Nitrofurantoin is an antibiotic widely used in the treatment and prevention of urinary tract infections (UTI). The most common adverse effects are gastrointestinal but cases of pulmonary and hepatic1 toxicity, and even vasculitis2 have been reported.
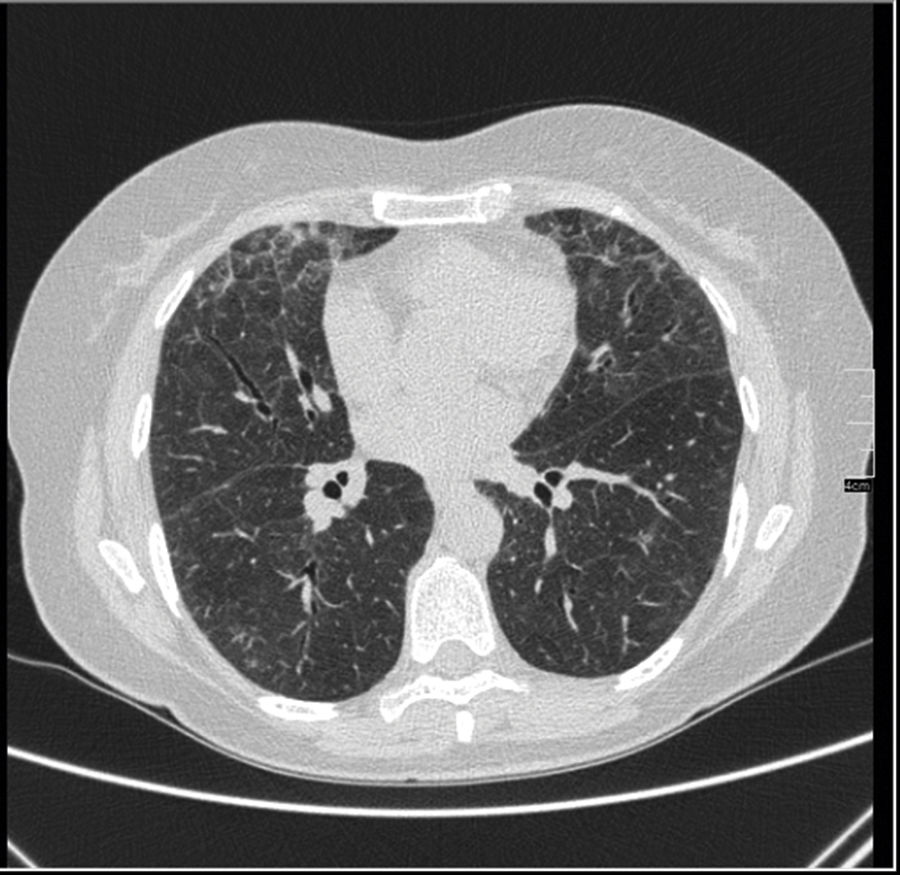
We present the case of a 63-year-old woman with a history of repetitive UTI, with no other relevant medical history. Prophylaxis with nitrofurantoin had been initiated a year prior to the presentation of symptoms. She was referred to the rheumatology department for migratory asymmetrical arthralgias of 4-month onset. During examination she referred to dyspnoea with moderate effort which had appeared after the arthralgias. Auscultation revealed bilateral crackling sounds. A chest X-ray showed a bilateral interstitial pattern and high resolution computerised tomography (HRCT) showed ground glass areas corresponding to acute/sub acute interstitial pneumonia (Fig. 1). Blood tests highlighted GOT 360U/l, GPT 432U/l and GGT 279U/l with normal abdominal ultrasound. The hepatropos virus serology and autoimmune antibody study tested negative. Autoimmunity studies detected ANCA+ 1/640 perinuclear staining (negative anti-myeloperoxidase and anti-proteinase 3). Due to these findings toxicity by nitrofurantoin was suspected and the drug was withdrawn. Treatment with prednisone was established, with a good response at respiratory level, a drop in hepatic enzymes and a complete resolution of arthralgias. During follow-up, the transaminase values remained normal, respiratory symptoms disappeared and posterior lung imaging tests were normal. The arthralgias abated and the ANCAs tested negative.
There have been case reports of concomitant pulmonary and hepatic toxicity attributed to the use of nitrofurantoin.3 Pulmonary toxicity and hepatic toxicity have 2 types of presentations: acute and chronic. Chronic pulmonary toxicity symptoms develop after several months of treatment. The most common are dyspnoea, irritative cough and fatigue. Crackling sounds, especially around the lung bases4 are usually the result of auscultation. All types of radiographic anomalies in most patients exist, mostly in inferior and bilateral fields. In the HRCT scan ground glass areas may be observed, together with septal enlargement and traction bronquiectasias.5
The acute form of hepatic toxicity generally presents after only a few weeks of treatment and is uncommon. It is usually accompanied by fever and rash.6 Normally withdrawing the medication resolves this, although cases of fulminant hepatitis3 have been known to exist. The more common chronic disorder may present months or years later. Symptoms are usually fatigue, muscle weakness and jaundice and an increase of transaminases in lab tests. Autoimmunity markers are occasionally detected (ANA+, anti-ML antibodies and elevated IgG).1 Recovery after the removal of the drug is usually slow and hepatic damage may persist.6
In the event of suspected diagnosis the temporary relationship between the onset of symptoms and exposure to the drug must be sought. Treatment is based on withdrawal of nitrofurantoin. Although glucocorticoids are usually combined with it, it is believed that the symptoms may cease after discontinuation of the drug.1
Prognosis is good if there is an early suspected diagnosis and exposure to the drug is limited. A case of cutaneous vasculitis and positive anti-MPO renal ANCA associated with the use of nitrofurantoin2 has been reported. In our case the ANCAs tested positive although without vasculitis-associated specificity. Given the patient's favourable evolution no hepatic or pulmonary biopsies were performed which could have highlighted vasculitis. We did not find any cases of arthralgias with simultaneous pulmonary and hepatic involvement with positive ANCA related to the use of nitrofurantoin. In this case the arthralgias were the predominant symptom and led to the detection of concomitant pulmonary and hepatic toxicity. We therefore believe that the involvement of joints may suggest systemic toxicity and its early detection may improve prognosis.
Please cite this article as: Arévalo Ruales K, Ivorra Cortés J, Román Ivorra J, Martinez Francés M. Artralgias migratorias: manifestación inicial de toxicidad sistémica asociada al tratamiento crónico con nitrofurantoína. Reumatol Clin. 2020;16:432–433.