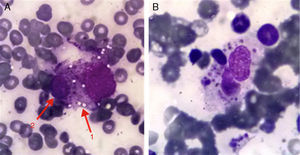
The patient was an 83-year-old man who was admitted to our department with hyperglycemia, but his reason for coming was that he felt generally unwell. He had type 2 diabetes and alcoholic cirrhosis with grade 2 esophageal varices, with no episodes of ascites-related decompensation, and had been diagnosed with polymyalgia rheumatica 6 months earlier; he reported having had symptoms consistent with upper respiratory infection the week before admission. Chest X-ray revealed an increase in the alveolar interstitial region, with no clear evidence of infiltrates. The most notable laboratory finding was pancytopenia, with a platelet count of 27000l. Tomography disclosed the presence of bilateral pleural effusion with posterior infiltrates and, in abdomen, an image consistent with hemoperitoneum, with spontaneous rupture of the spleen. On the basis of these findings, anemia was suspected. Analyses revealed a hemoglobin level of 8.5mg/dL, ferritin level of 1102ng/mL, erythrocyte sedimentation rate of 75mm/first hour and hypertriglyceridemia (270mg/dL). Bone marrow aspiration was performed and the bone marrow smear was studied using Wright's stain. Fig. 1 shows a histiocyte with vacuolated cytoplasm (arrow 1), phagocytosing a hematopoietic cell (arrow 2–lymphocyte). A histiocyte can also be seen phagocytosing a number of hematopoietic cells, with cellular debris in its cytoplasm. The findings obtained pointed to a diagnosis of haemophagocytic syndrome1,2 and treatment with intravenous gammaglobulins was begun. The patient's clinical response was good, with an improved platelet count at the end of the treatment (85000l).
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
We thank Dr. Pilar Brito-Zerón, of the Department of Autoimmune Diseases of the Hospital Clínic, without whose help, this case would not have had such a good ending.
Please cite this article as: Hurtado García R, Beneit Villena P, Martín Guillén S, Pérez Bernabéu A. Síndrome hemofagocítico en paciente con polimialgia reumática. Reumatol Clin. 2016;12:50–51.