To assess the influence of the implementation of a program for secondary prevention of osteoporotic fractures on prescribing bisphosphonates and persistent short-term treatment.
Patients and methodsPatients >50 years of age with fragility fracture attended in the emergency department were enrolled in an observational study. The program consisted of (1) training of primary care physicians, (2) baseline visit: questionnaire on osteoporosis, bone densitometry and patient education, (3) patient referral to primary care, except those with multiple fractures or requiring special study or therapy, who were referred to a specialist, and (4) follow-up by checking prescriptions in electronic records, and a telephone survey. The outcome variable was the percentage of patients who, on having been prescribed bisphosphonates, still adhered to the treatment at 3 months.
ResultsOf the 532 patients with inclusion criteria, 202 (39%) refused to participate. Those who refused to take part had a higher mean age (P<.01) and a higher frequency of hip fracture (P<.01) compared with patients who did participate. A total of 330 patients were included for intervention, with a mean age of 71 years, and 254(77%) were women. An antiresorptive was being used by 45 patients (13%) at baseline. After the baseline visit 223 patients (67%) were recommended a bisphosphonate. In the follow-up at 3 months 78% of patients who had been prescribed bisphosphonate were still receiving treatment.
ConclusionsWe present a multidisciplinary program for secondary prevention of fractures coordinated by rheumatology in which the number of patients who were receiving bisphosphonate at 3 months increased by four times compared to that at baseline visit.
Evaluar la influencia de la implantación de un programa para la prevención secundaria de fracturas osteoporóticas sobre la prescripción de bisfosfonatos y la persistencia del tratamiento a corto plazo.
Pacientes y métodosSe incluyeron pacientes con fractura por fragilidad >50 años atendidos en el servicio de urgencias durante un año. El programa consistió en: 1) plan de formación en osteoporosis de los médicos de primaria; 2) densitometría ósea; 3) cuestionario relativo a osteoporosis y educación del paciente por la enfermera; 4) derivación al médico de primaria o, en caso de múltiples fracturas o precisar terapia parenteral, a consulta hospitalaria; y 5) seguimiento y comprobación de inicio del tratamiento prescrito a través de los registros electrónicos y encuesta telefónica. La variable principal de desenlace fue el porcentaje de pacientes que, habiéndose prescrito un bisfosfonato, cumple el tratamiento a los 3 meses.
ResultadosDe 532 pacientes con criterios de inclusión, 202 (38%) no aceptaron participar. Comparados con los pacientes que participaron, los que rechazaron tenían una edad promedio mayor (p<0,01) y una mayor frecuencia de fractura de cadera (p<0,01). Así, se incluyeron 330 pacientes con una edad media de 71 años, el 77% mujeres. Cuarenta y cinco pacientes (13%) utilizaban bisfosfonato al inicio del estudio, mientras que tras la visita basal se prescribió a 223 pacientes (67%). En el seguimiento a los 3 meses, el 78% de los pacientes a los que se aconsejó bisfosfonato estaba tomando la medicación.
ConclusionesEl programa de prevención secundaria de fracturas coordinado por reumatología consigue que el número de pacientes que inicia bisfosfonato se multiplique por 4 en comparación con la visita basal.
Fractures and their complications will be a health problem of the first order in the coming years due to the aging population. In Spain it is estimated that osteoporosis (OP) affects 32% of women aged 50 years and above to 52% of those aged 70 years.1 In addition, between 53% and 92% of fractures in women older than 50 years are attributed to OP.2 Fragility fractures are more common in patients who have had previous fractures. Wrist fracture, for example, increases the risk of hip and3 vertebral fracture. It is estimated that one of 4 patients with vertebral fracture suffer a second vertebral fracture during the next 2 years and 26% will suffer a non-vertebral fracture in the year following. At the same time, a fractured femur is the leading cause of disability and mortality in the elderly.4 In terms of costs, one study estimated that hip fracture, within 5 years, involves a cost of $36,929 U.S. dollars for women and $39,479 for men.5 The consequences of hip fracture were comparable to those of acute myocardial infarction and stroke.6 These data justify the need for an effective program to prevent fragility fractures.
Although treatment of patients with an OP fracture is cost effective in order to prevent new fractures,7 less than 20% of patients who have suffered a fragility fracture receive antiresorptive bisphosphonate treatment.8–10
Thus, 60% of cases of vertebral fractures diagnosed in primary care receive no treatment to prevent new vertebral fractures.11 Moreover, a high rate of treatment with antiresorptive bisphosphonates abandonment was found in these patients.12 Therefore, programs are needed for the detection and study of fractured patients, establishing management guidelines.
Coordination between hospitals and primary care is very important in these cases because once the fracture is healed there is no clear reference on who should undertake the study and monitoring of the patients. Existing models for secondary prevention of fractures are mostly Anglo-Saxon13,14 and should be adapted to our healthcare environment. In this study we present the results of a strategy for secondary prevention of osteoporotic fracture, the first multidisciplinary study of its type in Spain.
Patients and MethodsThis is an observational study, conducted in the area of Gran Canaria north, with 2 distinct parts: (1) prospective intervention study and (2) retrospective study. The structure of the health area in 2012 was as follows: 332,650 inhabitants older than 14 years of age, 21 health centers and 255 primary care physicians.
Prospective StudyHealth Centers Training PlanThe study included the training on OP and fragility fracture of primary care physicians in the health area through a session lasting 60min given by rheumatologists. The key points of the meeting were (1) the need to treat patients at high risk for fracture and maintain treatment, (2) explanation of the study protocol and patient flow from the densitometry unit to primary care and (3) presentation of the model report issued by the fractures unit and the offer of communication channels to resolve questions (telephone, fax and email).
Selection of PatientsPatients were seen in the emergency department of the hospital between March 2012 and March 2013 with a diagnosis of fracture. The first step was obtaining a mail list, followed by a screening of patients and application of the inclusion criteria based on the data platform. This work was carried out by the coordinators (AN and SOB) and took about 3h every month. The new listing was given to a secretary trained for the study, who, by telephone, informed the patient about the convenience of assessment from the bone metabolism point of view.
If after telephone contact the patient met the inclusion criteria and agreed to participate in the study, an appointment was made for the baseline visit, which was scheduled at least 2 months after the fracture and patient recovery. At baseline, a densitometry (DXA) followed by a consultation with the nurse was performed. This task entailed a nurse workday each week.
The selection criteria of patients were adults over 50 years with fragility fracture at any site except facial bones and skull, ribs and bones of the hands and feet. Fragility fracture was defined as a fracture that occurs as a result of a fall from the height of the person or lower.
Patients with pathological fracture or severe functional disability, as well as patients with advanced liver disease or renal failure, or any serious medical illness criteria were excluded.
Study ProtocolThe study was approved by the ethics and research committee of the hospital and follows the Helsinki Declaration of 1975. All patients gave written consent.
The nurse recorded the following data for each patient: OP family history of fracture (broken hip in parents), personal history of fragility fracture, active smoking, alcohol consumption, rheumatoid arthritis, previous use of any medication for OP (including bisphosphonates) and use of corticosteroids. Other secondary causes of OP were also recorded, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated hypothyroidism, hypogonadism or premature menopause (<45 years), chronic malnutrition or malabsorption, and chronic liver disease. Also, the height and weight of each patient were recorded to calculate the body mass index.
Bone mineral density was measured with DXA Hologic QDR-4500 (Hologic, Waltham, MA, USA. UU) equipment. Normal bone, osteopenia and OP were defined according to WHO criteria.15 The FRAX® index was calculated using the tool available online for the Spanish population (http://www.shef.ac.uk/FRAX/tool.jsp).
Laboratory tests recommended for all patients included complete blood count, ESR, biochemical profile, serum calcium and phosphorus, alkaline phosphatase, serum 25 OH vitamin D, and thyroid and parathyroid hormone determinations. In patients with urolithiasis history, a determination of calciuria and phosphaturia was added. In males, we recommended including serum free testosterone levels in addition to LH and FSH.
Treatment and Follow-upPatients received specific education by a nurse trained in OP. Treatment was explained, including tips for exercise, improving calcium intake with diet, avoiding alcohol and tobacco use, and measures to prevent falls. Patients were informed about the benefits of drug treatment with bisphosphonates. The nurse emphasised particularly on how to take the tablets and the importance of maintaining the prescribed treatment.
Recommendations to indicate bisphosphonate treatments were based on the guidelines for treatment published by the NOF (web site for detailed information: http://www.nof.org/professionals/pdfs/NOF_ClinicianGuide2009_v7.pdf). The treatment protocol was agreed on between rheumatology and primary care. The first choice of treatment was alendronate or risedronate. The decision to treat was based on the type of fracture (indicated in all hip and vertebral fractures), the result of the DXA (indicated in all OP) and fracture risk estimated by FRAX® (the rest of patients were treated if the risk of hip fracture was >3%). Regardless of the use of bisphosphonate, calcium supplements (1000mg/d) and vitamin D (800IU/d) were advised for all patients.
Patients treated at baseline were referred to primary care with the results of the DXA and a treatment decision algorithm, whether or not they were given a bisphosphonate. This report was issued by the nurse and signed by a medical coordinator. More serious cases such as vertebral fractures, multiple fractures and those with digestive problems receiving oral treatments were referred to rheumatology (see metabolic diseases) in order to assess not only bisphosphonate use, but also other treatments for OP.
The main outcome variable was the percentage of patients with confirmed onset of bisphosphonate therapy at 3 months from baseline, both proven through electronic records (medical coordinator) and by telephone (nurse). Follow-up work was done by the nurse in the weekday devoted to fractures while the medical coordinator employed three monthly hours.
Retrospective StudyA sample of patients with the same inclusion criteria as that in the prospective phase, treated in the emergency department 6 months before the start of the study were analyzed. Prescription of antiresorptive treatment was documented in electronic health records 6 months after the fracture occurred. The retrospective group was included for routine clinical practice in the health area and bias in primary care training talks on treatments at baseline were eliminated in the intervention group.
Statistical AnalysisThe characteristics of patients who refused the study and of those finally included, as well as of patients who started bisphosphonate and of those not taking it 3 months from the baseline visit were compared. Possible differences between the groups were analyzed by Student's t test for continuous variables and chi-square test for categorical variables. SPSS version 15.0 for data analysis was used. Statistical significance was set at P<.05.
ResultsIn this paper we present the results of the first 12 months of the program.
In the retrospective study, 167 patients met the criteria for evaluation; 70% women, with an average age of 71 years, were reviewed. The percentage of distribution of fractures in this group was as follows: forearm 30%, femur 24%, humerus 15%, and other fractures 29% (P=.57 compared with the prospective intervention group). In reviewing the 6 months after fracture treatment, 23 patients (13.7%) were prescribed an antiresorptive.
In the prospective study, a total of 532 patients met the inclusion criteria and were invited to participate, of whom 202 (38%) did not accept. Compared with the patients who agreed to participate, those who refused had a higher mean age (73 vs 70 years, P<.01) and a higher frequency of hip fracture (27 vs 21%, P<.01).
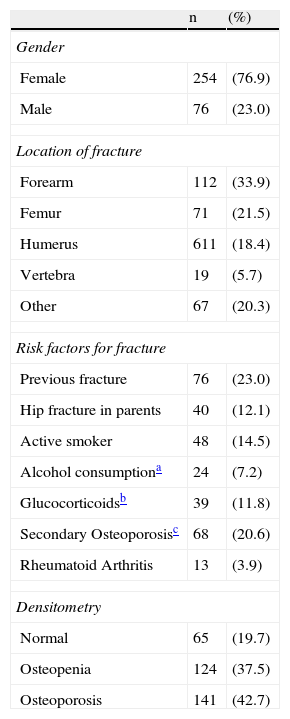
We included 330 patients for intervention, 254 of them women (77%). The mean age was 71 years, 64 patients were less than 60 years, 87 patients were between 60 and 69 years, 103 patients were between 70 and 79 years and 76 patients were over 79 years of age (Table 1). The most common fracture was that of the forearm (34%) followed by the femur (21%). A total of 68 patients (20%) were receiving calcium and/or vitamin D, and 45 patients (13%) were taking bisphosphonate or other effective drugs for reducing fractures at baseline (59 of them, 18% in the past). The DXA study showed osteopenia or OP in 80% of cases. The FRAX® for hip fracture was >3% in 153 patients (46%). After baseline, 213 patients were referred to the primary care physician (64%) and 117 patients to the hospital clinic (35%). In total, bisphosphonate treatment was recommended to 223 patients (67%): 109 of those sent to primary care (51%) and 114 of those sent to the hospital clinic (97%). The remaining 107 patients, presenting a low risk of fracture, received only general advice and supplements of calcium and vitamin D.
Characteristics of the Patients Included in the Intervention Study (n=330).
| n | (%) | |
| Gender | ||
| Female | 254 | (76.9) |
| Male | 76 | (23.0) |
| Location of fracture | ||
| Forearm | 112 | (33.9) |
| Femur | 71 | (21.5) |
| Humerus | 611 | (18.4) |
| Vertebra | 19 | (5.7) |
| Other | 67 | (20.3) |
| Risk factors for fracture | ||
| Previous fracture | 76 | (23.0) |
| Hip fracture in parents | 40 | (12.1) |
| Active smoker | 48 | (14.5) |
| Alcohol consumptiona | 24 | (7.2) |
| Glucocorticoidsb | 39 | (11.8) |
| Secondary Osteoporosisc | 68 | (20.6) |
| Rheumatoid Arthritis | 13 | (3.9) |
| Densitometry | ||
| Normal | 65 | (19.7) |
| Osteopenia | 124 | (37.5) |
| Osteoporosis | 141 | (42.7) |
| Mean | (SD) | |
| Age (years) | 71.1 | (10) |
| FRAX | ||
| Main fracture | 13.1 | (12) |
| Hip fracture | 7.0 | (12) |
At follow-up at 3 months, from the data from 169 patients who were prescribed bisphosphonate treatment, 133 (78%) were undergoing the prescribed treatment. Twelve of the 133 patients started treatment after forwarding the DXA report to the PCP or after a new appointment in the hospital clinic. Extrapolating data to the entire sample of 223 patients receiving bisphosphonate (multiplied by 5 compared to baseline), 174 patients had started treatment 3 months after the visit (multiplied by 4 with respect to the baseline visit). Comparing the group of patients who started treatment at 3 months with those who did not, patients who started it were on average older (74 vs 70 years, P=.007). However, there were no significant differences in relation to gender, type of fracture, fracture risk measured by FRAX® or the type of physician to whom the patient (primary care or hospital rheumatology) was submitted.
DiscussionAlthough there are moderately effective prophylactic treatments, most patients with fragility fracture are not studied or treated.8,10 In the present study, both in the retrospective group as at baseline and in the intervention group, fewer than 15% of patients were taking a bisphosphonate after fracture. We know it is more effective to treat with alendronate those patients with previous fracture since the number of patients needed to treat to prevent an OP vertebral fracture was 50 when no previous fracture was present (primary prevention), while it was an estimated 16 patients if a fragility fracture history was present.16
Different secondary prevention of fracture strategies published can be summarized as follows13:
- (a)
On the patient: information by telephone and/or letter, education and summons to visit with or without performing DXA or, in case of hospitalization, a report with treatment recommendations.
- (b)
On primary care physicians: report with treatment recommendations including DXA results if available. Performing DXA alone increases the prescription of treatment to prevent new fractures.17
- (c)
Specific units fracture: it has been observed that units that include specific personnel, especially nurses supervised by physicians experienced in OP and fractures, are the most effective in secondary prevention.17 The model of coordinated care systems of attention to fractures is officially recommended by the American Society for Bone and Mineral Research.18
Furthermore, because adherence to treatment for OP is low, estimated at 40%–50% in the first year,12,19 patients who have suffered a fracture should be followed up in order to increase adherence to treatment. It has been found that when the patient takes more than 80% of the prescribed medication, future fractures reduce significantly.20
In a study conducted in Spain by orthopedic surgeons, an increase in the diagnosis and treatment of OP after discharge due to a fracture was observed.21 The authors analyzed the usefulness of specific software in 70 hospitals,21 attaining 61% correct treatments for OP in the discharge report. Although this is a simple model that requires little infrastructure and no additional staff, it has the disadvantage of not including DXA or confirmation by the prescribing physician or primary monitor.
In a previous study by our group on fragility fractures, all patients were referred to the outpatient clinic for clinical evaluation, undergoing a DXA and treatment, with clinical follow-up for 12 months. After 4 years, the persistence of bisphosphonate therapy was 71%,9 which for this model is appropriate, yet it does not seem very effective because all patients must be assessed in hospital clinics with the consequential reviews.
We believe that the model presented here, regarding the care of fragility fractures, is a reasonable approach, adapted to the characteristics of the Spanish health system, integrating primary care physicians and other related OP specialists such as rheumatologists. This strategy covers performing a DXA, evaluation and patient education by the nurse and tracks treatment control, all known factors associated with an increase in fracture treatments. The time taken to carry it out is one day a week for the nurse and one day a month for the medical coordinator.
Results from the first year of our program are similar to those of other published models.9,17 The percentage of patients who were prescribed bisphosphonate increased from 13% at baseline to 67% after the evaluation. In the study by Harrington and Lease held in Madison (USA), after 3 years of experience with a coordinated unit fractures nurse and rheumatologist, they evaluated and advised treatment to 61% of patients with22 fractures. However, the most successful model is that done in Glasgow, which achieves 80% of patients participating in the program, 74% received treatment, with 96% of treatments prescribed by the GP and with patient compliance at one year of 86%.23 Thus, the Glasgow model appears to be cost effective, so it was taken as a reference for other centers in the UK.23
Our experience with these patients is that some of them are reluctant to participate in the study or take medication, assuming that only trauma was involved and they do not require more visits once the fracture is consolidated. It is therefore important that all health services involved in the patient's fracture remember the need for bone metabolic evaluation, starting with emergency medical and trauma care, to the primary care physician and musculoskeletal related specialists, endocrinology and other medical specialties. The main weakness we found in our study is not so much related to the model per se as the insufficient awareness of other medical specialties, such as primary care and trauma, on the importance of secondary prevention of fractures. When we reviewed the treatments at 3 months of the baseline visit, about a quarter of patients who were indicated or prescribed a bisphosphonate was not taking it; reasons such as fear of adverse effects or becoming a polymedicated patient were common. Therefore, we will try to strengthen the relationship with other specialties through training campaigns.
Rheumatology plays an important role in the secondary prevention of fractures because a good number of DXA units are managed by rheumatologists. In this regard, we believe that active uptake of fractured patients should be a priority of DXA units.
Our results show that, in the short-term, the strategy works as it involves the use of a small staff. If confirmed in the long term, this will allow the implementation of the model as a consolidated portfolio of services in the area of health care offerings.
In summary, we present the first multi-disciplinary and multi-professional program for secondary prevention of fractures in Spain, coordinated by rheumatologists. The number of patients who were prescribed and initiated bisphosphonate is multiplied 4 times compared with standard treatment.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that the study procedures conformed to the ethical standards of the responsible committee on human experimentation and are in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of data from patients and that all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
FinancingThis study is funded as a national research project by the Ministry of Science and Innovation, Carlos III Health Institute (reference PI11/01429).
Conflict of InterestThe authors have no conflicts of interest.
To Carmen Alonso and Fabiola Santana of the densitometry unit of the University Hospital of Gran Canaria Dr. Negrin. To Manuel de la Torre (Service of Traumatology and Orthopedic Surgery), Sinforiano Rodríguez (Geriatric Evaluation Unit), and Vanessa Diaz (Family Physician).
Please cite this article as: Naranjo A, Ojeda-Bruno S, Bilbao Cantarero A, Quevedo Abeledo JC, Henríquez-Hernández LA, Rodríguez-Lozano C. Resultados de un modelo de prevención secundaria de fractura osteoporótica coordinado por reumatología centrado en la enfermera y el médico de atención primaria. Reumatol Clin. 2014;10:299–303.