The patient was a 55-year-old woman with a 4-month history of pain in left flank that irradiated to the lumbar region. Computed tomography revealed a cystic tumor in the retroperitoneal region that compresses the ureter and left renal pelvis in contact with pancreatic body and tail. Surgery was performed and the definitive pathological report diagnosed nodular retroperitoneal fibrosis associated with IgG4; Ki67-positive in germinal centers (5%) and IgG4-positive (40 plasma cells in 3 fields of 40×) by immunohistochemistry. Retroperitoneal fibrosis is a rare disease, that develops gradually and has an excellent response to steroid management. Surgical treatment is reserved for cases that compromise adjacent structures. Thus, identifying it when studying a retroperitoneal tumor leads to better prognosis and survival.
Paciente de 55 años de edad con cuadro de dolor en flanco izquierdo irradiado a región lumbar de 4 meses de evolución, con tomografía axial computarizada que reporta tumoración quística en región retroperitoneal que comprime uréter y sistema pielocaliceal izquierdo en contacto con cuerpo y cola de páncreas. Es intervenida quirúrgicamente y se encuentra en reporte patológico definitivo fibrosis retroperitoneal nodular asociada a IgG4; con Ki67 positivo en centros germinales (5%) e IgG4 positivo (40 células plasmáticas en 3 campos de 40×) por inmunohistoquímica. La fibrosis retroperitoneal nodular es una enfermedad poco frecuente, de evolución paulatina con excelente respuesta al manejo con esteroides. El tratamiento quirúrgico se reserva para casos que comprometen estructuras adyacentes, por lo que el identificarlo al estudiar una tumoración retroperitoneal conlleva un mejor pronóstico y sobrevida.
Retroperitoneal fibrosis (RPF) associated with IgG4 is a disease of inflammatory and autoimmune origen.1 A rate of 1/100,000 and prevalence of 1.4/100,0002 have been reported. The average age at diagnosis is 50 and it presents 2–3 times more in men than in women.3 It is characterised by the histopathological appearance of a high number of IgG4+ plasmatic cells.
We present the case of a 55-year-old patient with a diagnosis of RPF associated with IgG4 and surgically treated by resection.
Case ReportA 55-year-old woman who had had a caesarean section 21 years before and an open appendectomy 3 years before, with no history of pancreatitis. She presented with a 4-month history of pain in the left flank that irradiated to the lumbar region, with no other symptoms on examination and no signs of dry syndrome or palpable lymphadenopathies. Computed tomography of the abdomen revealed a cystic tumour in the retroperitoneal region which compressed the ureter and the left pyelokaliceal system in contact with the pancreatic body and tail. Biochemical tests were requested which reported 95 serous amylase, 38 lipase, CA 19-9 antigen: 23.6 and CA 125: 6.4.
A double-J catheter was inserted into the left ureter with discreet resistance in its path and a surgical approach was decided upon. A solid tumour was found to be attached to the deep tissues in the retroperitoneal space, to the left of the inferior vena cava, which protruded through the mesentery and was in close contact with the kidney, left pelvis and anterior surface of the aorta, where signs of major inflammation were observed. A surgical specimen was sent to the pathology department for examination, comprising the tumour, left kidney and perirenal and suprarrenal ipsolateral fat. The postoperative period passed without event and the patient was discharged on day three. The patient is currently being managed by the rheumatology department with low doses of steroids, has not presented with any relapses and does not require corticosteroid-sparing agents.
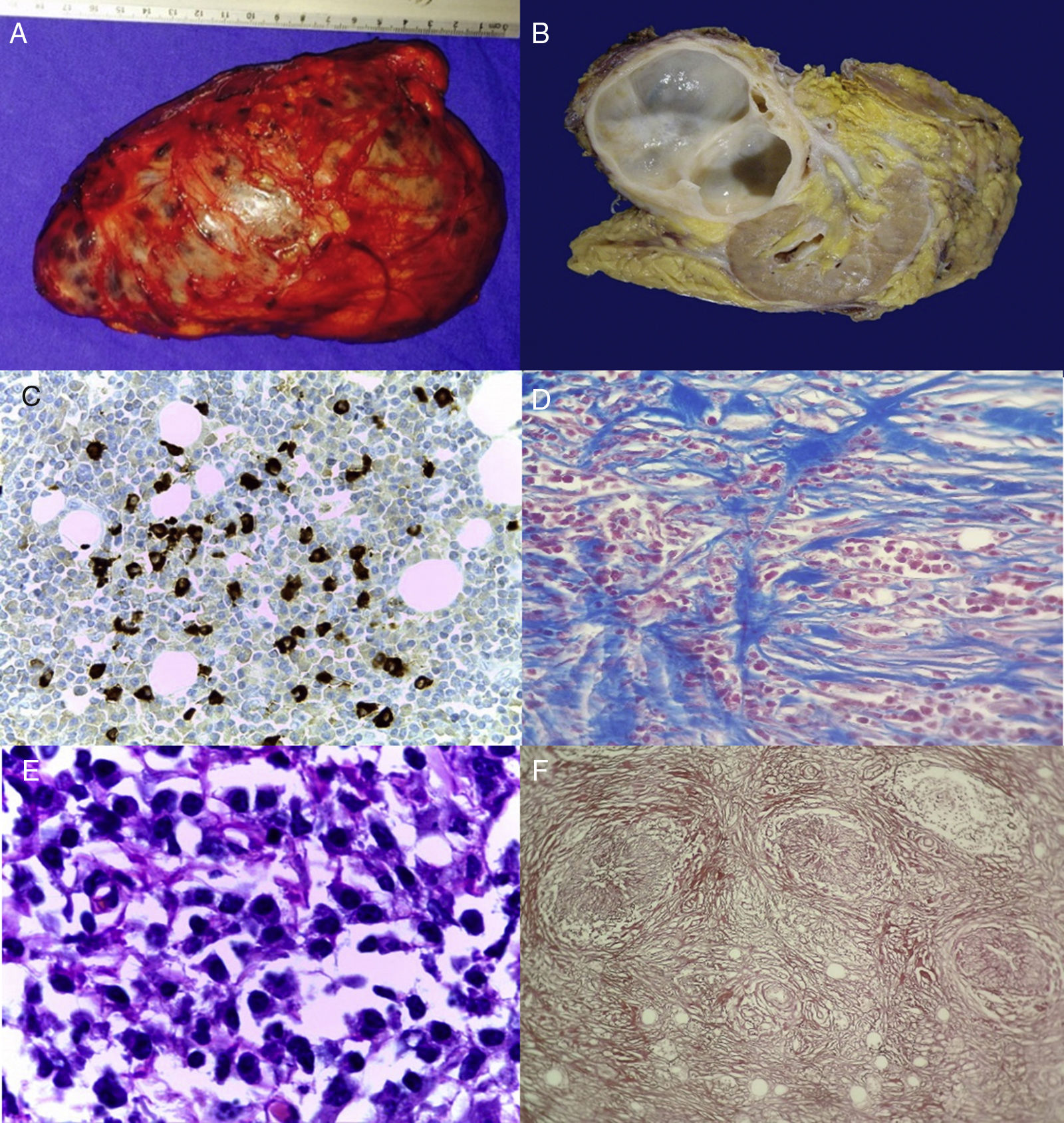
The definitive pathological report diagnosed nodular retroperitoneal fibrosis associated with IgG4, with Ki67-positive in germinal centres (5%) and IgG4-postiive (40 plasma cells in 3 fields of 40×) by immunohistochemistry (Fig. 1).
(A) Macroscopic tumour. (B) Surgical specimen, solid well defined tumour, fibrous in appearance, which does not invade the renal parenchyma. (C) Microphotography (40×). Reaction of the indirect immunoperoxidase with anti-IgG4 antibody, with over 40 plasmatic cells. (D) Microphotography (40×) with Mason staining. Fibrosis with focally steriform pattern. (E) Microphotography (100×). Inflammatory infiltrate predominantly composed of plasmatic cells. (F) Microphotography (10×) obliterating phlebitis consistent with extensive fibrosis and lymphoplasmacytic infiltrate.
IgG4-related disease was the name given during the previous decade to an entity characterised by swelling lesions, dense lymphoplasmacytic infiltrate with abundant IgG4 positive cells, storiform fibrosis and frequently, but not always, raised IgG41 serous levels.
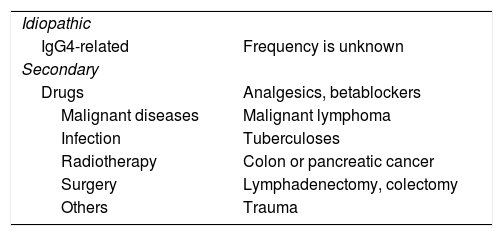
RPF is a rare inflammatory process which involves the retroperitoneal region on the fourth lumbar vertebra, may involve and compress one or both ureters in over 60% of cases and the abdominal vasculature (aorta and inferior vena cava).1,2 in general, RPF is divided into 2 types: idiopathic RF (IRPF), where there is no one direct cause for its appearance and which is essentially a diagnosis of exclusion, and secondary RF (SRPF) which is associated with several causes such as drugs, diverse infections and malignant tumours.2,5 (Table 1). At present, Riedel thyroiditis (fibrosing thyroiditis), Küttner tumour (increase in the size of submandibular glands with fribrosis within them), RPF and Mikulicz disease are classified within the IgG41-related disease spectrum.
Causes of Retroperitoneal Fibrosis.
| Idiopathic | |
| IgG4-related | Frequency is unknown |
| Secondary | |
| Drugs | Analgesics, betablockers |
| Malignant diseases | Malignant lymphoma |
| Infection | Tuberculoses |
| Radiotherapy | Colon or pancreatic cancer |
| Surgery | Lymphadenectomy, colectomy |
| Others | Trauma |
Source: taken from Corradi et al.4
The most common RPF symptoms include abdominal pain, jaundice from oedema and infiltrate of pancreatic and bile ducts, weight loss and exocrine or endocrine pancreatic failure.1,3 There is no internationally accepted criteria for the diagnosis of IgG4-related diseases.1 Three histopathological findings present in the patient and define the disease in the affected organ. They are as follows: (1) the presence of storiform pattern sclerosis; (2) a dense lymphoplasmacytic infiltrate and (3) a raised proportion of IgG4 positive cells from immunohistochemistry compared with IgG1 positive cells.6,7
The first line of treatment in RPF is renal level decompression through drainage, as in the case of our patient, combined with high steroid dose therapy.3 The goals are to induce regression of fibroinflammatory reaction, release the ureteral and retroperitoneal structure obstruction, stop the acute inflammatory reaction phase and its systemic manifestations and prevent recurrence.7 However, it has been reported that in cases where the fibrosis component predominates, a surgical approach may be useful.1 Disease remission has been reported in up to 75%–95% of cases but relapses are frequent.1,3
ConclusionsRPF should form part of the differential diagnosis in the case of retroperitoneal tumours, since a timely diagnosis will improve treatment, patient follow-up and prognosis.
Ethical LiabilitiesProtection of people and animalsThe authors declare that for this research no experimentation has been carried out on human beings or animals.
Data confidentialityThe authors declare that they have adhered to the protocol of their place of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ruiz Mar G, Cárdenas Serrano ÓE, Roldan García J, Cañavera-Constantino A, Menéndez Trejo VM, Chapa Azuela Ó. Fibrosis retroperitoneal nodular asociada a IgG4 como diagnóstico diferencial en tumores retroperitoneales. Reporte de un caso. Reumatol Clin. 2019;15:e27–e29.