In recent years, the use of vertebral cementing techniques for vertebroplasty and kyphoplasty has spread for the treatment of pain associated with osteoporotic vertebral compression fractures. This is also associated with the increased incidence of complications related with these procedures, the most frequent being originated by leakage of cementation material. Cement can escape into the vertebral venous system and reach the pulmonary circulation through the azygous system and cava vein, producing a cement embolism. This is a frequent complication, occurring in up to 26% of patients undergoing vertebroplasty but, since most of the patients have no clinical or hemodynamical repercussion, this event usually goes unnoticed. However, some serious, and even fatal cases, have been reported. We report the case of a 74-year-old male patient who underwent vertebroplasty for persistent pain associated with osteoporotic L3 vertebral fracture and who developed a cement leak into the cava vein and right pulmonary artery during the procedure. Although he developed a pulmonary cement embolism, the patient remained asymptomatic and did not present complications during follow-up.
En los últimos años se ha extendido el uso de técnicas de cementación vertebral, vertebroplastia y cifoplastia, para el tratamiento del dolor asociado a fracturas vertebrales osteoporóticas. Se han descrito diferentes complicaciones relacionadas con dichos procedimientos, siendo las más frecuentes derivadas de la fuga del material de cementación. El cemento puede extravasarse al sistema venoso vertebral y a través del sistema ácigos y la vena cava alcanzar la circulación pulmonar, produciendo embolismo por cemento. Esta complicación es frecuente, ocurriendo hasta en 26% de los pacientes sometidos a vertebroplastia, pero dado que generalmente no produce repercusión hemodinámica ni clínica este evento suele pasar inadvertido. Sin embargo, se han descrito algunos casos graves e incluso fatales. Presentamos un paciente varón de 74 años, sometido a vertebroplastia por dolor persistente asociado a una fractura vertebral osteoporótica en L3, que presentó una fuga de cemento hacia la vena cava y la arteria pulmonar derecha. Aunque desarrolló un embolismo pulmonar por cemento, el paciente permaneció asintomático y sin complicaciones durante el seguimiento.
Vertebroplasty and kyphoplasty are percutaneous techniques which employ vertebral cement and their use have spread widely in recent years in the treatment of pain associated with vertebral fractures, especially those of osteoporotic origin. These procedures, in addition to relieving pain, stabilize and prevent further collapse or vertebral height loss or kyphosis deformity progression.1 In the case of vertebroplasty, cement (typically polymethyl methacrylate or calcium phosphate) is injected through a needle into the spongy bone of the vertebral body through the pedicles. The cement flows through the path of least resistance and the procedure is monitored by fluoroscopy.2 For both procedures, a cannula is placed in the vertebral body through which 2 ballons are inserted, which upon inflation compact the surrounding cancellous bone and create a closed cavity. These ballons are then removed and the cavity is filled with cement. As with vertebroplasty, the entire procedure is monitored fluoroscopically.3
While there is widespread practice of these techniques because of their potential effectiveness, one should also take into account the complications arising from them, some very complex, as a refracture of a previously stabilized vertebra, vertebral fractures or persistent pain. However, the most frequent complications for both procedures are those derived from the leakage of cementing material, especially in the case of vertebroplasty and may range from small asymptomatic extravasation into surrounding tissue to embolism to the pulmonary circulation.4 We present the case of a patient who developed cement pulmonary embolism (CPE) after vertebroplasty performed for the treatment of pain associated with an osteoporotic vertebral fracture.
Case PresentationA 74-year-old male patient developed mechanical dorsolumbalgia, with no irradiation, with a sudden onset after moderate effort in March 2007, which led to the diagnosis of multiple vertebral collapse. The patient had a history of being a former smoker (10cigarettes/day for more than 20 years) and having been diagnosed in the previous year with a colon adenocarcinoma, requiring colectomy plus a permanent colostomy and receiving oral chemotherapy. He maintained an adequate dairy intake and sun exposure, with an active life and had no history of urolithiasis, prior fragility fractures, thyroid disease or steroid use.
The radiological study revealed the presence of a previous vertebral compression at the D7, D9, and L3 levels, without displacement of the rear wall, and the MRI also showed the presence of bone edema in L3, corresponding to the most painful area. He was treated with Level II analgesia (tramadol plus acetaminophen and NSAIDs), without any improvement in pain, presenting disabling and limited mobility, so it was decided that he should undergo a vertebroplasty at L3.
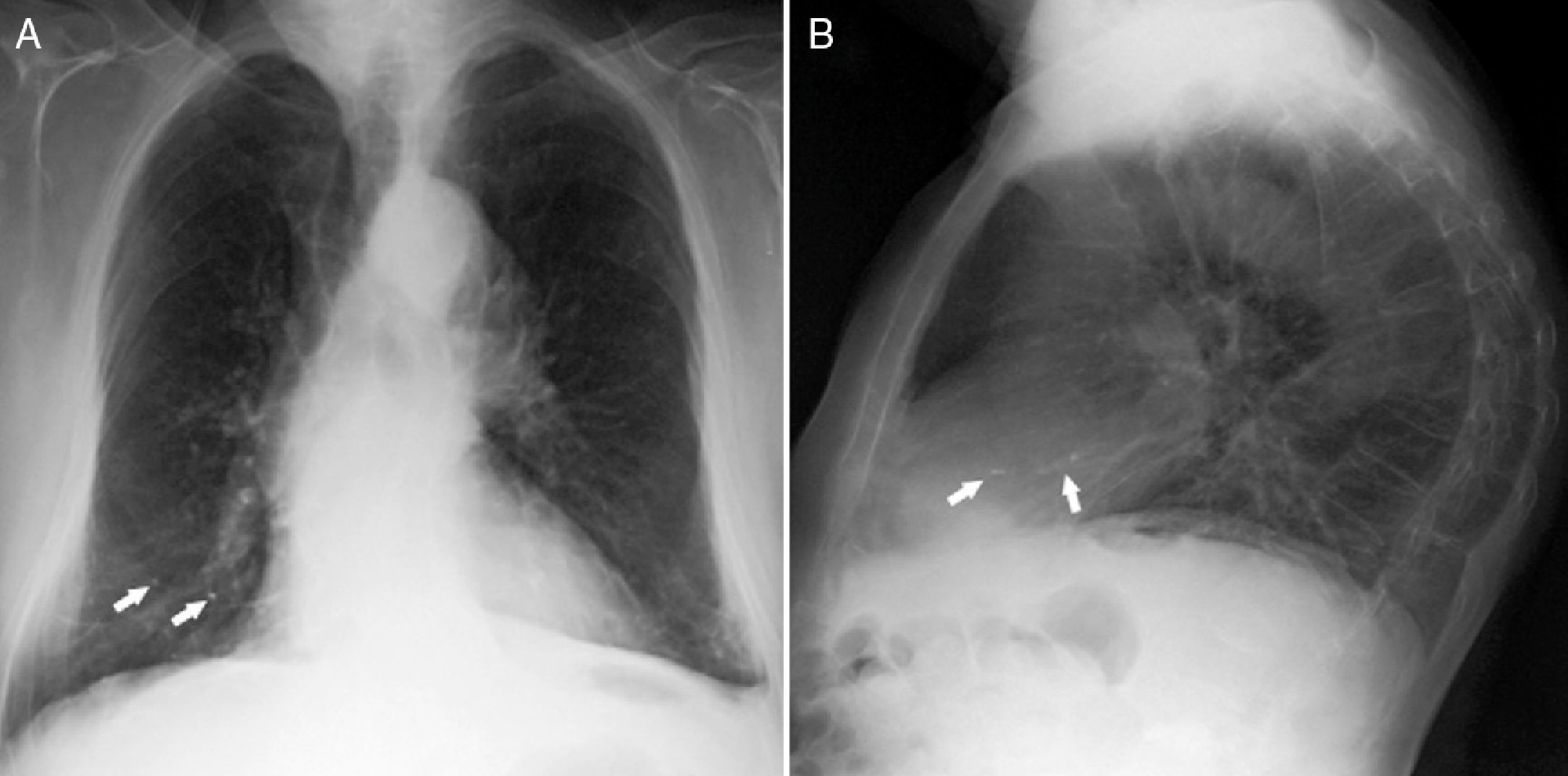
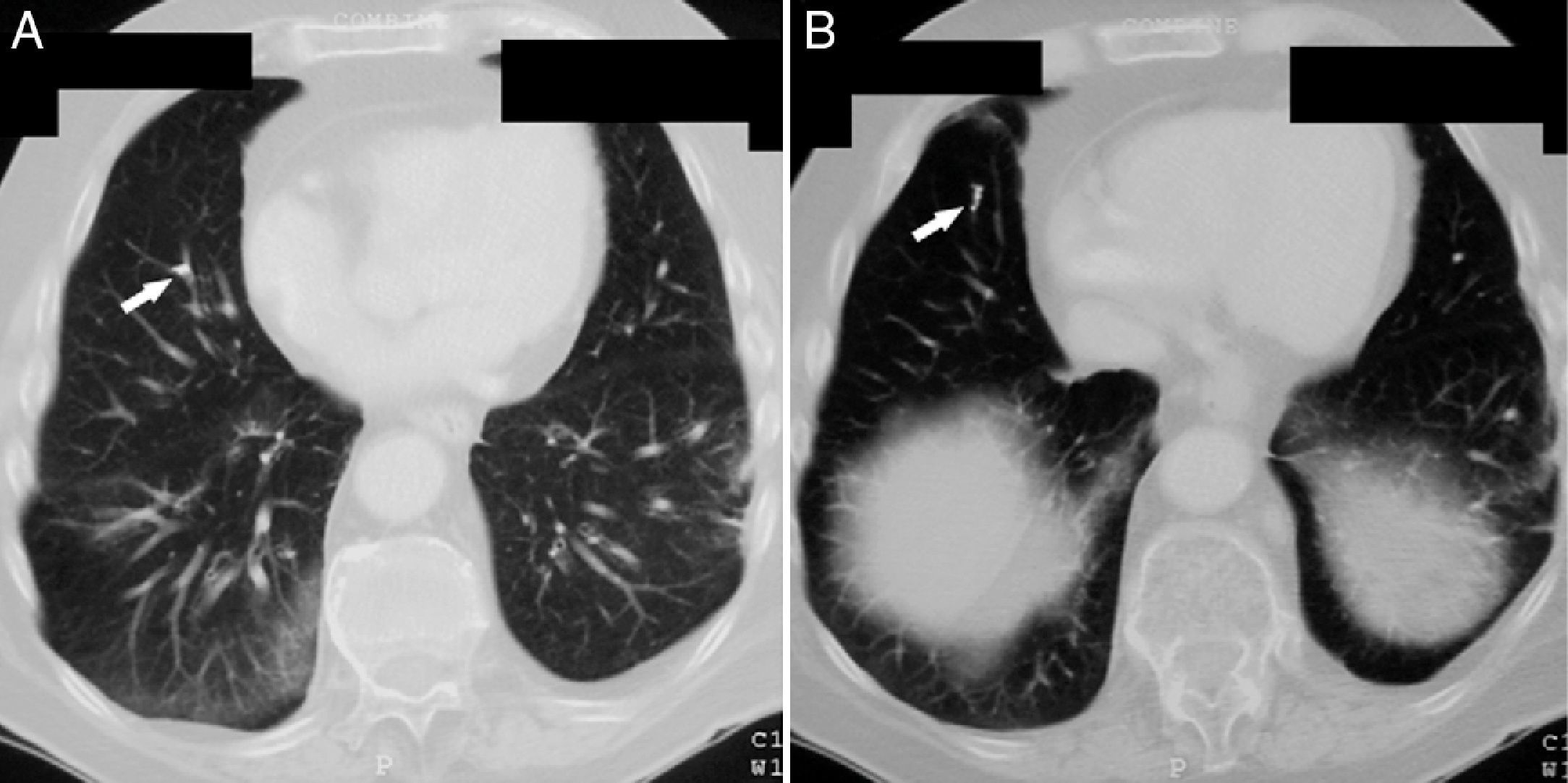
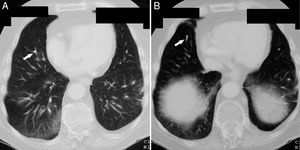
Vertebroplasty was performed in July 2007 and during the procedure surgeons detected a small cement leakage into the vena cava and the right pulmonary artery. The patient remained asymptomatic after vertebroplasty, without developing signs of hypoxemia and pulmonary hypertension. However, the control chest X-ray after the procedure showed radiopaque lesions on the vessels of the lower third of the right lung, which on CT corresponded to multiple emboli of cement in the distal branches of the right pulmonary artery in the middle and lower lobes (Figs. 1 and 2). The patient had no pain after the procedure and was asymptomatic from the respiratory standpoint; however, the cement emboli remained unchanged and are still observed in radiological controls to date.
Vertebral cement material leaks occur more frequently during vertebroplasty (30% to 75%) than with kyphoplasty (from 8% to 33%).5 These leaks can cause local and systemic complications, including the CPE in the latter group. CPE is a relatively common event after vertebroplasty, with an incidence of 0%–23% in observational studies, while in the multicenter, randomized clinical trial Vertos II (which compared the efficacy and safety of vertebroplasty compared to conservative treatment in patients with osteoporotic vertebral compression fractures) it was found to occur in up to 26% of patients.6 Patients undergoing kyphoplasty develop CPE much less frequently, with a few cases reported and some series showing an incidence of 0.2%–4.6%.7,8 It is considered that the difference in the CPE incidence between the 2 procedures is due to biomechanical factors because, unlike vertebroplasty in which cement is injected at high pressure into the vertebral body, the balloon kyphoplasty creates a low pressure cavity that will expand and compress the cancellous bone, thereby sealing bone or venous defects that could allow leakage of cement.8
The migration of cement to the pulmonary circulation occurs its extravasation toward the vertebral venous plexus, which is connected to the azygos system, reaching in this way the vena cava and the pulmonary arterial system.9 Actually, the only risk factor identified to date for the development of CPE is fluoroscopic evidence of leakage of cement to the azygos vein or vena cava during the procedure.6,10 Therefore, patients in whom these leaks are observed, should also be evaluated to rule out a pulmonary circulation CPE. Conversely, the apparent absence of leakage of cement under fluoroscopy does not exclude the migration thereof into the pulmonary circulation, since most are small and no leaks are detected during the procedure.11
In most patients CPE is not a clinical event. In the Vertos II study all patients were asymptomatic at the time of diagnosis, which was made by imaging findings. This is because the cement emboli are usually small and are distributed sparsely in peripheral areas of the lung, with no specific lobar localization. Moreover, cement is usually deposited in the heart or great vessels.6 Tracking studies conducted in patients with CPE show that cement deposits are not associated with the occurrence of structural changes in the lung parenchyma and patients usually do not develop sequelae.6,12 This is considered because the cement behaves like a biologically inert agent without causing inflammation in the lung parenchyma.6
Despite the apparent safety of vertebroplasty, severe cases of CPE have been described, including some fatalities.13–18 These cases are usually associated with large volumes of injected cement (9–15ml) or the production of massive cement leakage into the heart or central pulmonary arteries. Clinically, we can suspect a CPE after vertebroplasty sudden with the appearance of symptoms such as dyspnea/tachypnea, tachycardia, cyanosis, chest pain, cough, hemoptysis, and sweating.4 Persistent pulmonary hypertension after CPE has been infrequently described.19 There are no management guidelines for CPE. In asymptomatic patients no treatment is recommended and in those with symptomatic or central embolism it is recommended to follow standard treatment guidelines for pulmonary thromboembolism, including measures such as initial heparinization and coumarin therapy for 6 months.4
Because vertebral cementing techniques are performed with increasing frequency, some strategies should exist to prevent the development of CPE. Some studies have considered the amount of cement injected into the vertebral body, the position of the needle, the unilateral type of approach vs a bilateral one and the degree of prolimerization of cement at the time of injection. It is recommended that the volume of cement injected is limited to 4–6ml per vertebral body, with special care when performing the procedure in several vertebrae.20 Regarding the position of the needle, a venography of the vertebral body is recommended before injecting the cement, since this way fast flow connections may be detected between the spinal epidural compartment and the vena cava, allowing to redirect the tip of the needle and prevent its passage into the pulmonary circulation.9 It is considered that the bilateral approach is safer than the unilateral for locating the tip of each needle into the lateral area of the vertebral body, thus preventing the central part where leakage into the vein is more frequently found.11 Finally it is recommended that the cementing material have a highly viscous consistency, similar to toothpaste as highly liquid material or excess pressure can cause leakage.20
Because CPE after vertebroplasty is not a rare event and since most cases are initially asymptomatic, the routine performance of a chest X-ray is recommended after the procedure, and even the performance of CT scans for early detection of cement emboli in the pulmonary circulation. In X-rays such emboli may be seen as multiple tubular or branched radiopacities. Computed tomography is the test of choice to confirm their presence, distinguished from other calcified lesions due to their location in areas of branching and the accompanying high attenuation areas around the pulmonary arteries. Echocardiography may be useful in assessing the development of pulmonary hypertension in patients with symptomatic or multiple emboli. In these patients, respiratory function tests may also show decreased CO2 lung diffusion capacity.20
In conclusion, CPE commonly occurs after performing vertebroplasty, but is uncommon or hemodynamically has little clinical impact. However, patients undergoing this procedure should be carefully evaluated from the respiratory and cardiovascular standpoint after its implementation, especially those with indicative symptoms. It is desirable to perform imaging in the way of X-rays in all cases and CT scans, especially those in which cement leakage is detected during the procedure.
Ethical ResponsibilitiesProtection of People and AnimalsThe authors state that no experiments were performed on humans or animals.
Data ConfidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to Privacy and Informed ConsentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflicts of InterestThe authors have no disclosures to make.
Please cite this article as: Sifuentes Giraldo WA, et al. Embolismo pulmonar por cemento tras vertebroplastia. Reumatol Clin. 2013;9:239–42.