To evaluate the larynx involvement in patients with rheumatoid arthritis (RA) in a clinical setting and correlate with the different clinical features related to more aggressive disease.
MethodsCross-sectional study including 36 consecutive patients with RA. Reflux symptoms were evaluated by the Reflux Symptom Index (RSI) and vocal cord impairment by the Voice Handicap Index-10 (VHI-10). Laryngeal involvement was done by videolaryngostroboscopy (VLS).
ResultsThe mean age was 56.3±14 years with a mean disease duration of 2.6±3.1 years (range 0–16 years). Voice use was considered as professional users in 33%. Twenty-four (67%) out of 36 patients had abnormal findings of VLS. One patient had larynx nodules (bamboo nodules). Eleven patients (31%) were diagnosed with muscle tension dysphonia, and there were symptoms and signs of pharyngeal-laryngeal reflux in 23 (64%) patients. No signs of cricoarytenoid joint impairment were found.
ConclusionsOrganic larynx involvement was uncommon in patients with RA. However symptoms and signs of pharyngeal–laryngeal reflux were seen in around 60% of patients. There was no correlation between the clinical phenotype, severity of disease, immunological profile or treatment with VLS findings.
Evaluar la afectación laríngea en pacientes con AR en la práctica diaria y correlacionar los hallazgos con las diferentes manifestaciones de la enfermedad, incluyendo la gravedad de la misma.
MétodosRealizamos un estudio transversal a 36 pacientes consecutivos diagnosticados de AR a los cuales se les realizó una exploración sistemática de su enfermedad, una anamnesis dirigida para síntomas de reflujo y valoración del índice de discapacidad vocal. La exploración laríngea se realizó mediante videolaringoestroboscopia (VLE).
ResultadosEl tiempo medio de evolución de la enfermedad fue de 2,6±3,4 años. El requerimiento vocal se consideró profesional en 12 pacientes (33,3%). Veinticuatro (67%) pacientes presentaron algún hallazgo patológico en la VLE. Se evidenciaron nódulos en bambú en una paciente (2,8%), signos de disfonía hipertónica en 11 pacientes (30,6%) y en 23 pacientes (63,9%) se evidenciaron síntomas y signos de reflujo faringolaríngeo (RFL). No se observaron alteraciones de la movilidad cricoaritenoidea.
ConclusionesEn nuestra cohorte las lesiones laríngeas valoradas por VLE en la AR son poco frecuentes. No obstante, alrededor del 60% de los pacientes presenta síntomas y signos de RFL. Dichos hallazgos no se correlacionaron con las características clínicas, la gravedad o el tratamiento de la enfermedad.
Laryngeal manifestations of rheumatoid arthritis (RA) are poorly described and generally include cricoarytenoid (CA) joint involvement, rheumatoid nodules on the vocal cords and dryness symptoms associated with Sjögren's syndrome (SS).1,2 The prevalence of laryngeal clinical involvement in RA has been estimated between 15% and 70% of patients3–5 and in post mortem series between 45% and 88% of patients.1
Dysphonia, cough, foreign body sensation, stridor or snoring are usually the main symptoms of laryngeal involvement in RA, although sometimes it may be asymptomatic. The diagnosis depends on high clinical suspicion and a good examination by indirect laryngoscopy or videolaryngostroboscopy (VLE).6
VLE is a minimally invasive clinical tool that allows the clinician to identify the etiology of voice disorders by analyzing images of the larynx in high resolution. In addition to reporting the appearance of the glottis, VLE provides data on the vibratory pattern of the vocal mucosa. VLE is the only method of analyzing both the ripple of the mucosa and successive opening/closing movements of the vocal cords. This allows the detection of minimal lesions (small areas of fibrosis, intracordal injury, asymmetric vibration) that would have been overlooked with rigid endoscopy studies or fibrolaryngoscopy.7 The limitations of VLE are few. The presence of severe nausea despite the use of topical anesthesia, a very short phonation time (less than 3s), strongly aperiodic phonation and the existence of low intensity voice can hinder adequate imaging for evaluation.7
Although VLE is a standard technique in otolaryngology, there is little information on using VLE for laryngeal involvement in patients with RA.
Our objective was to evaluate laryngeal involvement in patients with RA in daily practice regardless of the presence or absence of laryngeal symptoms and to correlate the findings with the various manifestations of the disease, including the severity thereof.
MethodsWe studied a cross-sectional cohort of 36 consecutive patients diagnosed with RA (ACR 1987 criteria). We assessed clinical variables that included age, gender, duration of disease, smoking history, extra-articular involvement, the patient's immunological profile, including rheumatoid factor (RF) and anti-CCP antibody (CPC-2) and treatment at the time of the study, including disease-modifying drugs, proton pump inhibitors (PPIs) and NSAIDs. We also determined disease activity by the DAS-28 index.
Additionally, we collected a number of variables designed to assess laryngeal involvement in RA, including patient history, assessment of reflux symptoms by the Reflux Symptom Index (RSI)8 and the assessment of vocal disorders using the Vocal Handicap Index (VHI-10). An RSI greater than 5 is highly indicative of RFL. The VHI-10 is a questionnaire developed to quantify the impact perceived by a subject affected by a voice disorder in the areas of vocal function itself, physical ability associated with it and emotions causing dysphonia.9 The VHI is divided into four categories, according to the results, as follows: 0–9 normal, 10–20 mild disability, 21–30 moderate disability and 31–40 severe disability.
The laryngeal examination was performed using a Karl Storz PULSAR VLE™ II. The VLE was analyzed for the presence of specific laryngeal lesions, including signs of RFL by the Reflux Finding Score (RFS)10 as well as signs of hypertonics functional dysphonia or alteration in the mobility of the CA joint. A greater than 11 RFS is highly indicative of RFL. The different rates used in this study are explained in Annexes 1–3.
Laryngeal lesions were considered as functional or structural and functional lesions. Organic lesions include polyps, nodules, cysts and scars, among others. Indirect reflux signs are equivalent to organic lesions but are not specific and include hyperemia, thickening and edema but assessment is subjective. Functional lesions due to overuse or misuse of the voice include, among others, hypertonicity and hypotonicity. In order to determine if there was correlation between clinical variables and VLE findings, we used parametric tests (Student's t test) for dichotomous variables and continuous variables with normal distribution. To perform these calculations we used the statistical program SPSS v20.
All patients signed informed consent prior to the procedure. In all cases, the VLE was for diagnostic purposes only, without any therapeutic intervention.
ResultsClinical FeaturesThe sample included 3 men (8.3%) and 33 women (91.7%) with a mean age of 56.3±14.2 years (range 28–86). The median time to disease progression was 2.6±3.4 years. Nineteen patients were smokers, 5 (13.9%) at present and 14 (38.9%) in the past. The general characteristics set of patients included in the study are summarized in Table 1.
General Characteristics of the 36 Patients With RA and VLE.
| Females (%) | 92 |
| Time since onset of the disease, years (%) | 2.6±3.1 |
| Current age, years (mean±SD) | 14.2±56.3 |
| Previous smokers (%) | 39 |
| Active smokers (%) | 14 |
| Extraarticular involvement (%) | 25 |
| Associated Sjögren syndrome (%) | 8 |
| Subcutaneous nodules (%) | 20 |
| RF (%) | 80 |
| RF titers, IU (mean±SD) | 164.1±190.6 |
| CCP2 (%) | 69 |
| CCP2 titers, IU (mean±SD) | 719±664.4 |
| Erosive disease (%) | 33 |
| Number of previous DMARDs (mean±SD) | 1.7±0.8 |
| Treatment with MTX (%) | 89 |
| Biological treatment (%) | 24 |
| Concomitant use of PPIs (%) | 39 |
| Concomitant use of NSAIDs (%) | 39 |
| Remission (DAS-28 <2.6) (%) | 37 |
NSAIDs, NSAIDs; SD, standard deviation; DMARD, disease-modifying drugs; RF, rheumatoid factor; PPi, proton pump inhibitors.
The vocal requirement was considered usual in 24 patients (66.6%) and professional in 12 patients (33.3%), and none of them were highly demanding of their voice.
At the time of the study, 37% of patients were in remission (DAS-28 index <2.6). Thirty-two patients (88.9%) received methotrexate (MTX), 19 (52.8%) received corticosteroids (usually at low doses, <5mg/day) and a 24% received biological treatment.
ENT StudyThe RSI was 4.6±4.1 (range 0–15) and the VHI-10 was 1.1±2.8 (range 0–16). Twenty-four (67%) patients had some type of alteration in the VLE. In 23 patients (63.9%) there were indirect signs of RFL with a RFS of 2.6±2.9 (range 0–15), 11 patients (30.6%) were diagnosed with hypertonic dysphonia and in one patient (2.8%) bamboo type laryngeal nodules were apparent.11 No alterations in CA mobility were observed.
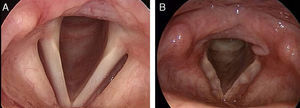
The patient with laryngeal nodules, a 41-year-old female, had a 5-year, non-erosive, seronegative for RF and CCP2 RA history, but with positive antibodies against chimeric citrullinated peptides fibrin/filaggrin and was treated with MTX.12 The patient reported a history of moderate but persistent dysphonia lasting for 6 months, with no other associated symptoms. The ENT study showed, through VLE, rounded lesions of a “pearly” submucosal location in the folds of the vocal cords (Fig. 1).
We did not perform excision of the nodules due to the fear of speech worsening secondary to surgery. Suspecting Nodulosis induced by MTX, treatment was stopped and switched to leflunomide (10mg/day), achieving good control of disease activity without significant changes in voice. After 6 months of discontinuing MTX, a new VLE was performed, which showed no significant changes from baseline. The patient currently continues with a mild degree of dysphonia and remission of RA.
Correlations Between the Videolaryngostroboscopy Findings and Clinical FeaturesStrobe lesions were significantly correlated with age (P=.04) and with the RSI and RFS indices (P<.0001 for both). There was no correlation between lesions in the presence of strobe with RF or anti-CCP, with a history of smoking, extra-articular involvement, the severity of the disease or the antirheumatic treatment received. Similarly, no correlation was found between RFL signs and concomitant treatment with PPI or NSAID.
DiscussionThe prevalence of laryngeal involvement in RA is highly variable, depending on the series studied and the technique used. The first series reported an involvement in 26%–52% of patients.3,13 Postmortem studies have demonstrated an involvement of the CA as such villous synovial proliferation, similar to RA14 synovitis.
In the present series of patients with RA, we found that specific laryngeal lesions seen using VLE in RA are rare. However, about 60% of patients had isolated RFL symptoms and signs. These findings did not correlate with the clinical characteristics, severity or treatment of disease.
The different sets of patients with laryngeal affection and RA published to date are summarized in Table 2. The low prevalence of organic lesions in our patients compared with other series3,13,15 can be explained by several reasons: (a) most of the patients in our series had laryngeal symptoms, (b) the vast majority of series include patients with long-standing RA (mean follow-up of 10 years), our series included patients with recent onset RA with a mean follow-up of 2 years; and finally, (c) the majority of the series were made prior to the era of biological therapies. All patients received treatment with disease-modifying drugs since the early stages of the disease and, additionally, a quarter of patients were receiving biologic therapy.
laryngeal Involvement in RA in the Published Series.
| Author, reference | Year and place of study | No. of patients | Scanning technique | Top findings |
| Lofgren and Montegomery3 | 1962, Boston, USA | 100 | Physical examination and indirect laryngoscopy | CA Involvement: 26%Greater involvement in women and in patients with active RA |
| Jurik and Pedersen4 | 1984, Aarhus, Denmark | 22 | Radiology simple and indirect laryngoscopy | CA Involvement: 45%.Greater involvement in women |
| Lawry et al.5 | 1984, California, USA | 45 | Indirect laryngoscopy and laryngeal CT | Alterations in laryngoscopy: 52%Alterations in the vocal cords: 55%CA Involvement: 27% (CT) |
| Brazeau-Lamontagne et al.13 | 1986, Québec, Canada | 32 | Indirect laryngoscopy and laryngeal CT | Alterations in laryngoscopy: 72%.Alterations in the TC: 75% |
| Castro et al.15 | 2012, São Paulo, Brazil | 27 | VLE | Alterations in the VLE: 48% of patients, mainly with erythematous arytenoid subluxation |
| Current series | Barcelona, Spain | 36 | VLE | Signs of RFL: 64%Hypertonic dysphonia: 30.6%BAmboo nodules: 2.8% |
To date, we only know of a recently published Brazilian study that evaluated laryngeal involvement by VLE in a series of 27 patients with RA.15 However, this study did not assess disease activity or information was unavailable on its length, immunological profile and background treatment.
We must recognize that our study has several limitations, including the small sample size and the lack of a control group. In the present study we found a high proportion of symptoms and signs of RFL in spite of the fact that more than one-third of the patients received treatment with PPIs. The prevalence of reflux esophagitis in healthy subjects ranges between 6% and 23%.16 Reflux has been reported in up to 50% of patients attending ENT consultation for voice problems.17 A recent study that evaluated the presence of gastrointestinal symptoms in patients with RA and a control group, found that the prevalence of gastroesophageal reflux symptoms was similar in both groups.18 However, the non-specificity of the symptoms and signs of RFL has been mentioned in the literature, with some authors suggesting the need for confirmation of reflux with more specific tests for a correct diagnosis.19 The lack of confirmation with pH-metry in our series could therefore justify our findings, making it difficult to draw conclusions in this regard.
The case of the patient with bamboo nodules is of note in our study. This is a benign lesion of the vocal cords (bamboo nodes), described as isolated instances in a number of autoimmune diseases, including systemic lupus erythematosus, SS, systemic sclerosis and RA, among others.11
Currently, there is no consensus on the treatment of benign lesions of the vocal cords associated with autoimmune diseases. In our case, we chose a conservative treatment and clinical follow-up.
The rheumatologist current perception is that extra-articular manifestations of RA are less frequent, although not all studies have confirmed this perception.20 Probably tighter and earlier control of the disease, the use of more effective therapies, such as biologic therapies, and implementing better diagnostic and monitoring tools (such as ultrasound or MRI) enable a lower expression of different extra-articular manifestations of the disease, including laryngeal involvement.
Conflict of InterestThe authors declare no conflict of interest.
| During the last month, how do the following problems affect you? | 0=No problem5=Great difficulty | |||||
| 1. Hoarseness or voice problems | 0 | 1 | 2 | 3 | 4 | 5 |
| 2. Throat clearing | 0 | 1 | 2 | 3 | 4 | 5 |
| 3. Excess mucus in the throat or nose | 0 | 1 | 2 | 3 | 4 | 5 |
| 4. Difficulty swallowing liquids, solids or medications | 0 | 1 | 2 | 3 | 4 | 5 |
| 5. Coughing after eating or lying down | 0 | 1 | 2 | 3 | 4 | 5 |
| 6. Difficulty breathing or coughing | 0 | 1 | 2 | 3 | 4 | 5 |
| 7. Annoying cough | 0 | 1 | 2 | 3 | 4 | 5 |
| 8. foreign body sensation | 0 | 1 | 2 | 3 | 4 | 5 |
| 9. Burning pain, chest pain, epigastric pain | 0 | 1 | 2 | 3 | 4 | 5 |
| Total | ||||||
10 items scored from 0 to 4.
0=never, 1=almost never, 2=sometimes, 3=usually, 4=always.
| 0 | 1 | 2 | 3 | 4 | ||
| 1. | People have difficulty hearing me because my voice | |||||
| 2. | People do not understand in noisy environments | |||||
| 3. | My voice problems alter my personal and social life | |||||
| 4. | I feel displaced from conversations due to my voice | |||||
| 5. | My voice problem affects job performance | |||||
| 6. | I feel I need to tighten the throat to produce voice | |||||
| 7. | The quality of my voice is unpredictable | |||||
| 8. | My voice annoys me | |||||
| 9. | My voice makes me feel some disability | |||||
| 10. | People ask me what's wrong with my voice? |
Standard value: 0–9; mild disability: 10–20; moderate disability: 21–30; severe disability: 31–40.
Reflux Findings Index (Reflux Findings Score [RFS]).
A score greater than 11 in a proper clinical situation is highly indicative of RFL.
Laryngeal and pharyngeal complications of gastroesophageal reflux disease. GI Motility online (2006), doi: 10.1038/gimo46.
| Find | Score |
| Subglottic edema | 2=present0=absent |
| Ventricular obliteration | 2=partial4=complete |
| Eritemia/hyperemia | 2=Only arytenoid4=diffuse |
| Edema of vocal cords | 1=mild2=moderate3=severe4=polypoid |
| Diffuse laryngeal edema | 1=mild2=moderate3=severe4=obstructive |
| Hypertrophy of the posterior commissure | 1=mild2=moderate3=severe4=obstructive |
| Granuloma/granulation | 2=present0=absent |
| Endolaryngeal mucus/other | 2=present0=absent |
| Total | |
Please cite this article as: Gómez-Puerta JA, Cisternas A, Hernández MV, Ruiz-Esquide V, Vilaseca I, Sanmartí R. Valoración laríngea mediante videolaringoestroboscopia en pacientes con artritis reumatoide. Reumatol Clin. 2014;10:32–36.