Prevalence studies may underestimate the frequency of some chronic diseases such as gout, as they are asymptomatic for long periods of time; several articles have reported that osteoarthritis (OA) and rheumatoid arthritis (RA) are the most prevalent rheumatic diseases.1–3 In an epidemiological study in our country, in which the COPCORD methodology was used, a prevalence of 10.5% and 1.6% for OA and RA was reported, respectively, whereas the prevalence of gout in this report was 0.3%.4 Reports of incidence in other countries suggest that gout is the most common inflammatory joint disease, in contrast to some studies that indicate other methodology.5,6 In our country, there is no epidemiological data on the incidence of various rheumatic diseases, but we have the perception that some of them are more common than others.
With this in mind, we interviewed 111 doctors, asking them the number of persons among their “known”-first-or second-degree family members, political family and friends, who had the diagnosis of OA, fibromyalgia (FM), RA, lupus erythematosus (SLE), ankylosing spondylitis (AS) or gout. Statistical analysis was performed using descriptive statistics.
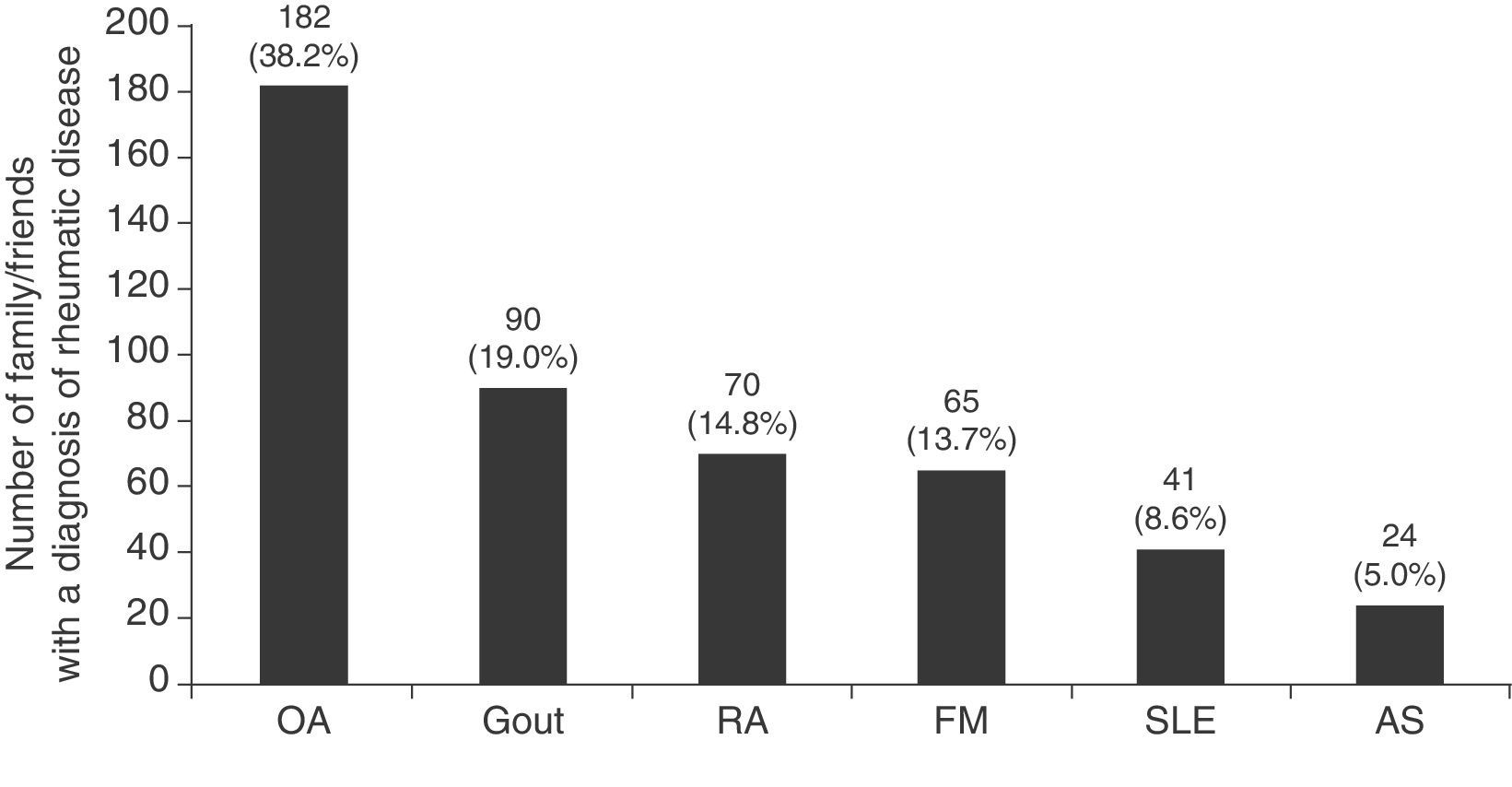
The physicians who responded to the survey were 57 men/54 women, 45 (40.5%) medical residents, mainly of internal medicine (17), rheumatology (5) and gastroenterology (4); 37 (33.3%) were medical specialists, of which 29.7% saw musculoskeletal diseases, 70.3% are internists or related subspecialists (9 internists, 2 endocrinologists and 2 geriatricians); finally, 24 (21.6%) were general practitioners and 5 (4.5%) family physicians, with a mean age±standard deviation 30.9±6.7 years. As perceived by the respondents, 85.5% had at least one family member/friend with one of the diseases mentioned. Each respondent had, on average, 4.3±7.2 (median 2) family/friends with one of the diagnoses. As expected, OA was the most common rheumatic disease followed by gout, RA, FM, SLE and AS (Fig. 1).
The respondents knew 1.3 times more patients with gout among family and friends than someone diagnosed with RA; in addition, we found that there were 1.38, 1.7 and 3.75 times more patients with gout than those observed with FM, SLE and AS, respectively.
The reported differences in the frequency of gout are related to the methodology, the type of study and the approach to diagnosis. It is also possible that these differences are related to the characteristics of the disease, since, unlike the OA and RA, gout has episodic clinical manifestations and may remain asymptomatic for long periods of time. In the various studies, the diagnosis is established variably, either by patient self-report, clinical databases and drug use, evaluation by a family doctor, internist or rheumatologist. Sometimes the diagnosis can be challenging for primary care physicians; the preliminary criteria of the American College of Rheumatology7 have been evaluated in several studies and have shown great limitations.8,9
There are at least 5 proposals for the clinical diagnosis of gout, including 2 very recent,10,11 but both have some controversial points12 and these are taken as the basis for a multicenter, multinational study being done in order to propose clinical criteria for the classification of gout that may be used by different studies and primary care physicians.13 Surely, improved detection of this disease will be crucial in the reports of its frequency.
Please cite this article as: García-Méndez S, Arreguín-Reyes R, López-López O, Vázquez-Mellado J. Frecuencia de la gota según la percepción de los médicos en México. Reumatol Clin. 2014;10:197–198.