Methotrexate-induced pneumonitis is a serious (mortality: 13%–20%)1 but uncommon (0.3%–7.5%)2,3 complication of treatment with this folic acid antagonist in patients with rheumatoid arthritis (RA) and other diseases. The typical onset is characterised by an acute picture of nonproductive cough, dyspnoea, and fever, within the first year of treatment, most commonly during the first months (mean: 36–78 weeks),4 and irrespective of scheduled dose, patient's smoking habit, and gender. The following risk factors have been identified: advanced age, extra-articular manifestations of rheumatoid arthritis (mainly pulmonary involvement), diabetes, and elevated creatinine levels.5 If this condition is suspected, methotrexate should be immediately discontinued, and respiratory support and systemic steroids at medium-high doses should be initiated; it is also recommended to associate a broad-spectrum antibiotic, with coverage for Pneumocystis jirovecii,6 until the infectious origin is ruled out.1
We present the case of a 68-year-old female patient, who in February 2013 was diagnosed with seronegative rheumatoid arthritis in the context of high blood pressure and type II diabetes mellitus with secondary sensorimotor axonal polyneuropathy. We started oral treatment with prednisone 30mg/day and methotrexate 10mg/week. After eight weeks, a partial improvement was observed; for this reason, methotrexate dose was increased to 15mg/week and steroid dose was reduced.
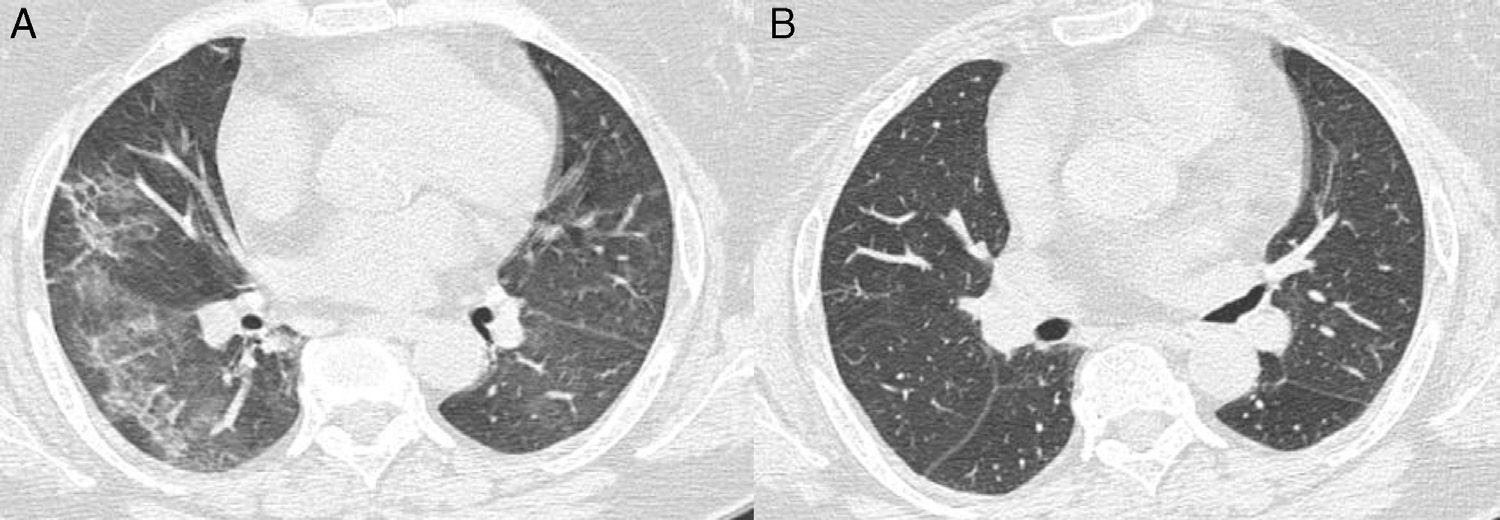
Two months later, the patient presented at the ER of our hospital with 24-h-course dyspnoea, cough, sweating, nausea, fever, and dizziness. Physical examination: BP 92/56mmHg, HR 110bpm, SaO2 86%, T 38.4°C, glycaemia 178mg/dL, Glasgow index 15/15, negative meningeal signs, tenderness on abdominal palpation. Of the complementary tests, the most significant data include: ECG: sinus tachycardia 100bpm with isolated ventricular extrasystole; abdominal ultrasound: normal; chest X-ray: bilateral diffuse alveolar consolidation and cardiomegaly (the X-ray performed before treatment start was reported as normal); haemogram: haemoglobin 11.4g/dL, haematocrit 34.4%, MCV 104fL; coagulation: Quick's test 51%, d-dimer: 5109ng/mL; gasometry: lactic acid 5.8mmol/L, pH 7.52; creatinine: 1.8mg/dL (normal values in previous tests); procalcitonin 0.11ng/mL; pro-BNP: 9130pg/mL; urine sediment: normal. The patient was admitted to the Intensive Care Unit, where respiratory support (Mk-reservoir 12lpm and, subsequently, CPAP) and empiric antibiotic therapy with imipenem, along with low doses of noradrenaline and methylprednisolone IV, were initiated; methotrexate was discontinued. Serial blood culture and urine culture were negative, and the echocardiography was normal. Bronchoalveolar lavage was not performed.7 After 48h, an improvement in her condition and the laboratory values was observed; for this reason, she was transferred to the ward, where two days later she was asymptomatic and oxygen therapy was no longer required. A pulmonary CT was performed (Fig. 1A) where the presence of a predominantly peripheral bilateral extensive ground-glass opacity was confirmed, associated with minimum subpleural lung consolidations in the right lower lobe; the preserved lung parenchyma was normal. The patient was discharged with oral steroid treatment (0.5mg/kg) for control at the outpatient offices; oral sulfasalazine was added, and it was discontinued a few weeks later due to hair loss, abdominal pain, and palpable purpura in abdomen and upper part of limbs. Therefore, we continue treatment with oral prednisolone alone in a down-titration schedule up to a maintenance dose of 7.5mg/d. A few weeks later, the patient was completely recovered.
Ten months later, a control high-resolution computed axial tomography scan was performed (Fig. 1B), showing normal lung parenchyma and no ground-glass opacity. Currently, the patient continues in clinical remission of RA and has returned completely to her normal activity.
Since this condition, although rare, is considered to have potential severity, we urge the reader to suspect it when a patient on treatment with methotrexate presents with a clinical picture compatible with respiratory tract infection and/or heart failure.
Please cite this article as: Fernández Matilla M, Fernández-Llanio Comella N, Castellano Cuesta JA. Neumonitis inducida por metotrexato en una paciente con artritis reumatoide seronegativa. Reumatol Clin. 2015;11:190–191.