Shrinking lung syndrome (SLS) is a rare manifestation of systemic lupus erythematosus. We report the case of a patient with non-responding SLS (neither to glucocorticoids nor immunosupresors), who showed remarkable improvement after the onset of treatment with rituximab. Although there is a little evidence, treatment with rituximab could be proposed in SLS when classical treatment fails.
El síndrome del pulmón encogido (SPE) es una manifestación poco frecuente del lupus eritematoso sistémico. Exponemos el caso de una paciente afectada de SPE, refractario al tratamiento con glucocorticoides e inmunosupresores, que tras el inicio de tratamiento con rituximab presentó marcada mejoría de los síntomas. Aunque la evidencia es escasa, el tratamiento con rituximab podría ser propuesto en el SPE cuando fracasa el tratamiento clásico.
Shrunken lung syndrome (SLS) is a rare manifestation of some autoimmune diseases such as systemic lupus erythematosus (SLE). It is characterized by a restrictive type ventilatory defect and should be suspected in patients with SLE presenting unexplained dyspnea. Treatment is not well established. Although the use of systemic corticosteroids as first-line treatment has been proposed in refractory cases, other immunosuppressive drugs, such as rituximab, have been suggested.
Clinical CaseThe patient was a 57-year-old female followed by the Rheumatology Department since age 22, diagnosed with SLE in the context of fever, polyarticular pain, malar rash, and photosensitivity. She presented antinuclear antibodies 1/320 (normal <1/40), anti-native DNA 50.00IU/ml (normal <15), IgG anticardiolipin 20.23GPL/ml (normal 0.00–7.70), and positive anti-histone antibodies. She was initially treated with prednisone (15g/day) and chloroquine (155mg/day) with good response.
At age 29, due to an episode of focal segmental glomerulonephritis, treatment with azathioprine was added 50m g/12h, with complete remission.
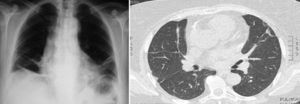
Years later, she presented moderate dyspnea accompanied by dry cough and pleuritic pain, and was evaluated by pneumology. She had crackling rales in the lung bases on auscultation. The chest X-ray showed elevation of both hemidiaphragms and bibasilar atelectasis (Fig. 1). The pulmonary function tests (September 2008) showed an intense restrictive ventilatory defect, moderate decrease in the diffusion capacity of carbon monoxide, which fully corrected by alveolar volume, along with a slight decrease in peak inspiratory pressure (Table 1). A chest computed tomography confirmed the loss of volume in both lungs and the presence of atelectasis in the bases (Fig. 1).
With these data, she was diagnosed with SLS associated with SLE. It was decided to increase the dose of prednisone to 30mg/day, associated with an inhaled beta-2 adrenergic, with good initial clinical response.
When trying to lower the dose of glucocorticoids (March 2009), the patient had a worsening of respiratory symptoms, with mild effort dyspnea and chest pain. Upon detection of lymphopenia and positivity of biomarkers (increased levels of anti-DNA antibodies and consumption of C4 complement), we decided to maintain the same previous dose of prednisone and azathioprine, adding mycophenolate mofetil at a dose of 720mg/12h. Six months later, she presented a new outbreak of arthritis, so the combined treatment was discontinued and rituximab was initiated (2 doses of 1g separated by 15 days were administered; this pattern has been repeated every 6 months until publication).
Under the established treatment, a progressive improvement in both the symptoms and the lung function tests (May 2011–April 2013) (Table 1) was seen, making it possible to reduce the dose of prednisone to 5mg/24h; she has remained clinically stable until this report.
DiscussionWe present the case of a patient who had SLS, who showed no significant clinical improvement with the classic treatment with corticosteroids and immunosuppressants, but which was achieved after initiation of rituximab.
It is known that the pleuropulmonary involvement in SLE is present in 60%–80% of patients 1, wherein SLS is one of the less common manifestations.2 Its prevalence is 7%,3 higher in women with severe SLE refractory to treatment.1
The presenting symptoms are dyspnea and chest pain. Auscultation is usually normal.4,5
Respiratory function shows a restrictive type of ventilatory defect with reduced lung volumes. Imaging tests show no evidence of pleural, parenchymal or vascular disease.1,2
The cause of the SLS is not known.1–3 There are several hypotheses including the presence of atelectasis by the loss of surfactant6,3,4 diaphragmatic myopathy, phrenic neuropathy, pleural adhesions, and inactivation of the diaphragm induced by pain.3 SLS has also been linked to anti-Ro antibody.2,3,7 None of these theories has been confirmed.
The long-term prognosis is generally good, with clinical stabilization or improvement.8 Deterioration appears in only 2% of cases, requiring aggressive therapy8,9 or even mechanical ventilation.
There is no definitive treatment of SLS, although glucocorticoids are considered the first line therapy, alone or in combination with other immunosuppressive agents.1 In addition, theophylline and beta-2 agonists are used with the intention to increase diaphragmatic strength.1,3
On the other hand, there has been much improvement both of pleuritic pain and of dyspnea in patients treated with rituximab. Rituximab is a chimeric mouse/human monoclonal antibody that specifically binds to the CD20 antigen expressed on pre-B and mature B lymphocytes. Although no prospective study of rituximab in SLS has been performed, isolated cases have been reported where refractory patients experience symptom improvement with increased exercise tolerance, and an improvement in respiratory function tests with increasing expiratory volume in the first second and forced vital capacity.3,10
ConclusionSo far, the treatment of choice for SLS is corticosteroids alone or in combination. Refractory cases may benefit from treatment with rituximab.
Ethical ResponsibilitiesProtection of persons and animalsThe authors state that no experiments were performed on persons or animals for this study.
Data confidentialityThe authors state that they have followed their workplace protocols regarding the publication of patient data and all patients included in the study have received enough information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors state that they have obtained informed consent from patients and/or subjects referred to in this article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflicts of interest.
Please cite this article as: Peñacoba Toribio P, Córica Albani ME, Mayos Pérez M, Rodríguez de la Serna A. Rituximab en el tratamiento del síndrome del pulmón encogido del lupus eritematoso sistémico. Reumatol Clin. 2013;10:325–327.