies for the follow-up of PsA patients. Results of the Delphi consensus
| In disagreement | Neutral | In agreement | ||
|---|---|---|---|---|
| Frequency | (1-2-3) | (4-5-6) | (7-8-9) | |
| Quality of life/disease activity indices | ||||
| Assess at least one quality of life index, at least annuallya | 1.10% | 4.30% | 94.60% | |
| Patient Global Assessment (PtGA) at each visit | 4.70% | 15.30% | 80.00% | |
| Physical examination and metrology | ||||
| Hip examination, at least once a year | 2.40% | 4.70% | 92.90% | |
| At each visit | Perform a tender/swollen joint count (66/68) at each visit | 3.50% | 5.90% | 90.60% |
| Skin and nail assessment, at each visit | 2.40% | 8.20% | 89.40% | |
| Perform an enthesitis count at each visit | 2.40% | 9.40% | 88.20% | |
| Perform a specific dactylitis count, at each visit, and record separately from joint count | 2.40% | 9.40% | 88.20% | |
| Ask about history of red eye, at each visit | 2.40% | 17.60% | 80.00% | |
| Hip examination at each visit | 9.40% | 11.80% | 78.80% | |
| Assessment of comorbidities and extra-articular manifestations | ||||
| Assess cardiovascular risk factors, regardless of whether the assessment is by the rheumatology department, nurse, or from primary carea | .00% | 1.20% | 98.80% | |
| Having a nurse who assesses cardiovascular risk factors (weight, height, BMI, blood pressure)a | .00% | 5.90% | 94,10% | |
| Review the patient’s medical history at each visit, to assess comorbidities, even if the patient is not directly asked in the consultationa | 1.20% | 8.20% | 90.60% | |
| At least once a year | Blood pressure | .00% | 2.40% | 97.60% |
| Weight/height/BMI | .00% | 3.50% | 96.50% | |
| Non-alcoholic fatty liver disease | 1.20% | 4.70% | 94.10% | |
| Abdominal circumference | .00% | 9.40% | 90.60% | |
| At each visit, through history taking | Cardiovascular disease | 3.50% | 10.60% | 85.90% |
| Dyslipidaemia | 3.50% | 10.60% | 85.90% | |
| Diabetes mellitus | 3.50% | 11.80% | 84.70% | |
| Kidney failure | 3.50% | 12.90% | 83.50% | |
| High blood pressure | 3.50% | 12.90% | 83.50% | |
| Obesity/overweight | 3.50% | 12.90% | 83.50% | |
| Non-alcoholic fatty liver | 3.50% | 15.30% | 81.20% | |
| Metabolic syndrome | 4.70% | 15.30% | 80.00% | |
| Smoking | 5.90% | 15.30% | 78.80% | |
| Uveitis (confirmed by an ophthalmologist) | 3.50% | 17.60% | 78.80% | |
| Sedentary lifestyle, amount, and type of exercise | 4.70% | 17.60% | 77.60% | |
| Inflammatory bowel disease (UC and Crohn’s) | 3.50% | 20.00% | 76.50% | |
| Alcohol | 5.90% | 18.80% | 75.30% | |
| Depression/anxiety | 4.70% | 20.00% | 75.30% | |
| Gastric ulcer | 9.40% | 20.00% | 70.60% | |
| Disease activity and function indices | ||||
| Promote the role of rheumatology specialist nurses to increase the use of disease activity and function indicesa | .00% | 2.40% | 97.60% | |
| At each visit | Pain VAS (0-1) | 1.20% | 7.10% | 91.80% |
| Patient global VAS | 1.20% | 7.10% | 91.80% | |
| Physician global VAS (0-1) | 2.40% | 7.10% | 90.60% | |
| DAPSA | 2.40% | 9.40% | 88.20% | |
| Regarding skin assessment of the PsA patient: | ||||
| It is highly advisable to perform a skin assessment together with the dermatologist in cases of moderate or severe skin involvement | 3.50% | 9.40% | 87.10% | |
| It is highly advisable to perform a skin assessment at each visit | 1.20% | 12.90% | 85.90% | |
| Assessment with PASI should have been done by dermatology, in cases of moderate or severe skin involvement | 1.20% | 12.90% | 85.90% | |
| If the dermatologist has already assessed skin involvement, it is advisable to perform a BSA. If not done by dermatology, it is highly advisable to perform a BSA | 2.40% | 16.50% | 81.20% | |
| PASI could be dispensed with if BSA is already performed | 3.50% | 23.50% | 72.90% | |
| If BSA is not available, and there has been no skin assessment by dermatology, PASI assessment is highly advisable | 12.90% | 14.10% | 72.90% | |
| Laboratory tests | ||||
| At each visit | C-reactive protein | .00% | 2.40% | 97.60% |
| Blood count | .00% | 2.40% | 97.60% | |
| General biochemistry with liver profile | .00% | 2.40% | 97.60% | |
| Creatinine clearance/filtrate (MMDR-4) | .00% | 11.80% | 88.20% | |
| Erythrocyte sedimentation rate | 5.90% | 11.80% | 82.40% | |
| Every 6-12 months | Lipid profile, every 6-12 months, according to risk profile | .00% | 2.40% | 97.60% |
| Uric acid 6-12 months | 1.20% | 4.70% | 94.10% | |
| Urine analysis, at least once a year | 1.20% | 7.10% | 91.80% | |
| Imaging tests | ||||
| Peripheral X-rays of hands and feet if there are symptoms | 2.40% | .00% | 97.60% | |
| Perform at least one baseline X-ray of the lateral cervical and/or dorsal and/or lumbar spine | 2.40% | 7.10% | 90.60% |
AxSpA: Axial spondyloarthritis; BMI: Body Mass Index; DAPSA: Disease Activity in psoriatic Arthritis Index; PASI: Psoriasis Area Severity Index; PsA: Psoriatic arthritis; UC: Ulcerative colitis; VAS: Visual Analogue Scale.
Of the participants, 80% considered it highly advisable to assess at each visit the patient's global status using the PtGA; 94.6% agreed that assessing QoL by a specific index once a year is highly advisable.
It was considered highly advisable to perform hip examination at least once a year and, at each visit, swollen or tender joint count, enthesitis count, dactylitis count with a separate recording of joint count, skin and nail assessment, and assess for a history of red eye.
It was considered highly advisable to assess cardiovascular risk factors in patients with PsA, and appropriate nursing staff for this role was also considered highly desirable. It was determined that extra-articular manifestations and comorbidities should be assessed at each visit. Weight, height, BMI, abdominal circumference, blood pressure, and onset of fatty liver should be determined annually.
Global and pain VAS assessment was recommended at each visit, and calculation of DAPSA. Skin assessment at each visit was also recommended, preferably in conjunction with dermatology in moderate or severe cases. It was agreed that PGA × BSA should be assessed by the dermatology specialist.
It was considered highly advisable to determine C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), blood count, general biochemistry with liver profile, and creatinine clearance, or glomerular filtration rate at each visit; lipid profile and uric acid should be determined every 6 to 12 months.
A baseline cervical / dorsal / lumbar lateral spine X-ray was considered highly advisable. Peripheral X-rays of hands and feet were considered necessary, based on symptoms.
DiscussionThe optimal follow-up of patients with PsA is a broad and complex process. Although new therapeutic options have emerged in recent years, there is still room for improvement in quality of patient care in terms of diagnosis, referral, initiation of treatment. and follow-up, which may affect the clinical outcomes and QoL of patients in the long term18.
Lack of resources in clinical practice is undoubtedly a limiting factor for the comprehensive follow-up of patients with PsA. This study presents a total of 52 strategies agreed as highly advisable, which form a minimum action framework and ensure optimal follow-up, even in a setting with a high care burden, limited consultation time, and lack of resources. Furthermore, these strategies are applicable to the entire country, as no significant differences were found in the degree of consensus by region. These recommendations are aimed at all experts involved in the care of patients with PsA: rheumatologists, rheumatology nurses, primary care physicians, and dermatologists. They may also be of use to government and hospital managers, patient organisations, and regulatory agencies.
In the first phase of this study, lack of consultation time, lack of nursing and/or support staff, and delayed imaging tests were identified as major limitations in the follow-up of patients with PsA. There was some disparity between the desired time for first and follow-up visits and the time actually dedicated by the experts.
Given that one in four participants stated that rheumatology nurses were not available and that the positive impact of rheumatology nurses on rheumatology services and patients has been demonstrated19,20, it was recommended that their role be enhanced to increase the use of activity and function indices, support patients in completing QoL and patient-reported outcome questionnaires, and assess comorbidities (CV risk factors, depression, etc.).
The high comorbidity associated with PsA and the consequent impact on its sufferers have led to the development of recommendations for its identification, assessment, and management21. Some of the highly recommended strategies offered in this study aim to identify comorbidities such as cardiovascular or metabolic diseases, and extra-articular manifestations. It is also vitally important to promote multidisciplinary management and to optimise system efficiency, patient care, and collaboration between dermatologists and rheumatologists22. At national level, existing models of multidisciplinary care and the corresponding standards of care and quality indicators have been defined13. However, their degree of implementation has also been described as heterogeneous and insufficient14. In particular, the role of the dermatologist is crucial in certain aspects, such as early detection of the disease23 and the existence of multidisciplinary dermatology-rheumatology units has been considered a criterion of excellence.14 In the study presented, these were also considered to play an indispensable role in the skin assessment of PsA, especially in patients with moderate or severe involvement.
As the goal of PsA treatment is to eliminate inflammation and optimise functional capacity and QoL10, disease activity and patient status should be assessed on a regular basis and therapy adjusted appropriately. Nationally, it has been observed that assessment using indices of joint involvement and function is not recorded in a significant number of medical records24. In the current study, more than one third of participants did not use the DAPSA index, despite its proven usefulness11,25,26, and one in 10 did not use global and pain VAS assessment, although both assessments were considered necessary at each visit. The PsAID questionnaire is the only validated tool to collect information on the impact of the disease on the patient's health status based on all the domains considered relevant according to the patients with PsA27. They are also, together with the DAPSA, considered the most appropriate tools for assessing response to biologic treatments 3 months after the start of treatment17. Even so, almost 3 out of 4 participants stated that they did not use it, which shows that there is room for improvement in its implementation. Digital databases for recording the assessment of patients with PsA could be tools to facilitate joint assessment (activity, function, skin involvement, QoL) although, according to the results shown, they are not available in more than half of cases.
The standards for the follow-up of patients with PsA described here should be disseminated among the professionals involved in their care, so that they can adapt them to the characteristics of their hospitals, claim the necessary resources, increase the multidisciplinary approach, and help in the control of the disease, and the prevention of associated comorbidities. Certain healthcare quality standards28 have also been published that may be useful for organising activity in rheumatology outpatient departments and for submitting proposals for improvement to hospital management or other administrative bodies. Furthermore, PsA patients should be able to understand the purpose of such an exhaustive and time-consuming assessment, although the development of tools to reduce patient consultation time is desirable. There has also been increased use of telemedicine in recent years, accelerated by the COVID-19 pandemic, in the field of rheumatology, and new tools are being developed29, and standards for their development and implementation30.
The present study has limitations. Firstly, it is an opinion survey and not a study based on a review of patient records. The representativeness of the sample of participants in the Delphi consensus is not assured. Although experts were selected from the different regions of the country, it was not conducted homogeneously, which may limit the ability to detect differences between regions.
ConclusionsThe highly advisable strategies proposed in the CREA study respond to the unmet needs detected in the national survey and discussed in the regional meetings, which were subsequently agreed upon by a large group of rheumatologists. These strategies involve the promotion of multidisciplinary management with dermatologists playing a major role in the skin assessment of these patients and rheumatology nurses in assessing activity and function indices, supporting patients in completing QoL questionnaires and, assessing comorbidities (CV risk factors, depression, etc.). Thus, resources can be freed up to focus on physical examination, identification, and management of comorbidities and extra-articular manifestations, and ensure the most individualised treatment possible in each case. The data from this study also reveal that a significant proportion of rheumatologists are currently not using the recommended activity indices. The strategies proposed in this study would optimise the efficiency of the system and result in better patient care. These strategies are applicable nationwide, form a minimum action framework, and ensure optimal follow-up of patients with PsA.
FundingNovartis Farmacéutica S.A financially supported the development of this Project, medical writing assistance and journal processing fees for this article.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all the expert rheumatologists who participated in the regional meetings: Adela María Gallego Flores, Agustí Sellas i Fernández, Agustín Javier Alegre López, Alfonso Fernando Corrales Martínez, Ana Lafont Ruzafa, Ana Pérez Gómez, Ana Urruticoechea Arana, Àngels Martinez Ferrer, Antonio Álvarez de Cienfuegos Rodríguez, Antonio Juan Mas, Arantxa Conesa Mateos, Azucena Hérnandez Sanz, Beatriz González Álvarez, Carlos Alberto Montilla Morales, Carlos García Porrúa, Carlos Javier Rodríguez Lozano, Carlos Manuel González Fernández, Cristina Campos Fernández, Cruz Fernández, Delia Reina Sanz, Elisa María Trujillo Martín, Emma Beltrán Catalán, Erardo Ernesto Meriño Ibarra, Francisco José Maceiras Pan, Gloria Candelas Rodríguez, Jaime Calvo Alën, Javier Calvo Catalá, Jesús Rodríguez Moreno, José Ángel Hernández Beriain, José Antonio Mosquera Martínez, José García Torón, José Miguel Senabre Gallego, José Ramón Maneiro Fernández, Juan Moreno Morales, Laura González Hombrado, Luis Espadaler Poch, Luis Fernández Domínguez, Luis Francisco Linares Ferrando, Manuel José Moreno Ramos, María Concepción Castillo Gallego, María Cristina Lerin Lozano, María José Moreno Martínez, María Luz García Vivar, María Paz Martínez Vidal, Marta Valero Expósito, Meritxell Fernández Matilla, Mireia Moreno Martínez-Losa, Olga Sánchez González, Raquel Hernández Sánchez, Ricardo Gutiérrez Polo, Sara Manrique Arija, Sergio Antonio Rodríguez Montero, Sergio Ramon Machin García, Teresa Font Gayá, Tomás Ramón Vázquez Rodríguez, Vicente Aldasoro Cáceres, Yolanda Cabello Fernández, Julio Antonio Medina Luezas, Isabel de la Morena Barrio and José Campos Esteban.