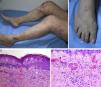
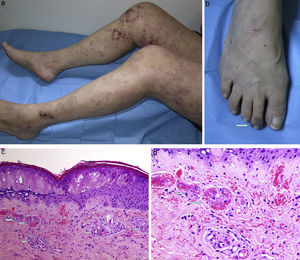
The patient was a 54-year-old woman who had no significant previous medical history. She presented with pruriginous lesions that had started on her legs 1 year earlier and had spread to her thighs, buttocks and upper limbs. They were accompanied by slight fever and arthralgia. Physical examination revealed an irregular and diffuse violaceous reticulated discoloration that in certain regions had become purpuric. They were very suggestive of livedo reticularis or livedo racemosa (Fig. 1a). She also had distal purpura on the second toe of her right foot (Fig. 1b). The differential diagnosis included cryoglobulinemia, polyarteritis nodosa, livedoid vasculopathy, cholesterol crystal embolism concomitant with arteriosclerosis, polycythemia vera, essential thrombocytopenia, atrial myxoma, etc. Skin biopsy revealed hyaline thrombi in the papillary dermal vessels, with no inflammatory infiltrate in the vascular wall (Fig. 1c, d). An antibody positive for lupus anticoagulant was detected, and was confirmed 12 weeks later. She was treated with acetylsalicylic acid, chloroquine and prednisone, which led to the disappearance of the systemic clinical manifestations, complete resolution of the distal purpura and attenuation of the livedo racemosa, which became less evident.
(a) Livedo reticularis in its variant, livedo racemose, involving both lower limbs in their entirety. (b) Purpuric discoloration on the second toe. (c) Skin displayed epidermal necrosis and the presence of hyaline thrombi in the papillary dermal vessels (hematoxylin–eosin, 100×). (d) Greater detail of the thrombi (hematoxylin–eosin, 20×).
Antiphospholipid syndrome (APS) is a prothrombotic state characterized by the presence of antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant or anti-β2-glycoprotein I). The diagnosis also requires evidence of arterial, venous or microcirculation thrombosis or a history of recurrent fetal loss.1–3 It is also frequently accompanied by cutaneous manifestations (which occur in up to 40%–50% of the patients). Livedo reticularis is the disorder most widely reported and, on occasion, they may be the first sign of the disease.4,5 Other possible lesions are skin ulcers, purpuric lesions, skin necrosis, superficial thrombophlebitis and atrophie blanche-type lesions.6–8 Our familiarity with these manifestations would enable us to make a diagnosis as early as possible and prevent potential complications of the disease.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Campos-Muñoz L, Fueyo-Casado A, Cortés-Toro JA, López-Bran E. Manifestaciones cutáneas del síndrome antifosfolípido. Reumatol Clin. 2017;13:233–234.