Soft tissue infection due to Mycobacterium tuberculosis can affect muscle, tendons, fascia, bursa and synovial tissue. Tuberculous trochanteric bursitis is a rare entity that usually affects immunocompromised patients. Manifestations usually occur insidiously, which delays diagnosis and treatment. We present the case of an immunocompetent young woman who came to our department for chronic left hip pain. The study confirms the diagnosis of tuberculous trochanteric bursitis. This case demonstrates the importance of considering a possible infectious origin of bursitis in immunocompetent patients.
La infección de tejidos blandos por Mycobacterium tuberculosis puede afectar al músculo, tendones, fascia, bursa y tejido sinovial. La bursitis trocantérea de origen tuberculoso es una entidad infrecuente, que suele afectar a pacientes inmunocomprometidos. Se manifiesta habitualmente de forma insidiosa, lo que dificulta el diagnóstico y retrasa el tratamiento. Se presenta el caso de una mujer joven, inmunocompetente, que acudió a nuestro servicio por dolor crónico de cadera izquierda. El estudio realizado confirmó el diagnóstico de bursitis trocantérea tuberculosa. Este caso demuestra la importancia de considerar el posible origen infeccioso de las bursitis en pacientes inmunocompetentes.
We present the case of a 35-year-old woman who presented pain in the left trochanter region with functional limitation, which had lasted for 6 months. The patient only had a history of exposure to a person diagnosed as infected with tuberculosis 7 years prior to the onset of symptoms. Then, and due to positive tuberculin test, in the absence of symptoms or radiological abnormalities, she completed prophylaxis with isoniazide for 6 months, remaining asymptomatic afterward and with no high-risk contact with TB.
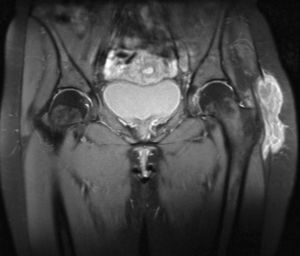
At the moment of the consultation she presented inflammatory pain in the left peritrochanteric region, which extended to the gluteus, the inguinal area and the knee, limiting movement, without a history of trauma, fever or constitutional symptoms. Examination revealed an increase in soft tissue opacity in the area, with no other inflammatory signs, as well as marked limitation to active and passive mobilization of the coxofemoral joint in all planes of movement. There was no other joint affection or respiratory problems. Laboratory testing revealed leukocytes of 13000/μl and erythrocyte sedimentation rate of 35mm in the first hour. Mantoux test was positive. A chest X-ray was normal. Imaging (Fig. 1) of the hip revealed an increase in soft tissues in the left trochanter region, with no signs of bone affection. Ultrasound and magnetic resonance of the hip revealed trochanteric bursitis. A guided aspiration of the abscess was done using ultrasound and caseum like material was obtained. Culture of this revealed the presence of Mycobacterium tuberculosis.
After the diagnosis, treatment with isoniazide, riphampin and pyrazinamide was started and lasted 2 months, followed by combined isoniazide and riphampin treatment until completing 9 months. In spite of the adequate treatment compliance, the patient persisted with pain and functional limitation, and 4 months after treatment a surgical approach was opted for, draining the lesion and performing a trochanteric bursectomy. A year after treatment the patient remains asymptomatic.
DiscussionThe bursae are virtual cavities located in areas of friction, coated with synovial cells. Trochanteric bursitis can be of traumatic, postural, infectious, inflammatory, tumoral or idiopathic. In cases of infectious origin, dissemination may occur through the blood or by extension, from a contiguous infectious site. The predominant organisms are Gram-negative organisms, anaerobes and, in rare cases, mycobacteria (particularly M. tuberculosis). The cause of tuberculous bursitis in our patient remains unclear, as there was no evidence of hematogenous dissemination or local involvement due to proximity.
Extrapulmonary TB is usually diagnosed late due to a reduced diagnostic suspicion.1 Musculoskeletal manifestations occur in approximately 1%–5.2% of cases. Of these, arthritis and spondylitis are the most frequent, whereas bursitis and tenosynovitis are exceptional.2
Musculoskeletal TB is more common in immunosuppressed patients. Our case is an immunocompetent woman who was diagnosed with tuberculous bursitis years after the completion of prophylaxis. Musculoskeletal manifestations of M. tuberculosis usually present progressively,3 in the absence of fever and general symptoms. Tuberculous bursitis can be a sign of reactivation of the disease. The diagnosis is usually made in advanced stages by the presence of abscesses or fistulas.4 The CT or MRI scans help define their size and the existence of bone involvement. Cases of reactivation of TB even decades after tuberculostatic therapy5,6 have been described in the literature. The treatment of musculoskeletal manifestations in these cases is controversial.7,8 There is a high recurrence rate described in some series of patients treated only with TB drugs, making the surgical approach something that should be considered in all patients. In cases with extended trochanteric involvement, we recommend delaying surgery for several weeks while the patient receives antituberculous therapy to reduce the risk of dissemination of mycobacteria4 during surgery, as was done in the case presented.
In conclusion, this case illustrates that tuberculous bursitis can occur in isolation, without other systemic or musculoskeletal manifestations, and therefore should be considered in the differential diagnosis of the trochanteric bursitis.
DisclosuresThe authors have no disclosures to make.
Please, cite this article as: Soro Marín S, et al. Bursitis trocantérea tuberculosa en mujer joven inmunocompetente. Reumatol Clin. 2012;8(1):34–35.