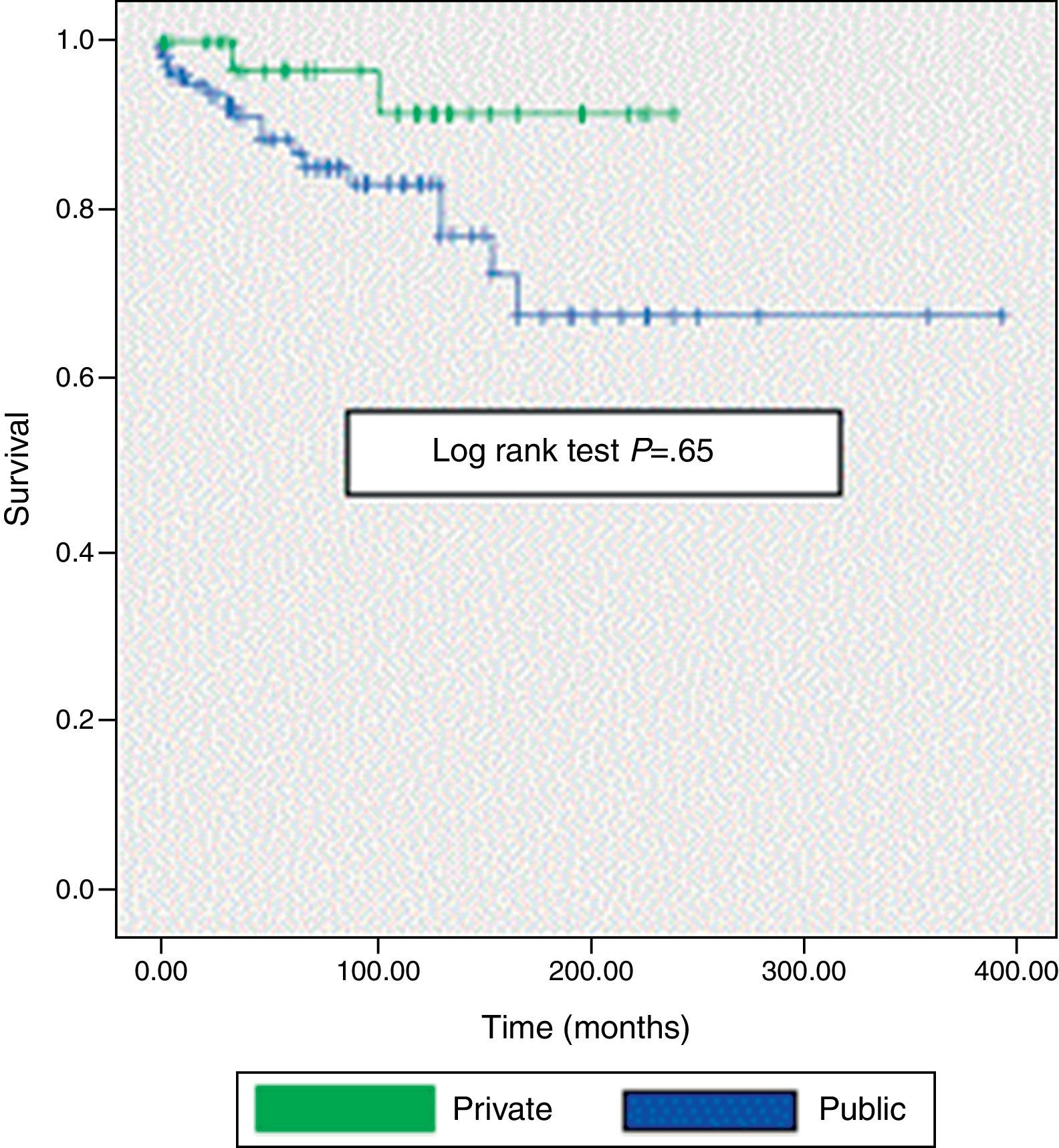
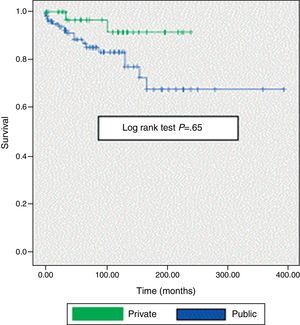
The study includes 159 SLE patients seen between 1987 and 2011, of whom 116 were treated in the public health system and 43 in private practice. In the comparison between both groups, it was shown that patients in the public health system were younger at first consultation and at the onset of SLE, and that the mean duration of their disease prior to nephropathy was statistically significantly shorter. They also presented with more SLE activity (measured by Systemic Lupus Erythematosus Activity Index) such as fever, lower levels of C4, and elevated erythrocyte sedimentation rate. Although cyclophosphamide was administered more frequently to patients in the public health system group, there were no statistically significant differences in renal histological findings. A second renal biopsy was performed on 20 patients due to the presence of persistent proteinuria, peripheral edema, urinary casts, or because of previous defective renal specimens. The overall 10-year survival of the patients in the public health system was 78% compared to a survival rate of 91% for the patients in private practices. When survival was evaluated at 15 years, however, no differences were found (log rank test: 0.65). Patients from both public and private groups attended medical specialist practices and received early diagnoses and close follow-ups.
Se identificó a 159 pacientes con lupus eritematoso sistémico (LES) vistos entre 1987 y 2011. Ciento dieciséis fueron tratados en el sistema público de salud y 43 en el sistema privado. Ambos grupos fueron comparados, observando que los primeros tenían menor edad al momento de la primera consulta y al inicio del LES y menor duración de la enfermedad al momento de producirse la nefropatía de manera estadísticamente significativa. También mostraron mayor actividad del LES (medido por Systemic Lupus Erythematosus Activity Index), con presencia de fiebre, menor nivel de C4 y elevado valor de eritrosedimentación globular. La ciclofosfamida fue administrada con mayor frecuencia a los pacientes del sistema público, si bien no hubo diferencias en los hallazgos histológicos renales. En 20 pacientes se realizó una segunda biopsia renal debido a la presencia de proteinuria persistente, edema periférico y cilindros en orina, o por tener una mala muestra renal previa. La supervivencia a 10 años fue del 78% en los pacientes atendidos en el sistema público vs el 91% de aquellos atendidos en el sistema privado. No se hallaron diferencias estadísticamente significativas cuando la sobrevida se evaluó a 15 años (log rank test: 0,65). Ambos grupos de pacientes (tanto los del sistema público como los del sector privado) fueron atendidos por especialistas, quienes realizaron un diagnóstico temprano de la enfermedad, con un cuidadoso seguimiento.
Recent studies on systemic lupus erythematosus (SLE) who have placed special emphasis on trends in mortality and have reported a more favorable outcome, perhaps due to better knowledge of the disease, a more expert handling of it and the rational use of treatments. It is well documented that many changes in SLE are due to factors that influence patients, such as ethnicity, gender, education, treatment compliance and socioeconomic characteristics. Mortality exceeds 2 or 3 times the average for the general population and even the more favorable mortality trends, when present, cannot always be applied to some economically disadvantaged groups both in under developed as well as in developed countries.1
There is very little literature comparing the clinical presentation, laboratory data, treatments administered and survival of lupus patients, treated at a public hospital or a private hospital. Due to the substantial difference observed between the two, the objective of this study is to describe and compare the demographic characteristics, clinical manifestations, laboratory results, treatment, renal involvement and outcome of patients with SLE. These patients studied were selected from the Rheumatology Department of a public health system and a private practice rheumatology center in Santa Fe, Argentina.
The public health system in Santa Fe is subsidized by the provincial government. Patients can choose their doctors, where rheumatologists act as primary physicians. In turn, the public health system provides the patient possibilities for additional studies and pharmacological and non-pharmacological treatment (physiotherapy, physical therapy, etc.). The patient who chooses the public health system usually does not have health insurance. By contrast, the patient spontaneously consulting a private practice usually has health insurance or pays for medical attention. Health insurance will cover (partially or completely) the costs of ancillary studies (laboratory, imaging, etc.) and non-pharmacological and pharmacological treatment.
The objective was to compare the clinical presentation, laboratory data, treatments administered in the population and survival of lupus patients treated at a public hospital with a private hospital.
Materials and MethodsAn observational, retrospective and transversal study was performed, reviewing medical records of 10,750 Rheumatology Service, Hospital JM Cullen (public health system) and the Center for Rheumatology (private), identifying 159 patients with SLE (1982 ACR criteria)2 from 1987 to March 2011.Patients in both sectors were both from the inpatient and outpatient clinic, of similar proportions, regularly seen by the same team of doctors every 3 months.
Demographic variables such as gender, mean age at the time of the consultation and the diagnosis of SLE (years); SLE duration and follow-up time (in months); SLE activity (for Systemic Lupus Erythematosus Disease Activity Index [SLEDAI],3 considering activity as a score <1); clinical manifestations; laboratory data, urea and serum creatinine, proteinuria, blood count, serological parameters (FAN by HeP-2, nDNA [Crithidia Lucilliae]), decreased C3 and C4, the presence of anti-Ro and La, Sm, RNPn, anticardiolipin IgG and IgM, and lupus inhibitor were evaluated.
Public sector patients who had renal involvement were compared to those treated in private practice, analyzing renal biopsy histology (classified according to the World Health Organization, as amended in 1982)4 and evaluated by the same pathologist, comparing also renal function at the end of treatment, the renal outcome after treatment (according to whether renal function was normal, the presence of persistent proteinuria or ESRD, defined as the need for dialysis, transplantation or a diagnosis of chronic renal failure, defined as the presence of creatinine <1.5mg/dl on 2 opportunities separated by at least 3 months).
Use of antimalarials, steroids and immunosuppressants was recorded in patients and these identified as alive, dead (consigning cause of death) or lost to follow up, considering as such a patient who did not attend for a visit for one consecutive year to the study date.
Both public hospital and private practice patients were attended by the same group of physicians.
The study was approved by the Ethics Committee of the Hospital. No informed consent was required because of the anonymous nature of the study.
Statistical MethodsCategorical data was compared using the chi-square and Fisher's exact test. Continuous variables were evaluated using Student's t for large samples of similar variance and small samples were evaluated using the non-parametric Mann–Whitney test. Results are reported as ±standard deviations. Survival analysis was performed using the Kaplan–Meier curve. Survival distributions were compared using the log-rank test. A significance of α=0.05 was considered. The statistical analysis was done using SPSS18.0 software.
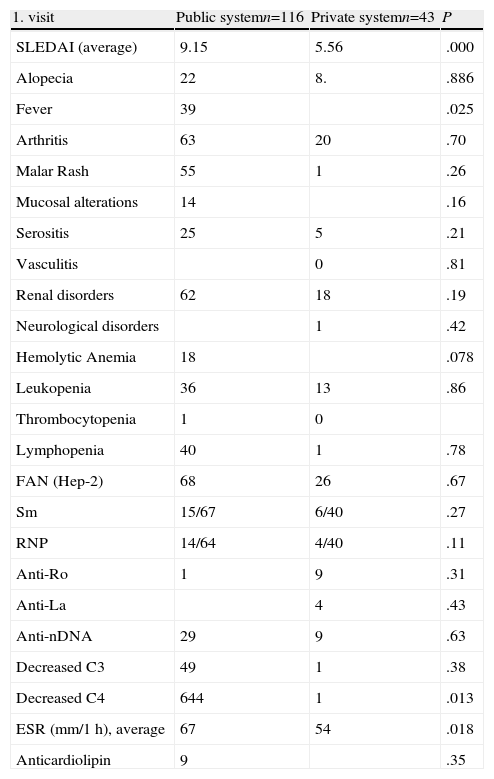
Results159 patients with SLE who fulfilled the 1982 ACR criteria were analyzed; 116 of them were treated in the public health system and 43 in private practice. When comparing both groups, we noted that the first had a lower age at first visit (28 vs 36 years, P=.001), younger age at onset of SLE (26 vs 32 years, P=.001) and a shorter evolution of SLE until the appearance of nephropathy in a statistically significantly manner (18 vs 41 months, P=.03). Furthermore, also during the first visit, we saw increased SLE activity demonstrated by SLEDAI, with fever, low C4 and elevated erythrocyte sedimentation value (ESR). There were no statistically significant differences between groups in relation to gender, the mean time from development of lupus to the first visit (Table 1) and treatment (steroid pulses, oral steroids, antimalarials, azathioprine and mycophenolate) except in the case of treatment with cyclophosphamide, which was mostly used in the hospital group (34% vs 14%, P=.008). The outcome was similar in both groups (10% died in the public sector vs 7% of those treated in the private sector, P=.14).
Clinical, Laboratory and Disease Activity in the First Patient Visit.
| 1. visit | Public systemn=116 | Private systemn=43 | P |
| SLEDAI (average) | 9.15 | 5.56 | .000 |
| Alopecia | 22 | 8. | .886 |
| Fever | 39 | .025 | |
| Arthritis | 63 | 20 | .70 |
| Malar Rash | 55 | 1 | .26 |
| Mucosal alterations | 14 | .16 | |
| Serositis | 25 | 5 | .21 |
| Vasculitis | 0 | .81 | |
| Renal disorders | 62 | 18 | .19 |
| Neurological disorders | 1 | .42 | |
| Hemolytic Anemia | 18 | .078 | |
| Leukopenia | 36 | 13 | .86 |
| Thrombocytopenia | 1 | 0 | |
| Lymphopenia | 40 | 1 | .78 |
| FAN (Hep-2) | 68 | 26 | .67 |
| Sm | 15/67 | 6/40 | .27 |
| RNP | 14/64 | 4/40 | .11 |
| Anti-Ro | 1 | 9 | .31 |
| Anti-La | 4 | .43 | |
| Anti-nDNA | 29 | 9 | .63 |
| Decreased C3 | 49 | 1 | .38 |
| Decreased C4 | 644 | 1 | .013 |
| ESR (mm/1h), average | 67 | 54 | .018 |
| Anticardiolipin | 9 | .35 |
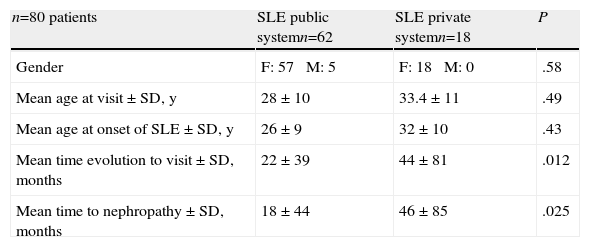
Lupus patients with renal disease were then compared, the public health system vs those seen in the private sector, finding no statistically significant differences in relation to gender, mean age at the time of consultation and the mean age at onset of SLE. It was observed that hospital patients with renal involvement consulted earlier than those treated in the private sector and had less time evolution of the underlying disease until renal involvement developed (P=.012 and .025, respectively) (Table 2).
Demographics of Patients With Renal Involvement in the Public System vs the Private System.
| n=80 patients | SLE public systemn=62 | SLE private systemn=18 | P |
| Gender | F: 57 M: 5 | F: 18 M: 0 | .58 |
| Mean age at visit±SD, y | 28±10 | 33.4±11 | .49 |
| Mean age at onset of SLE±SD, y | 26±9 | 32±10 | .43 |
| Mean time evolution to visit±SD, months | 22±39 | 44±81 | .012 |
| Mean time to nephropathy±SD, months | 18±44 | 46±85 | .025 |
SD, standard deviation; F, female; SLE, systemic lupus erythematosus; M, male.
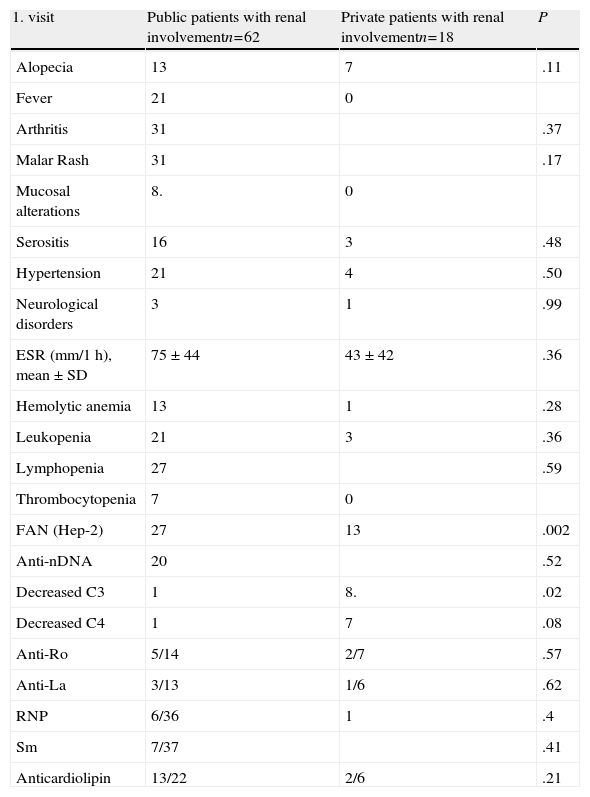
When clinical symptoms, laboratory and activity was measured by SLEDAI in SLE, patients with renal involvement seen in the public health system (n=62) were compared vs those treated in private (n=18), no significant differences in relation to the clinical manifestations were found. There were differences with respect to the activity of SLE at the first visit in the public system (SLEDAI 12.5 vs 6.33, P=.024), higher proportion of FAN (+) (27 vs 13, P=.002) and consumption of C3 (11 vs 8 patients) than patients in private practice (Table 3). However, no differences were found in relation to the histological type of renal injury, with types III and iv constituting 51% of samples from patients in the public sector and 60% of those treated in private practice. In 20 patients (16 public and 4 private) a second renal biopsy due to the presence of persistent proteinuria (13 patients), peripheral edema,1 casts,1 or a poor prior biopsy3 was performed. In 2 patients the data was not available. Again, the most prevalent type was diffuse proliferative nephritis.
Clinical, Disease Activity and Laboratory Data From Patients With Renal Impairment in the Public System vs the Private System.
| 1. visit | Public patients with renal involvementn=62 | Private patients with renal involvementn=18 | P |
| Alopecia | 13 | 7 | .11 |
| Fever | 21 | 0 | |
| Arthritis | 31 | .37 | |
| Malar Rash | 31 | .17 | |
| Mucosal alterations | 8. | 0 | |
| Serositis | 16 | 3 | .48 |
| Hypertension | 21 | 4 | .50 |
| Neurological disorders | 3 | 1 | .99 |
| ESR (mm/1h), mean±SD | 75±44 | 43±42 | .36 |
| Hemolytic anemia | 13 | 1 | .28 |
| Leukopenia | 21 | 3 | .36 |
| Lymphopenia | 27 | .59 | |
| Thrombocytopenia | 7 | 0 | |
| FAN (Hep-2) | 27 | 13 | .002 |
| Anti-nDNA | 20 | .52 | |
| Decreased C3 | 1 | 8. | .02 |
| Decreased C4 | 1 | 7 | .08 |
| Anti-Ro | 5/14 | 2/7 | .57 |
| Anti-La | 3/13 | 1/6 | .62 |
| RNP | 6/36 | 1 | .4 |
| Sm | 7/37 | .41 | |
| Anticardiolipin | 13/22 | 2/6 | .21 |
Requirements of oral or intravenous steroids, antimalarials and immunosuppressive drugs were similar in both groups. There were also no statistically significant differences between both groups regarding the outcome of renal function: 33% of patients treated in the public health system retained normal renal function vs 30% of the private sector; 20% in both groups had persistent proteinuria and 10% of patients in the public sector vs 13% in the private had renal failure. Only 2 patients in the latter group underwent transplantation and one was on dialysis (vs 3 public sector patients requiring dialysis).
The 10-year survival rate was 78% in the public system vs 91% of those treated in the private sector. In assessing the same rate at 15 years of follow up, no significant differences were found (72 vs 90%, log-rank test. 0.65) (Fig. 1).
DiscussionThe literature has reported that patients in the public health system are affected by socio-economic problems that hinder periodic visits to follow up on their underlying disease, treatment adherence and access to medication. It is less favorable lifestyle, poor nutrition, transportation and education issues lead to a delay in attention, a greater risk of infection and decreased survival.5
Despite these difficulties, patients in the public health system included in this study visited at a younger age and earlier in their disease evolution than patients seen in private practice (coinciding with the data presented by Dubois and Tuffanelli).6
There are few studies comparing symptoms, signs and laboratory data of populations served in public and private health systems. There seems to be an increased frequency of serositis, renal failure and hematuria in the population served in the public system, while Raynaud's phenomenon was observed with higher prevalence in patients from private practices.7
We were able to determine that the group of patients treated in the public sector more often had fever, increased consumption of C4 and higher ESR than those treated in private practice. They presented to the first visit with higher SLE activity measured by SLEDAI (probably because they developed renal disease earlier), so a higher proportion of them received cyclophosphamide. In general, these patients demonstrated a more active disease and, therefore, more serious from the clinical and laboratory standpoint. Tuffanelli Dubois and found no signs or symptoms that differentiate both populations, they only found easy fatigue as the only symptom that prevailed in the private practice patients.6
There were no statistically significant differences with the rest of the medication received by our 2 populations studied (antimalarials, steroids, mycophenolate, azathioprine, etc.). Which indicates that addressed in our public health system (which provides medication) does not entail a risk of worse survival by not having access to medication. Mayor and Vila reported less use of antimalarials in the public health system (as this medication is not provided by the state and patients do not have access to it due to economic costs) and increased use of intravenous steroids. Medical coverage is an issue closely related to poverty, which has been associated with mortality in some studies.7,8
The group of patients in the public sector had more severe SLE and, while it had a higher mortality rate than patients seen in private practice, this data did not reach statistical significance.
Patients with myocardial infarction, acquired and community-acquired pneumonia and immunodeficiency syndrome tended to have a better prognosis if they were attended by physicians experienced in handling such patients.9–15 Ward noted that the mortality of hospitalized patients with SLE was lower in hospitals where doctors were experts in managing this condition. This association is higher among patients hospitalized due to an emergency related to SLE.16–18These findings support the hypothesis that specific experience improves disease prognosis. Therefore, it is interesting to note that, in this study, both populations were treated by the same team of medical specialists.
Reveille et al.19 have documented that black patients with private health insurance had higher survival rates than black patients without insurance who attended a public health service, showing that ethnicity did not play a role. Petri et al. could not sustain the association between blacks and morbidity in lupus. Moreover, this suggests that non-adherence to treatment and the type of health insurance were important factors in morbidity.20
Patients with higher socioeconomic and educational levels have the ability to choose their specialist and access to medication; this allows them to seek medical attention much earlier, allowing them be treated for SLE in a reversible state of the disease and prevent or quickly treat infectious complications.5,21 In turn, if the patients are treated from the outset by specialists who know the disease and the public health system provides decent care (such as access to early diagnosis, the rational use of drugs, etc.), the prognosis of these patients should not be different from those in the private sector.
One limitation of this study is the fact that it is retrospective; there were no ethnic differences between patients (due to which we were unable to compare the effects of race in relation to clinical manifestations, laboratory or survival) and patients with less than one year of follow up were excluded from analysis.
In summary, this study shows that patients treated in the public sector had a more severe and active disease that led them to consult earlier than those in the private sector. The fact that public sector patients have access to medication and were treated by medical experts in the disease helped in that there was no survival difference between the two groups.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this study did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients, and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflict of interest.
The authors wish to thank Elena Carrera and Liliana Contini, for statistical assistance (Biometrics Unit, Department of Mathematics, Faculty of Biochemistry and Biological Sciences, UNL).
Please cite this article as: Schmid MM, Roverano SG, Paira SO. Comparación de datos demográficos, presentación clínica, tratamiento y desenlace de pacientes con lupus eritematoso sistémico tratados en un centro público y otro privado de salud en Santa Fe, Argentina. Reumatol Clin. 2014;10:294–298.