The term “autoimmune/inflammatory syndrome induced by adjuvants” (ASIA) describes a variety of autoimmune conditions triggered by exposure to substances with adjuvant activity. We present the case of a patient with a history of biopolymer infiltration in both glutes, who years later experienced progressive weakness and pain in the lower limbs, myalgias, cramps, and progressive functional impotence following a mild COVID-19 infection. Laboratory test results were not consistent with any autoimmune disease. Physical examination revealed diffuse bilateral subcutaneous nodules. After an extensive etiological study, a gluteal biopsy was performed, which showed findings compatible with sclerosing lipogranuloma. Our patient required treatment with high-dose glucocorticoids and showed significant improvement in symptoms during long-term follow-up. We suggest the role of COVID-19 infection as a possible trigger for ASIA, as it has already been described as a trigger for several other autoimmune diseases.
El término «síndrome autoinmune/inflamatorio inducido por adyuvantes» (ASIA) describe una variedad de condiciones autoinmunes desencadenadas por la exposición a sustancias con actividad adyuvante. Presentamos el caso de una paciente con antecedentes de infiltración de biopolímeros en ambos glúteos que años más tarde experimentó debilidad progresiva y dolor en extremidades inferiores, mialgias, calambres e impotencia funcional progresiva después de una infección leve por COVID-19. Los resultados de los análisis de laboratorio no sugerían enfermedad autoinmune. El examen físico reveló nódulos subcutáneos difusos bilaterales. Después de un extenso estudio etiológico, se realizó una biopsia glútea, la cual mostró hallazgos compatibles con lipogranuloma esclerosante. La paciente requirió tratamiento con glucocorticoides a dosis altas y mostró una mejora significativa en los síntomas durante el seguimiento a largo plazo. Sugerimos el papel de la infección por COVID-19 como posible desencadenante de ASIA, ya que se ha descrito como desencadenante de otras enfermedades autoinmunes.
“Autoimmune/inflammatory syndrome induced by adjuvants” (ASIA) describes an autoimmune or autoinflammatory disease triggered by exposure to compounds that have adjuvant properties.
ASIA is defined as fatigue, muscle and joint discomfort, neurological impairment, and cognitive disorders with the possible appearance of autoantibodies. ASIA is thought to occur when the immune system overreacts with the adjuvant, resulting in variable latency.
We report a case of ASIA more than 15 years after esthetic gluteal injections of biopolymers, triggered after COVID-19 infection.
Clinical observationA 50-year-old woman, native of Ecuador, was affected by well-controlled HIV diagnosed 22 years ago with emtricitabine/rilpivirine/tenofovir and underwent bilateral gluteal injection of biopolymers 15 years ago. She presented 3 months-progressive weakness and pain in the lower limbs, myalgia, and progressive functional impotence, which started 3 weeks after mild COVID-19 infection.
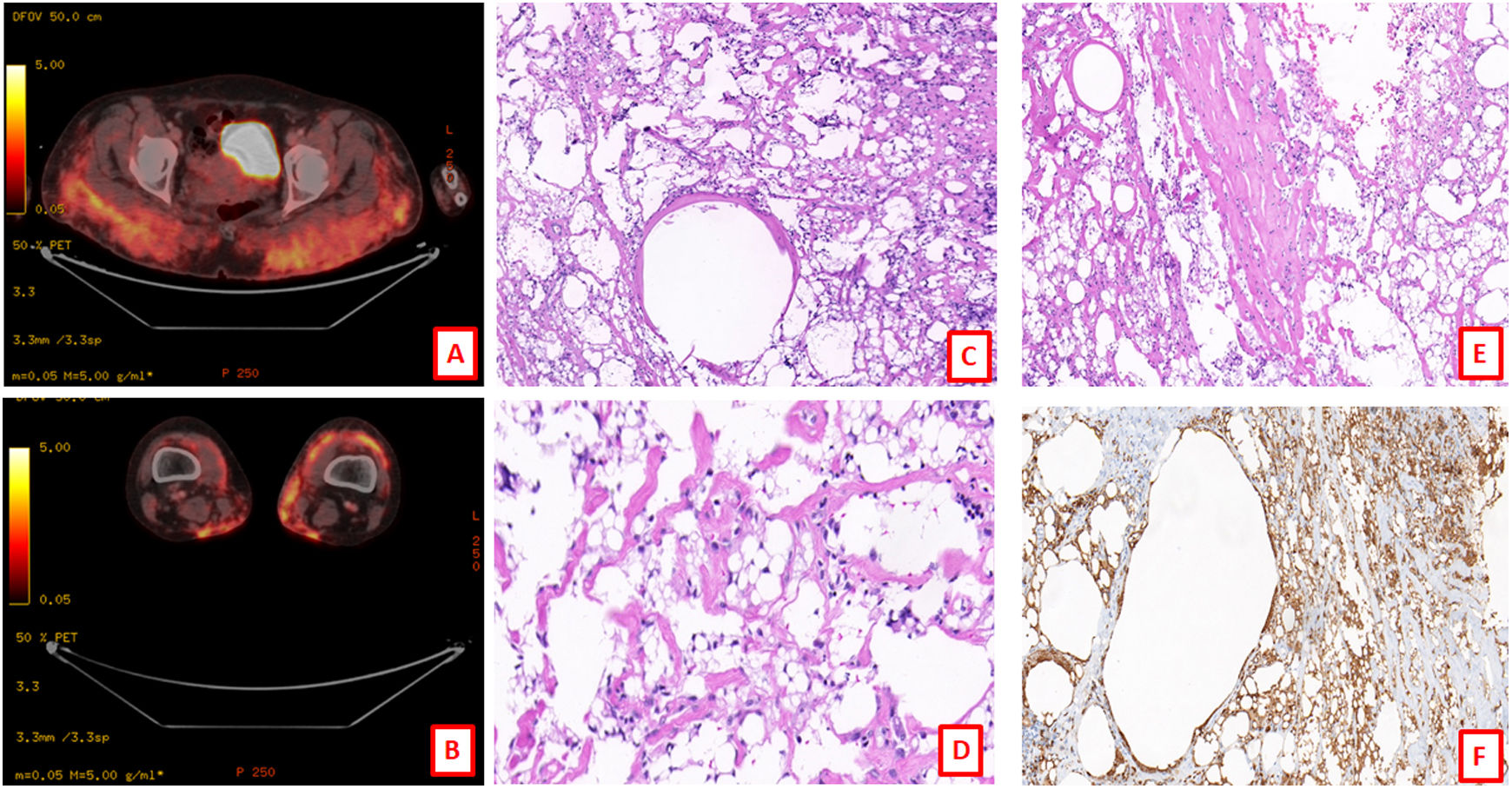
On physical examination, she presented diffuse nodules of soft consistency in both thighs. Laboratory, serological, and immunological tests revealed no abnormalities. No signs of myopathy or neuropathy were observed on the electromyography. Nuclear magnetic resonance imaging revealed a large infiltration and diffuse subcutaneous and intramuscular nodular images in both gluteal regions related to injectable material located in the subcutaneous cellular tissue. Positron emission tomography imaging revealed an inflammatory tissue reaction to biopolymers at the lower lumbar level and gluteal area, with migration of the material to the lower extremities (Fig. 1: A, B). A gluteal biopsy showed granulomatous inflammation with cystic spaces of different sizes, with fibrosis and necrosis compatible with sclerosing lipogranuloma (Fig. 1: C to F).
(A, B) PET-CT showing inflammatory tissue reaction to synthetic macromolecules at the lower lumbar level and gluteal area, with probable migration of the same to lower extremities and right anterior rectus muscle. (C) Membrano-cystic bodies formed by lipid vacuoles and surrounded by giant cells (HE ×100). (D, E) Fibrosis and steatonecrosis (HE ×100). (F) Immunohistochemistry with CD68 antibody marking histiocytes and giant cells surrounding membrano-cystic bodies (HE ×100).
A diagnosis of autoimmune/inflammatory syndrome induced by adjuvants, possibly triggered by a COVID-19 infection, was finally made.
The patient showed a good clinical evolution after treatment with prednisone 60mg/d (with a subsequent rapid descent sequence up to 5mg/d) and hydroxychloroquine 200mg/12h during long-term follow-up. The patient was referred for biopolymer removal.
DiscussionVarious adjuvant-induced diseases have been widely described as ASIA. These adjuvant substances are used in vaccines, silicone implants, and other medical or nonmedical products that are capable of enhancing antigen-specific immune responses.1,2
The most frequent manifestations are erythema, hyperpigmentation, or changes in skin texture. One or more deep, irregular, firm nodules, sometimes fluctuating or ulcerated, can appear at injection sites in the case of esthetic materials.3
A wide range of autoimmune conditions, including systemic lupus erythematosus and rheumatoid arthritis, has been described at the systemic level. Systemic granulomatous reactions, such as acute pneumonitis or granulomatous hepatitis, have also been documented, although the process by which these processes develop remains unclear.2
The diagnosis of ASIA is based on the precedent of contact with any adjuvant substance and confirmed by histopathology, with multiple cystic spaces, dense fibrous tissue, inflammatory phagocytic cells, and chronic granuloma.3–5
The treatment is based on the elimination of external stimuli, and in most cases, a favorable long-term response is observed without immunomodulatory treatment. However, in cases of evolution to well-defined autoimmune/autoinflammatory diseases, it is necessary to initiate immunomodulatory treatment. Long-term prognosis has not yet been evaluated. However, the existing recommendation is to avoid further exposure to the adjuvant involved because of the theoretical risk of re-triggering or exacerbating the immune response.3
It is typical for infectious pathogens to activate autoimmune pathways,6 and COVID-19 infection has been proposed as a possible inducer of autoimmune disease.
To our knowledge, this is the first reported case of ASIA triggered by COVID-19 infection.
ConclusionsASIA is a rare disease that should be suspected in patients exposed to esthetic biopolymers. It remains a challenging diagnosis, and infections such as COVID-19, may trigger hyperactive immune responses in patients previously exposed to adjuvants.
Ethical considerationsFor the completion of this article, the ethics committee of our hospital approved the data collection, and there is a signed consent form from the patient.
FundingThere has been no funding for the completion of this article.
Conflict of interestThe authors declare that there are no conflicts of interest or personal relationships that could have influenced the work presented in this article.