Among the extraintestinal manifestations of inflammatory bowel disease (IBD), pyoderma gangrenosum (PG) often poses a therapeutic challenge. We describe two cases of PG associated with inflammatory bowel disease, who responded to treatment with Infliximab.
Dentro de las manifestaciones extraintestinales de la enfermedad inflamatoria intestinal (EII), el pioderma gangrenoso (PG) plantea con frecuencia dificultades terapéuticas. Describimos 2 casos de PG asociados a enfermedad inflamatoria intestinal, con buena respuesta al tratamiento con infliximab.
Pyoderma gangrenosum (PG) is a neutrophilic dermatosis of unknown cause that manifests as painful skin ulcers. It was described by Brunsting et al.1 in 1930. Approximately 50% of patients have a background systemic disease, the most common being inflammatory bowel disease (IBD), myeloproliferative disorders, and different forms of arthropathy (both spondylitis and rheumatoid arthritis).2 Sometimes skin lesions can precede, follow, or occur simultaneously with the disease with which it is associated. In some patients with IBD, control of bowel disease also leads to the control of PG, but this does not occur in all patients. The diagnosis is based on clinical suspicion and exclusion of other causes of ulceration by histology and microbiological studies.
Clinical CasesCase 1Male patient, 55 years old with a history of type 2 DM, HLA-B27+ankylosing spondylitis, diagnosed at 18 years of age, followed up by the rheumatology service and treated with sulfasalazine. The patient had Gleason 7 acynar adenocarcinoma of the prostate (T2-3N0M0 p) and was operated by radical prostatectomy in September 2008, subsequently receiving adjuvant radiotherapy from January through March 2009. He also presented cellulitis and a perianal abscess. No other relevant history was present.
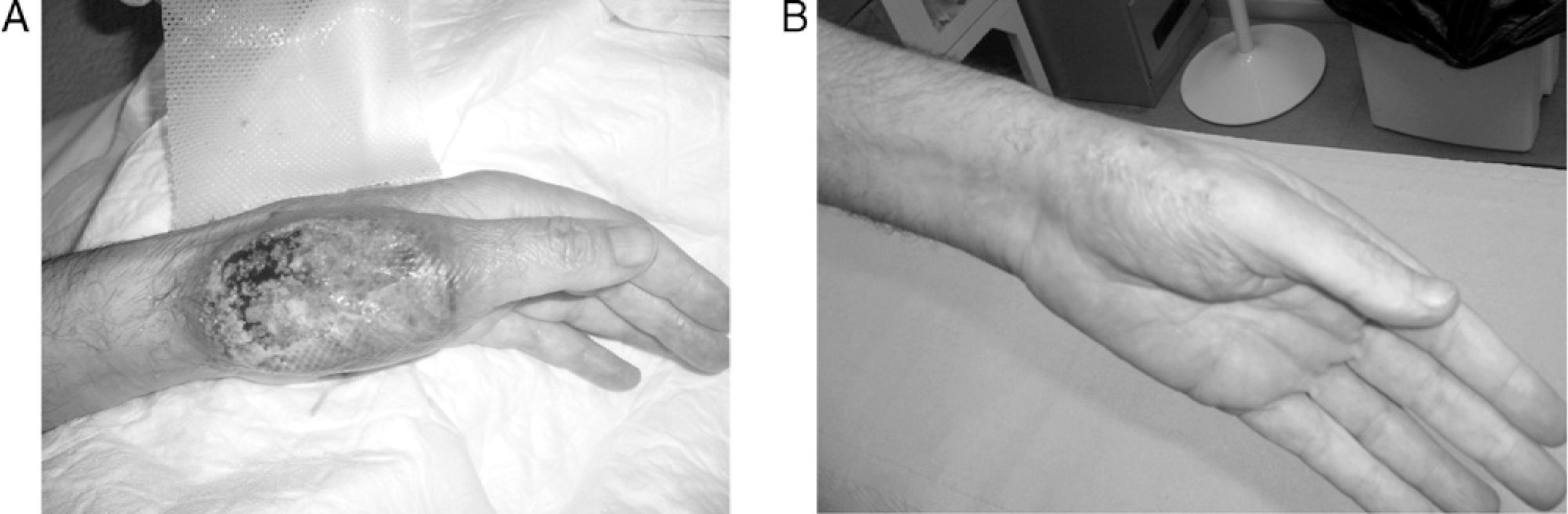
The patient was hospitalized (July 7, 2009) for presenting an ulcerated lesion with loss of substance and a purplish erythematous halo on the back of the left hand (Fig. 1A), in addition to severe fistulizing perianal lesions. He had no fever, abdominal pain, or altered bowel habits, nor joint, eye, or constitutional symptoms.
On examination, the patient had mucocutaneous pallor. The abdomen showed no tenderness or other abnormalities on examination. It showed two skin ulcers on the back of the left hand, infiltrated, with a jagged edge, elevated and erythematous, painful to the touch, with a fibrinous background and hemorrhagic exudation. We performed a skin biopsy of the ulcers’ margin. The next day, the ulcer had expanded aggressively into that margin. In the perianal region there were severe fistulizing lesions.
The CBC only showed normochromic normocytic anemia, hemoglobin of 11.6g/dl and hematocrit of 33.2%, without changes in basic biochemistry, liver function, or hemostasis. There was elevated C-reactive protein (11.63mg/dl). Serologic testing for hepatitis B and C, human immunodeficiency virus, and syphilis were negative as were rheumatoid factor and antinuclear antibodies. Electroimmunoforesis, quantification of immunoglobulins, complement levels, and blood smear showed no abnormalities.
The histological study of the biopsied skin ulcer showed necrosis of the epidermis and dermis, with a mixed inflammatory infiltrate and abscess formation at the base. The edge of the ulcer showed pseudoepitheliomatous hyperplasia. We did not detect bacteria, fungi, parasites, or cytopathic effects induced by viral infection. Biopsy cultures for bacteria, mycobacteria, and fungi were negative.
The colonoscopy revealed a severe impairment and a pancolonic perianal fistulizing pattern. The colon mucosal biopsy showed ulceration and architectural distortion, with acute and chronic inflammatory signs.
Due to the symptoms, signs, histological findings of skin lesions, and the exclusion of other diseases through microbiological testing, the patient was diagnosed with Crohn's disease associated with PG.
Initially, the progression was favorable after treatment with intravenous corticosteroids, but the patient later showed new lesions on both forearms, also suggestive of pyoderma.
Due to the severity of the disease, we opted for the use of infliximab with the approval of the oncology and gastroenterology departments. After ruling out latent TB, treatment was begun with anti-TNF alpha.
After starting therapy with infliximab (5mg/kg), the patient progressed favorably, with progressive improvement of skin (Fig. 1B) and bowel lesions and is currently under maintenance therapy with infliximab every 8 weeks after completing the induction with good response.
Case 233-year-old male with a history of Crohn's disease of several years of progression, treated with mesalazine. He presented frequent outbreaks of intestinal disease and polyarthritis, which required treatment with corticosteroids.
One week before admission, the patient had a painful ulceration on the right perimalleolar region appear and begins to suppurate without fever or gastrointestinal symptoms. Because of the suspicion of septic arthritis, we performed a surgical drainage of the abscess in addition to starting intravenous antibiotic therapy with unfavorable results. A few days later, there was necrosis of the surgical wound with great loss of substance, showing progressive worsening after each lavage.
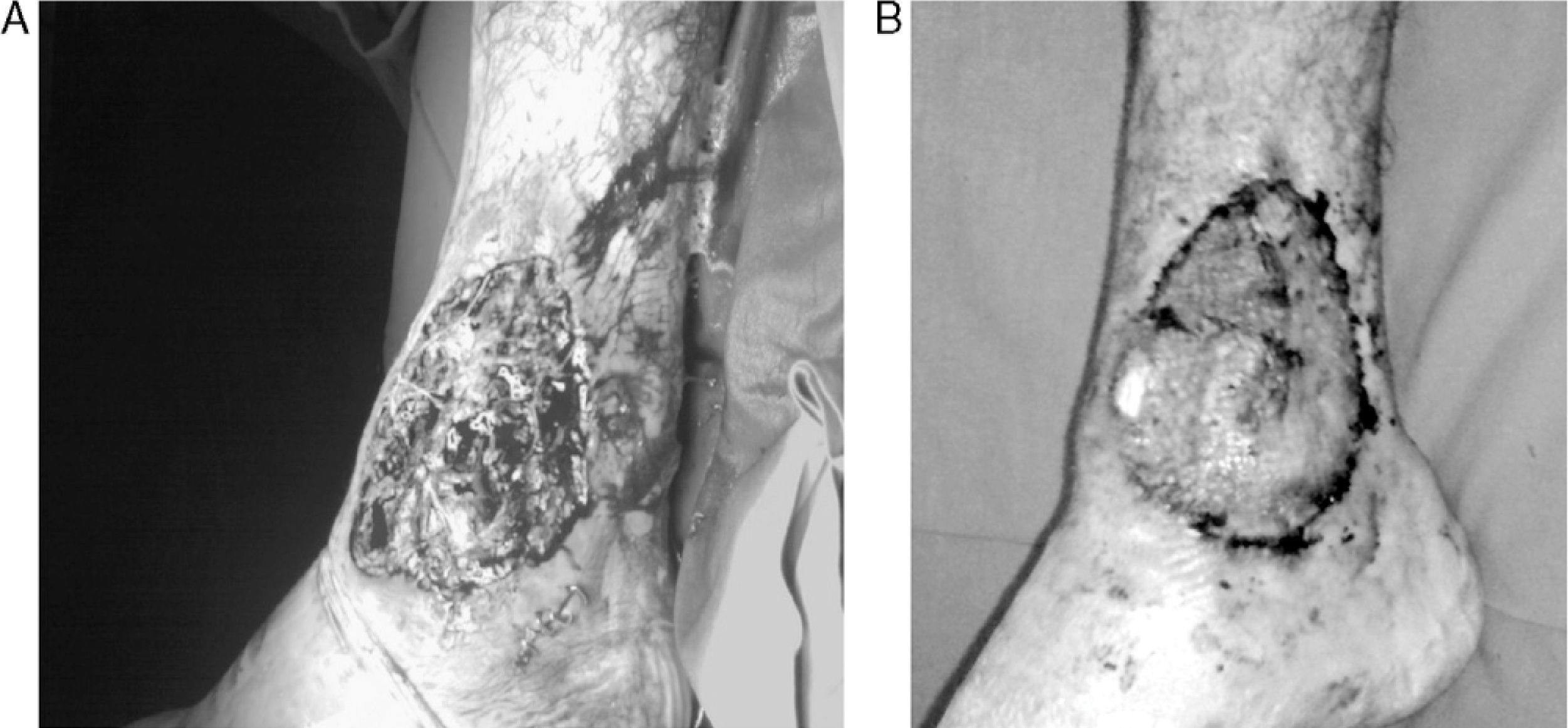
After his hospitalization (September 15, 2007), the patient presented fever, abdominal pain, and diarrhea (more than 20 stools per day), with pathological features. The patient had mucocutaneous pallor, with general malaise and abdominal tenderness. Upon the anal inspection, he presented several tracts and drainage sites. His right ankle had a skin ulcer, with significant loss of tissue (Fig. 2A).
He also presented significant anemia (hemoglobin 7.9g/dl, hematocrit 23.2%), WBC 24300 with 77% PMN, platelets 647000. The basic biochemistry, liver profile, and hemostasis tests were normal. There were elevated acute phase reactants (CRP: 12.3mg/dl and ESR 82mm/h). Serologic testing for hepatitis B and C, human immunodeficiency virus, and syphilis were negative. Mantoux and rheumatoid factor and antinuclear antibodies were also negative.
The colonoscopy revealed colon Crohn's disease with severe activity. We performed an MRI of the abdomen and pelvis, which showed severe involvement of the descending colon, sigmoid and rectum with loss of haustrae, edema of the colon wall and perirectal fat and severe complex and bilateral perianal fistulizing disease.
Parenteral nutrition was begun in the operating room and catheterization was performed for perianal fistula drainage with placement of two separate drains, partially improving intestinal function.
Steroid and antibiotic treatment, in addition to general measures, improved the patient's general condition without achieving success regarding the right ankle ulcer. A biopsy was taken from the wound edge and was compatible with PG.
Treatment was initiated with intravenous infliximab (5mg/kg), with dramatic improvement. Gradually, the patient achieved remission of bowel disease. The ulcer required a skin graft to cover the severe loss of substance (Fig. 2B).
DiscussionExtraintestinal manifestations complicate the course and treatment of IBD in 20%–40% of patients.2 Among the extraintestinal manifestations, mucocutaneous PG appears in 1%–5% of patients with IBD.3
It is more common in ulcerative colitis than Crohn's disease, and manifests itself initially as painful pustules that increase in size forming ulcers with purple edges and a necrotic base, may be multiple and scars after healing. It is most frequently located in the lower extremities.2
PG can respond to the basic treatment of IBD, but its relationship disease activity is less obvious than in other mucocutaneous extraintestinal manifestations, such as erythema nodosum.3
The pathogenesis of PG is not fully elucidated but appears to be an immune-mediated injury similar to IBD. Therefore, various therapies that act to control the inflammatory response, such as infliximab, have been used in its treatment. It has also been speculated that the effect of infliximab in PG is a consequence of the healing of intestinal lesions underlying IBD, or is a direct drug effect on skin4 injuries.
The use of infliximab on extraintestinal manifestations such as mucocutaneous PG has recently been described in some publications of small series or isolated cases5,6 and opens new perspectives in its management. The skin lesions responded well in most cases. The dosing of infliximab used in cases published is very diverse and in many of them chose an initial infusion and then at weeks 2 and 6, and a significant percentage of new doses were administered thereafter. In our case, we chose to follow the recommendations of the Spanish Group for the Study of Crohn's disease and ulcerative colitis.7
On the other hand, there are studies in which it has been shown that patients with chronic skin ulcers, such as PG, have an increased risk of serious infections (septic shock) while undergoing treatment with anti-TNF alpha, so individual prophylaxis should be provided before initiation of treatment.8
ConclusionsIn the cases reported, treatment with infliximab proved to be able to achieve remission of PG associated with Crohn's disease after failure of immunosuppressive therapy.
DisclosuresThe authors have no disclosures to make.
Please cite this article as: Carrasco Cubero C, et al. Pioderma gangrenoso asociado a enfermedad inflamatoria intestinal. Descripción de 2 casos con buena respuesta a infliximab. Reumatol Clin. 2012;8(2):90-2.