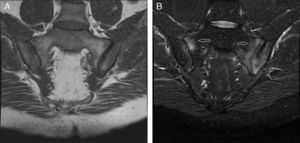
The patient in question is a 44 year old male with a history of alcohol abuse. He came to the consultation due to episodes of mono/oligoarthritis of the hands and ankles, recurring every week for 5 years, and inflammatory back pain of 10 years of evolution, with alternating buttock pain. He reported no other accompanying symptoms. Examination revealed the presence of arthritis of the right wrist, left 4th and 5th PIP with accompanying nodules. Laboratory tests showed uric acid 13.2mg/dl, ESR 44mm/h (0–20) CRP 15mg/l (<5mg/l) and a Mantoux test of 20mm. The remaining tests (CBC, TSH, CPK, rheumatoid factor, HLA-B27, anti-citrullinated-peptide antibodies, immunoglobulins, antibodies for hepatotropic virus, HIV, syphillis, Brucella, renal function, liver, urine sediment and uricosuria 24h) were normal. Chest, hands and feet X rays showed no pathological findings. The lumbar spine radiograph (Fig. 1) demonstrated left sacroiliitis stage II and right sacroillitis stage III. Examination with magnetic resonance imaging (MRI) of the lumbar spine was normal and sacroiliac MRI (Fig. 2) demonstrated irregularities and erosions in both sacroiliac joints observed in the T1 sequence. STIR detected subchondral bone marrow edema, markedly in the ilium and left sacral bone, with the right sacroiliac joint being less involved.
Semicoronal T1 and STIR sequence MRI cuts of the sacroiliac joint. (A) T1 sequence shows clear irregularities and subchondral bone erosions in both sacroiliac joints, as well as sacroiliac focal sclerosis in the left joint. (B) STIR sequence with a hyperintense signal corresponding to subchondral bone marrow edema (arrows), more severe on the left ilium and sacrum, and with less involvement in the anterior segment of the right sacroiliac joint, compatible with active sacroiliitis.
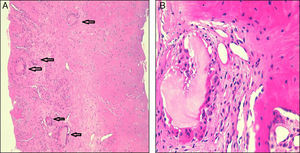
Arthrocentesis of synovial fluid (SF) of the 5th PIP joint of left hand nodule was performed, finding monosodium urate crystals (MSU) under polarized light microscopy with a negative culture. The patient was diagnosed with chronic tophaceous gouty arthritis. Dietary measures and medical treatment was initiated with allopurinol (300mg/d) and colchicine 1mg day. On the other hand, due to the coexistence in this patient of inflammatory back pain, along with radiographic bilateral sacroiliitis, the presence of active sacroiliitis on MRI according to the ASAS criteria1 and a normal lumbar spine MRI, we decided to perform the differential diagnosis with other diseases such as spondyloarthritis (the patient had no family history of psoriasis or inflammatory bowel disease) and infections. To do this, a sacroiliac joint biopsy where intraosseous tophi were demonstrated (Fig. 3A and B) was performed and MSU crystals proven to exist. Currently, the patient is asymptomatic, with a reduction of tophi and uric acid levels 5.6mg/dl, after 5 months of treatment.
DiscussionGout is a chronic disease caused by deposition of MSU crystals in joint, peri-articular, subcutaneous and, although infrequently, bursae and tendon tissue. Its prevalence in Western countries is estimated at about 1%–2%.2
Until recently it was thought that spinal gout was a rare entity, however some studies show that it has a prevalence of up to 35% of patients with gout when an active case is studied with sophisticated imaging techniques.3–5 This type of involvement is rare in patients under 45, as occurred in the case presented.6 The lumbar spine is the most frequently affected area,3–6 with the sacroiliac joint less often affected, 7.5%–17%.7,8 The literature has several publications on axial involvement in gout and, as predisposing factors, longstanding gout, degenerative disk disease and renal transplantation have been proposed.3–13
Therefore, a patient with sacroiliitis should always undergo a thorough differential diagnosis. The most common causes of unilateral sacroiliitis are infectious, traumatic or metastatic disease. Among the disease with asymmetric bilateral involvement, we must suspect psoriatic arthritis, osteoarthritis, or spondylitis associated with inflammatory bowel disease. As for diseases with symmetrical bilateral involvement, the most common cause is ankylosing spondylitis (AS). Therefore, in this patient a differential diagnosis of sacroiliitis was gout, because of patient history, and AS. Both diseases manifest with inflammatory back pain, although in gout the onset is usually sharper and in AS it is more insidious. In both cases, laboratory tests show elevated acute phase reactants, and HLA-B27 may be negative in up to 10% of10 AS cases. Radiological findings regarding juxta-articular erosions find irregularities at the sacroiliac level, both in gout and AS. MRI in axial gout is unspecific.3,13–15 All this leads to the diagnosis, though in some cases a joint biopsy is required, as in the case presented.
The therapeutic management of sacroiliitis in gout is the same as that used for other locations.14
In conclusion, sacroiliitis due to gout, although rare, should be included in the differential diagnosis of patients with inflammatory back pain, especially in patients with risk factors for MSU crystal deposition disease.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no conflict of interest to state.
Please cite this article as: Escudero R, Almodóvar R, Zarco P, Bueno Á, Dhimes P, Mazzucchelli R, et al. Lumbalgia inflamatoria en varón de 44 años. Reumatol Clin. 2015;11:325–327.