Joint involvement is one of the initial manifestations in most patients with systemic lupus erythematosus (SLE); ranging from joint pain to severe deforming arthritis.1 Within the deforming types, non erosive forms, such as Rhupus and others such as Jaccoud's arthropathy (JA),2 non-erosive in principle, occurs in 10%–35% of patients with SLE.3
Ultrasound has proven superior to clinical examination in detecting joint and tendon inflammatory activity in patients with SLE.2 We report a patient with SLE and JA in which this technique was useful in the assessment of disease.
The patient is a 40-year-old woman from Honduras diagnosed with SLE 4 years prior and, has presented during her evolution, joint pain and arthritis of small proximal joints of the hands, wrists, knees and elbows; scarring alopecia; Raynaud's phenomenon and subacute cutaneous lupus erythematosus lesions. She had positive antinuclear antibodies (1/1280), anti-dsDNA, anti-Sm, anti-RNP and anti-CCP (high titers); anemia of chronic diseases and complement consumption. From the onset of the disease she has been treated with hydroxychloroquine, methotrexate and prednisone. Currently, she is painless and has non reducible deformity of the hands, bilaterally, with a positive score (more than 5 points) for JA in the index proposed by Spronk et al.,3 with predominating “gooseneck” deformities, evident ulnar deviation in some fingers and unilateral thumb ‘Z’ deformity (Fig. 1). Despite being asymptomatic, C-REACTIVE protein (CRP) and erythrocyte sedimentation rate remained persistently positive, so an ultrasound of the wrists and hands was requested, after ruling out infections or other concurrent processes.
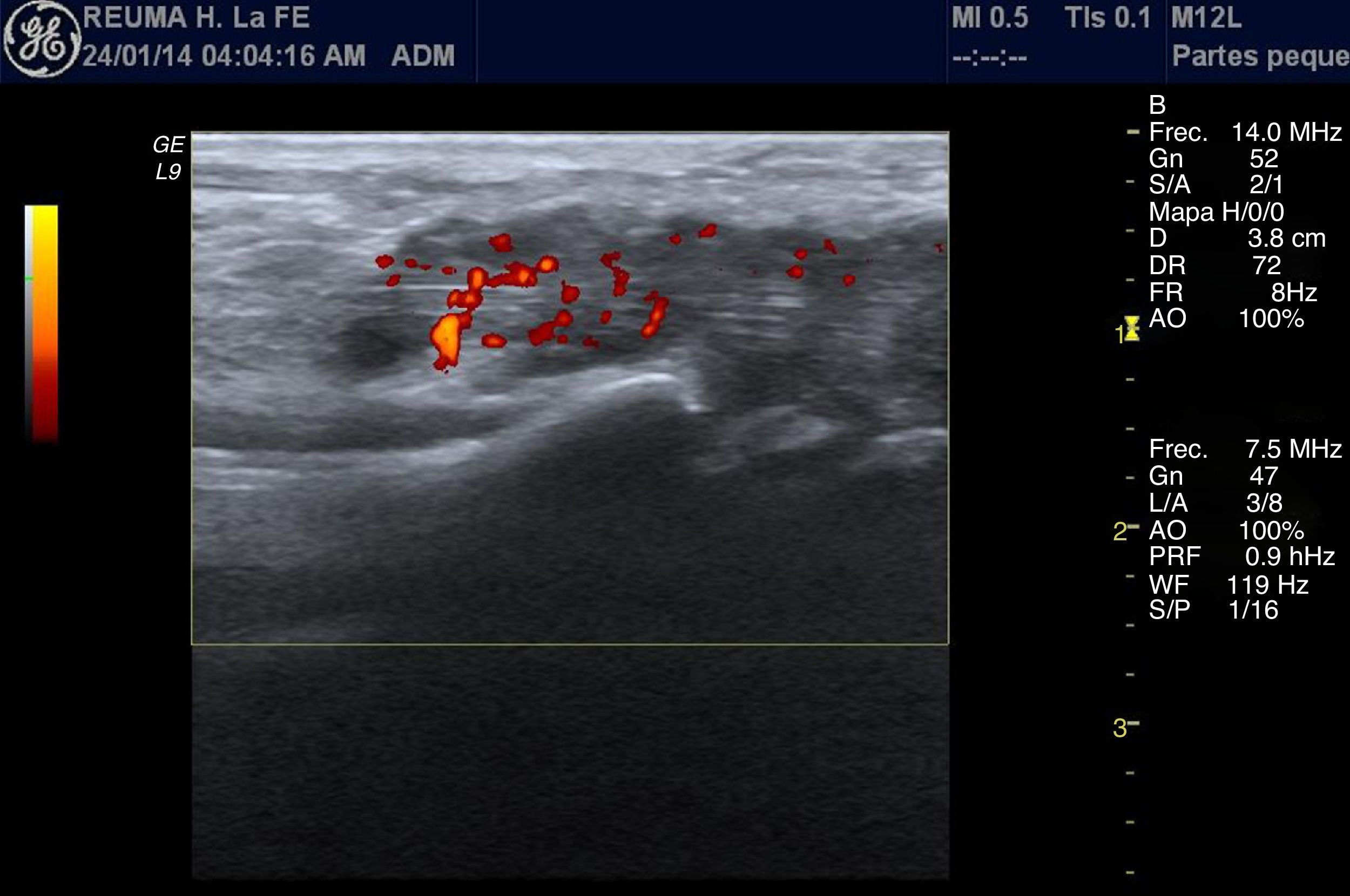
Synovial hypertrophy was observed in the radiocarpal and midcarpal joints bilaterally, according to the Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT). It is described as an abnormal non-movable, intraarticular hypoechoic tissue, poorly compressible,4 2nd stage,5 because it reached the top of the periarticular bone and did not extend to the diaphysis. The power Doppler signal was 26 as confluent vascular signals were observed in the synovial area. Flexor tenosynovitis was also shown on the wrist, corresponding to a hypoechoic thickening of the synovial sheaths of the tendons5 with bilateral pathological Doppler (Fig. 2) signal corresponding to an increase of normal vascularization. Similarly, tenosynovitis was seen in all finger flexors with no evidence of bone erosions.
Longitudinal view of the palmar radiocarpal joint, in which the flexor tendons of the wrist are appreciated. A hypoechoic thickening of the synovial sheaths of the tendons is highlighted, corresponding to tenosynovitis with marked synovial hypertrophy and a pathological Doppler signal, which shows an increase of normal vasculature.
JA is a chronic deforming joint affection,7,8 associated with different diseases9 which usually affects the metacarpophalangeal and proximal interphalangeal joints, wrists and knees.1 It leads to deformities that mimic rheumatoid arthritis (RA), predominantly dislocations, although with little pain and little functional impairment. Alterations are reducible9 and not the typical radiographic erosions seen in RA,2 even in patients with longstanding MR studied disease.1
We hypothesize that tenosynovitis is a typical primary lesion1 and deformities result from the involvement of ligaments and tendons, rather than an erosive arthritis with pannus formation, as in RA.2
In our patient, antiphospholipid antibodies were negative, contrary to the previously suggested association9 and she showed no renal involvement. There is a negative association between JA and kidney damage, despite the prevalence of anti-dsDNA antibody, suggesting a better prognosis in these patients.9
The acute phase reactants and ultrasound abnormalities point to sustained synovial inflammation, consistent with previous publications3 in which higher CRP levels were observed in patients with JA compared with patients without it, despite a similar clinical situation and treatment.
We agree with other groups, on the importance and value of ultrasonography in patients with SLE2 although it is still not validated as an imaging technique for the assessment of lupus. In our case, it allowed us to detect elementary lesions suggestive of active inflammation, although the patient remained clinically asymptomatic. These alterations detected by ultrasound show, with great probability, subclinical tendon involvement due to the disease, similar to what has been suggested in other studies in patients with lupus, but without reference to JA.10 Nevertheless, more studies are needed to assess the need for a screening ultrasound or other imaging techniques in all patients with JA, or only those who remain with elevated acute phase reactants, looking for signs of inflammatory activity.
Please cite this article as: Feced Olmos CM, Ivorra Cortés J, Negueroles Albuixech R, Román Ivorra JA. La ecografía en la artropatía de Jaccoud. A propósito de un caso. Reumatol Clin. 2015;11:127–129.