Patients with systemic lupus erythematosus (SLE) and anti-Ro+ antibody frequently pose a diagnostic and therapeutic challenge for the specialist, as they frequently present sicca syndrome, overlapping with Sjögren's syndrome (SS). To date, the clinical and prognostic variability that this antibody confers on SLE patients is not well characterized.
ObjectivesTo investigate the possible clinical, analytical, therapeutic and prognostic implications of anti-Ro antibody in SLE. Furthermore, we analyzed the possible implications of the expressed anti-Ro profile (subunit 52, 60 or both) on the disease phenotype.
MethodsThe medical records of patients with anti-Ro+ and - SLE, primary SS and SLE/SS overlap have been reviewed.
ResultsAnti-Ro+ SLE presents less arthritis, low C4, expression of DNA Crithidia and need for bolus corticosteroids than anti-Ro− SLE, but more xerophthalmia, xerostomia, expression of anti-La, anti-cyclic citrullinated peptide and overlap with other rheumatological entities. Anti-Ro+ SLE and the overlap group behave similarly for multiple variables. SS group shows a higher expression of β2-microglobulin compared to the overlap group. Anti-Ro52+ patients associate more Raynaud's phenomenon than anti-Ro60+ patients. The latter express more lupus anticoagulant and antiphospholipid antibodies than the group with both subunits.
ConclusionsThe presence of anti-Ro+ in patients with SLE provides clinical and analytical differences compared to patients with anti-Ro− SLE and SLE/SS. anti-Ro+ SLE and the overlap group behave similarly, but present differential characteristics that postulate them as separate phenotypes of the disease. The different serological profiles of anti-Ro confer specific clinical and analytical characteristics in patients with SLE and SS.
Los pacientes con lupus eritematoso sistémico (LES) y anticuerpos anti-Ro+ suponen con frecuencia un reto diagnóstico y terapéutico para el especialista, ya que presentan, con frecuencia, síndrome seco, solapado con síndrome de Sjögren (SS). Hasta la fecha, la variabilidad clínica y pronóstica que confiere este anticuerpo a los pacientes con LES no está bien caracterizada.
ObjetivosInvestigar las posibles implicaciones clínicas, analíticas, terapéuticas y pronósticas del anticuerpo anti-Ro en el LES. Además, analizamos las posibles implicaciones del perfil anti-Ro expresado (subunidad 52, 60 o ambas) en el fenotipo de la enfermedad.
MétodosSe han revisado las historias clínicas de los pacientes con LES anti-Ro+ y −, SS primario y solapamiento LES/SS.
ResultadosEl LES anti-Ro+ presenta menos artritis, bajo C4, expresión de ADN Crithidia y necesidad de corticoides en bolo que el LES anti-Ro-, pero más xeroftalmia, xerostomía, expresión de anti-La, antipéptido cíclico citrulinado y solapamiento con otras entidades reumatológicas. El LES anti-Ro+ y el grupo solapado se comportan de forma similar para múltiples variables. El grupo SS muestra mayor expresión de β2-microglobulina respecto al grupo solapado. Los pacientes anti-Ro52+ asocian más fenómeno de Raynaud que los pacientes anti-Ro60+. Estos últimos expresan más anticuerpos anticoagulantes lúpicos y antifosfolípidos que el grupo con ambas subunidades.
ConclusionesLa presencia de anti-Ro+ en los pacientes con LES aporta diferencias clínicas y analíticas respecto a los pacientes con LES anti-Ro- y LES/SS. El LES anti-Ro+ y el grupo solapado se comportan de forma similar, pero presentan características diferenciales que los postulan como fenotipos separados de la enfermedad. Los diferentes perfiles serológicos de anti-Ro confieren características clínicas y analíticas específicas en los pacientes con LES y SS.
SLE is a chronic autoimmune disease of unknown etiology with an estimated prevalence of 210/100,000 inhabitants in Spain.1 Its pathogenesis is complex and can affect several organs and systems. It presents a wide symptomatologic variability, and there are indications that this variability could be associated with the presence of different antibody profiles,2 which could act as biomarkers of different aspects of the disease. Some of these antibodies are included in the different classifying criteria of the disease (antinuclear antibody (ANA), anti-double stranded DNA (ds-DNA), anti-Sm, lupus anticoagulant, anti-β2glycoprotein (β2GPP), anti-cardiolipin (ACL)), while others are not (anti-Ro/SSA, anti La/SSB, anti-ribonucleoprotein (RNP)), despite being very common in SLE. Within this last group, patients with anti-Ro/SSA+ SLE can pose a diagnostic and therapeutic challenge for the specialist, since they often present xerophthalmia and xerostomia, as well as other manifestations of SS, resulting in an overlap between both entities.
Anti-Ro/SSA antibody is associated with 4 diseases: SLE, primary SS, subacute cutaneous lupus, and congenital heart block. There are two subunits of this antibody: anti-Ro52 (more typical of SS) and anti-Ro60 (more typical of SLE).3,4 The prevalence of anti-Ro/SSA antibody in patients with SLE ranges between 25 and 50%, and between 40 and 95% in those with primary SS,2 with its positivity in SS being one of the criteria of the group of the American College of Rheumatology/European League Against Rheumatism (EULAR/ACR) with a higher weight for its classification.5
Recent data in the literature indicate that the phenotypes of different connective tissue diseases and their clinical implications can vary significantly in patients with different anti-Ro antibody profiles, indicating the potential diagnostic and prognostic value of these antibodies in clinical practice.6 The previously cited study has investigated the clinical characteristics of individuals with different connective tissue diseases according to the expressed anti-Ro antibody profile (subunit 52+, 60+ or both), associating some of these groups with a higher incidence of serious manifestations such as diffuse interstitial pulmonary disease (DILD) or pulmonary hypertension (PHT).6 However, there is a lack of data in the literature comparing clinical characteristics and prognosis between patients with anti-Ro+ and − SLE and, within the former, according to which subunit of the antibody they present.
In SLE, early diagnosis and treatment are essential, since 50% of the patients can develop organic damage in the 5 years after diagnosis and up to 32% during the first year.7 Therefore, it seems essential to us to investigate the clinical and prognostic implications of anti-Ro antibody in this pathology, in order to achieve a better characterization of these patients according to their serological profile. Likewise, we consider of great clinical relevance to assess whether the role of anti-Ro differs in patients with isolated primary SS and in those with SLE/SS overlap, given the involvement of anti-Ro in both entities and the overlap of symptoms between both, which occurs on many occasions in clinical practice.
The objective of the present work is to assess the possible demographic, clinical, analytical, therapeutic and prognostic implications attributable to anti-Ro antibody in patients with SLE, primary SS and with overlap of both entities. Secondarily, we will analyze the possible implications of the expressed anti-Ro profile (subunit 52, 60 or both) on the disease phenotype of the patients under study.
Material and methodsStudy designA retrospective observational study was conducted, in which we compared the clinical, demographic, analytical, therapeutic and prognostic profiles of four subgroups of patients.
Study population, inclusion and exclusion criteriaThe medical records of 830 patients from the cohort of patients with SLE and with primary SS who are currently undergoing follow-up or have been followed up in the Rheumatology service of the Hospital del Mar (Barcelona, Spain) were reviewed from 2006, when electronical medical records started, to the end of 2023, until discharge, death or transfer out of the area. 144 patients have been included in the study, divided into 4 subgroups of between 31 and 42 patients each, according to the disease and presence of anti-Ro:
- 1.
with SLE anti-dsDNA+ anti-Ro−,
- 2.
with SLE anti-dsDNA− anti-Ro+,
- 3.
patients with overlapping SLE and SS,
- 4.
patients with primary SS.
Patients must met one of the SLE classification criteria (ACR 1997, Systemic Lupus International Collaborating Clinics 2012 or ACR/EULAR 2019 criteria)8–10 and/or SS classification criteria (American-European Consensus Group 2002 or ACR/EULAR 2016),5 depending on the subgroup to which they belonged, for inclusion. Groups 1 and 4 were included as controls for groups 2 and 3. Those patients who did not meet the classification criteria were excluded from the study.
This project was approved by the Ethics Committee of Hospital del Mar (project approval code: 2023/11269).
Definition of study variablesDemographic, immunological, analytical and urinary parameters were included as well as specific clinical variables of SLE and of SS, variables related to treatment and the calculation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus (SLICC).11 Anti-Ro antibodies were analyzed through multiplex immunoassay that differentiates the two subunits anti-Ro52 and anti-Ro60 and anti-dsDNA by two methods: enzyme linked immunoassay (ELISA) and the Crithidia luciliae indirect immunofluorescence test (Crithidia). Patients needed to have at least two positive determinations of the anti-Ro or the anti-dsDNA antibody to be included in their respective groups. To define prognosis, we performed a survival analysis of the presence of accumulated damage represented by a SLICC≥1 from the time of diagnosis to time of the medical history review for this study. This analysis could only be performed between the three groups of patients with SLE, as SLICC cannot be measured in patients with isolated SS.
Statistical analysisSPSS version 25.0 was used for the statistical analysis of the data. The χ2 and ANOVA test were performed for categorical and continuous variables, respectively. Post hoc analysis to compare pairwise groups was performed using Z test and Tukey's HSD test. The survival analysis was performed through a Kaplan–Meier analysis with log-rank (Mantel–Cox) pairwise comparison between the three SLE groups.
ResultsFig. 1 shows the flux diagram for patient selection.
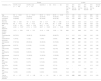
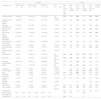
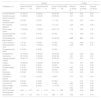
The results obtained are presented below. Tables 1–3 show the demographic, clinical, therapeutic and analytical differences observed between groups.
Results of the demographic and therapeutic variables by disease group and differences observed between them.
| Groups | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables (n, %) | Anti-Ro− SLE (n=38) | Anti-Ro+ SLE (n=31) | SLE/SS (n=33) | SS (n=42) | Anti-Ro− SLE vs. anti-Ro+ SLE | Anti-Ro− SLE vs. SLE/SS | Anti-Ro− SLE vs. SS | Anti-Ro+ SLE vs. SLE/SS | Anti-Ro+ SLE vs. SS | SLE/SS vs. SS |
| Age | 58±16.40 | 51±15.30 | 55.70±15.10 | 60.15±14.06 | 0.11 | 0.66 | 0.50 | 0.19 | 0.01 | 0.23 |
| Female sex | 34 (89.50) | 30 (96.80) | 32 (97.00) | 40 (95.20) | 0.24 | 0.22 | 0.33 | 0.96 | 0.74 | 0.70 |
| Caucasian ethnicity | 33 (86.80) | 21 (67.70) | 25 (75.80) | 26 (61.90) | 0.06 | 0.23 | 0.01 | 0.47 | 0.60 | 0.20 |
| Size (cm) | 160±6.60 | 161±6.54 | 160±6.71 | 160±6.65 | 0.15 | 0.82 | 0.36 | 0.10 | 0.12 | 0.47 |
| Weight (kg) | 69±14.70 | 64±11.02 | 64±12.20 | 65±12.80 | 0.14 | 0.07 | 0.75 | 0.56 | 0.26 | 0.12 |
| BMI | 27.34±5.81 | 24.24±3.96 | 24.67±4.67 | 27±5.85 | 0.04 | 0.06 | 0.84 | 0.90 | 0.06 | 0.09 |
| Age at diagnosis | 42.92±19.37 | 41.74±15.35 | 42.27±15.96 | 49.12±16.39 | 0.96 | 0.96 | 0.08 | 0.90 | 0.06 | 0.07 |
| Disease duration (years) | 14.74±8.84 | 9.35±5.21 | 12.18±9.88 | 10.64±7.05 | 0.01 | 0.11 | 0.03 | 0.61 | 0.23 | 0.91 |
| Corticosteroids ever | 29 (76.31) | 18 (58.10) | 20 (60.60) | 28 (66.70) | 0.11 | 0.15 | 0.34 | 0.84 | 0.45 | 0.59 |
| Corticosteroid bolus ever | 7 (18.42) | 1 (3.22) | 1 (3.00) | 2 (4.80) | 0.05 | 0.04 | 0.05 | 0.96 | 0.74 | 0.70 |
| Antimalarials ever | 37 (97.40) | 28 (90.32) | 30 (90.90) | 33 (78.60) | 0.21 | 0.24 | 0.01 | 0.94 | 0.18 | 0.15 |
| Mycophenolate ever | 9 (23.70) | 6 (19.35) | 5 (15.20) | 4 (9.50) | 0.66 | 0.37 | 0.09 | 0.66 | 0.23 | 0.46 |
| Leflunomide ever | 10 (26.40) | 2 (6.50) | 4 (12.10) | 9 (21.40) | 0.03 | 0.13 | 0.61 | 0.44 | 0.08 | 0.29 |
| Azathioprine ever | 13 (34.20) | 9 (29.00) | 7 (21.20) | 6 (14.30) | 0.65 | 0.22 | 0.04 | 0.47 | 0.12 | 0.43 |
| Methotrexate ever | 16 (42.10) | 10 (32.20) | 10 (30.30) | 10 (23.80) | 0.40 | 0.30 | 0.08 | 0.87 | 0.42 | 0.53 |
| Belimumab ever | 8 (21.10) | 0 (0.00) | 2 (6.10) | 0 (0.00) | 0.01 | 0.07 | 0.00 | 0.16 | – | 0.11 |
| Rituximab never | 1 (2.60) | 3 (9.70) | 5 (15.20) | 4 (9.50) | 0.21 | 0.06 | 0.20 | 0.51 | 0.98 | 0.46 |
| Anti-TNFα ever | 0 (0.00) | 0 (0.00) | 0 (0.00) | 3 (7.10) | – | – | 0.09 | – | 0.13 | 0.12 |
| Anifrolumab ever | 0 (0.00) | 1 (3.20) | 0 (0.00) | 0 (0.00) | 0.26 | – | – | 0.30 | 0.24 | – |
| Tacrolimus ever | 1 (2.60) | 2 (6.50) | 0 (0.00) | 0 (0.00) | 0.44 | 0.35 | 0.29 | 0.14 | 0.09 | – |
| Total of treatments received | 2.5±1.27 | 1.97±1.08 | 1.91±1.31 | 1.64±1.36 | 0.08 | 0.05 | 0.00 | 0.69 | 0.16 | 0.33 |
BMI: body mass index. Anti-TNFα: Tumor Necrosis Factor Alpha inhibitor.
Results of the clinical variables by disease group and differences observed between them. DILD: diffuse interstitial lung disease.
| Groups | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables (n, %) | Anti-Ro− SLE (n=38) | Anti-Ro+ SLE (n=31) | SLE/SS (n=33) | SS (n=42) | Anti-Ro− SLE vs. anti-Ro+ SLE | Anti-Ro− SLE vs. SLE/SS | Anti-Ro− SLE vs. SS | Anti-Ro+ SLE vs. SLE/SS | Anti-Ro+ SLE vs. SS | SLE/SS vs. SS |
| ≥2 joints arthritis | 32 (84.20) | 19 (61.30) | 25 (75.80) | 15 (35.70) | 0.03 | 0.37 | 0.00 | 0.21 | 0.03 | 0.00 |
| Cutaneous lupus (acute or chronic) | 23 (60.50) | 16 (51.60) | 24 (72.70) | 4 (9.50) | 0.46 | 0.28 | 0.00 | 0.08 | 0.00 | 0.00 |
| Subacute cutaneous lupus | 5 (13.20) | 4 (12.90) | 5 (15.20) | 1 (2.40) | 0.97 | 0.81 | 0.07 | 0.80 | 0.08 | 0.04 |
| Non-scarring alopecia | 12 (31.60) | 8 (25.80) | 8 (24.20) | 0 (0.00) | 0.60 | 0.49 | 0.00 | 0.88 | 0.00 | 0.00 |
| Oral or nasal ulcers | 20 (52.60) | 11 (35.50) | 19 (57.60) | 4 (9.50) | 0.15 | 0.67 | 0.00 | 0.07 | 0.01 | 0.00 |
| Serositis (pleuritis or pericarditis) | 5 (13.20) | 1 (3.20) | 4 (12.10) | 1 (2.40) | 0.14 | 0.90 | 0.07 | 0.18 | 0.83 | 0.09 |
| Raynaud's phenomenon | 9 (23.70) | 10 (32.30) | 12 (36.40) | 7 (16.70) | 0.43 | 0.24 | 0.43 | 0.73 | 0.12 | 0.05 |
| Lupus nephritis | 5 (13.20) | 2 (6.50) | 1 (3.00) | 0 (0.00) | 0.36 | 0.12 | 0.01 | 0.52 | 0.09 | 0.25 |
| Neuropsychiatric clinic | 2 (5.30) | 4 (12.90) | 4 (12.10) | 0 (0.00) | 0.27 | 0.30 | 0.13 | 0.92 | 0.02 | 0.02 |
| Congenital heart block | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | – | – | – | – | – | – |
| Xerophthalmia | 1 (2.60) | 12 (38.70) | 27 (81.80) | 38 (90.50) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 |
| Xerostomia | 0 (0.00) | 9 (29.00) | 26 (78.80) | 37 (88.10) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 |
| Arthralgia without arthritis | 35 (92.10) | 27 (87.10) | 28 (84.80) | 32 (76.20) | 0.49 | 0.33 | 0.05 | 0.80 | 0.24 | 0.35 |
| Fatigue | 8 (21.10) | 10 (32.30) | 19 (57.60) | 22 (52.40) | 0.29 | 0.00 | 0.00 | 0.04 | 0.09 | 0.65 |
| Lymphoma | 0 (0.00) | 0 (0.00) | 2 (6.10) | 2 (4.80) | – | 0.12 | 0.17 | 0.16 | 0.22 | 0.80 |
| Parotidomegaly | 0 (0.00) | 0 (0.00) | 5 (15.20) | 7 (16.70) | – | 0.01 | 0.01 | 0.02 | 0.02 | 0.86 |
| DILD | 1 (2.60) | 1 (3.20) | 3 (9.10) | 7 (16.70) | 0.88 | 0.24 | 0.04 | 0.33 | 0.07 | 0.34 |
| Peripheral neuropathy | 0 (0.00) | 2 (6.50) | 5 (15.20) | 3 (7.10) | 0.11 | 0.01 | 0.09 | 0.26 | 0.90 | 0.26 |
| Cutaneous purpura | 1 (2.60) | 0 (0.00) | 4 (12.10) | 1 (2.40) | 0.36 | 0.12 | 0.94 | 0.04 | 0.39 | 0.09 |
| Interstitial nephritis | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (4.80) | – | – | 0.17 | – | 0.22 | 0.20 |
| Clinical APS | 3 (7.90) | 1 (3.20) | 1 (3.00) | 1 (2.40) | 0.40 | 0.37 | 0.26 | 0.96 | 0.83 | 0.86 |
| Other overlaps | 2 (5.30) | 7 (22.60) | 6 (18.20) | 10 (23.80) | 0.03 | 0.08 | 0.02 | 0.66 | 0.90 | 0.55 |
| Overlap typea | 0.23 | 0.17 | 0.16 | 0.74 | 0.85 | 0.41 | ||||
| SLICC one year after diagnosis | 0.58±0.92 | 0.45±0.88 | 0.59±1.13 | – | 0.47 | 0.79 | – | 0.64 | – | – |
| Current SLICC | 1.42±1.75 | 0.67±1.14 | 1.15±1.52 | – | 0.04 | 0.47 | – | 0.17 | – | – |
APS: antiphospholipid syndrome. SLICC: Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus.
Results of the analytical variables by disease group and differences observed between them.
| Groups | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables (n, %) | Anti-Ro− SLE (n=38) | Anti-Ro+ SLE (n=31) | SLE/SS (n=33) | SS (n=42) | Anti-Ro− SLE vs. anti-Ro+ SLE | Anti-Ro− SLE vs. SLE/SS | Anti-Ro− SLE vs. SS | Anti-Ro+ SLE vs. SLE/SS | Anti-Ro+ SLE vs. SS | SLE/SS vs. SS |
| Hematuria | 20 (52.60) | 13 (46.40) | 19 (57.60) | 12 (32.40) | 0.62 | 0.67 | 0.07 | 0.38 | 0.25 | 0.03 |
| Leukocyturia | 21 (55.30) | 15 (53.60) | 23 (69.70) | 17 (45.90) | 0.90 | 0.21 | 0.42 | 0.19 | 0.54 | 0.04 |
| Proteinuria>0.5 g/24h | 5 (14.30) | 2 (7.10) | 2 (10.00) | 3 (12.00) | 0.37 | 0.64 | 0.80 | 0.72 | 0.55 | 0.83 |
| Hemolytic anemia | 3 (7.90) | 1 (3.20) | 3 (9.10) | 0 (0.00) | 0.41 | 0.85 | 0.06 | 0.33 | 0.25 | 0.05 |
| Leukopenia<4000/mm3 | 19 (50.00) | 19 (61.30) | 19 (57.60) | 17 (40.50) | 0.35 | 0.52 | 0.39 | 0.76 | 0.08 | 0.14 |
| Lymphopenia>1500/mm3 | 32 (84.20) | 25 (80.60) | 27 (81.80) | 36 (85.70) | 0.70 | 0.79 | 0.85 | 0.90 | 0.56 | 0.65 |
| Thrombocytopenia<100,000/mm3 | 4 (10.50) | 2 (6.50) | 2 (6.10) | 3 (7.10) | 0.55 | 0.50 | 0.59 | 0.95 | 0.90 | 0.85 |
| Low C3 | 22 (59.50) | 16 (51.60) | 12 (36.40) | 2 (4.80) | 0.52 | 0.05 | 0.00 | 0.22 | 0.00 | 0.00 |
| Low C4 | 16 (43.20) | 4 (12.90) | 6 (18.20) | 2 (4.80) | 0.01 | 0.02 | 0.00 | 0.56 | 0.21 | 0.06 |
| Low CH50 | 12 (32.40) | 5 (16.10) | 5 (15.20) | 1 (2.40) | 0.12 | 0.09 | 0.00 | 0.91 | 0.04 | 0.04 |
| Low complement ever | 28 (73.70) | 18 (58.10) | 13 (39.40) | 5 (11.90) | 0.17 | 0.00 | 0.00 | 0.13 | 0.00 | 0.00 |
| Anti-Ro 52 | 0 (0.00) | 19 (61.30) | 18 (54.50) | 30 (71.40) | 0.00 | 0.00 | 0.00 | 0.07 | 0.11 | 0.28 |
| Anti-Ro 60 | 0 (0.00) | 29 (93.50) | 32 (97.00) | 39 (92.90) | 0.00 | 0.00 | 0.00 | 0.21 | 0.66 | 0.44 |
| Anti-La | 0 (0.00) | 12 (38.70) | 15 (45.50) | 26 (61.90) | 0.00 | 0.00 | 0.00 | 0.58 | 0.05 | 0.15 |
| Anti-RNP | 11 (28.90) | 5 (16.10) | 5 (15.20) | 2 (5.00) | 0.21 | 0.16 | 0.00 | 0.91 | 0.12 | 0.14 |
| Anti-Sm | 6 (15.80) | 5 (16.10) | 2 (6.10) | 0 (0.00) | 0.97 | 0.19 | 0.01 | 0.20 | 0.01 | 0.11 |
| Anti-dsDNA | 38 (100.00) | 0 (0.00) | 10 (30.30) | 1 (3.00) | 0.00 | 0.00 | 0.00 | 0.00 | 0.33 | 0.00 |
| ANA maximum title | 1635±1563 | 1036±1049 | 1384±1408 | 1543±1390 | 0.94 | 0.93 | 0.96 | 0.97 | 0.85 | 1.00 |
| DNA crithidia | 21 (55.30) | 0 (0.00) | 6 (18.20) | 0 (0.00) | 0.00 | 0.92 | 0.11 | 0.00 | – | 0.12 |
| Rheumatoid factor | 7 (18.90) | 11 (37.90) | 18 (54.50) | 30 (71.40) | 0.08 | 0.00 | 0.00 | 0.19 | 0.00 | 0.13 |
| Polyclonal hypergammaglobulinemia | 3 (8.60) | 6 (26.10) | 11 (34.40) | 14 (34.10) | 0.07 | 0.01 | 0.01 | 0.51 | 0.50 | 0.98 |
| High β2-microglobulin | 7 (33.30) | 3 (14.30) | 7 (29.20) | 22 (59.50) | 0.15 | 0.73 | 0.06 | 0.23 | 0.00 | 0.02 |
| ACL-G | 6 (16.70) | 1 (3.20) | 2 (6.10) | 0 (0.00) | 0.07 | 0.17 | 0.03 | 0.59 | 0.36 | 0.20 |
| ACL-M | 6 (16.70) | 3 (9.70) | 5 (15.20) | 0 (0.00) | 0.40 | 0.86 | 0.03 | 0.50 | 0.10 | 0.04 |
| Anti-β2GPP IgG | 8 (22.20) | 2 (6.50) | 2 (6.10) | 1 (3.80) | 0.07 | 0.06 | 0.04 | 0.95 | 0.66 | 0.70 |
| Anti-β2GPP IgM | 6 (16.70) | 3 (9.70) | 4 (12.10) | 0 (0.00) | 0.40 | 0.59 | 0.03 | 0.75 | 0.10 | 0.07 |
| Lupus anticoagulant | 10 (27.80) | 5 (16.10) | 7 (21.20) | 2 (7.70) | 0.25 | 0.53 | 0.05 | 0.60 | 0.33 | 0.15 |
| APS antibodies | 14 (37.80) | 6 (19.40) | 7 (21.20) | 3 (11.50) | 0.09 | 0.13 | 0.02 | 0.85 | 0.42 | 0.32 |
| Anti-CCP | 0 (0.00) | 6 (20.70) | 3 (12.00) | 4 (12.50) | 0.07 | 0.04 | 0.04 | 0.40 | 0.39 | 0.95 |
ACL-G: anticardiolipin IgG. ACL-M: anticardiolipin IgM. Anti-β2GPPP: anti-β2glycoprotein. APS: antiphospholipid syndrome. Anti-CCP: anti-cyclic citrullinated peptide antibody.
Anti-Ro+ SLE presented less arthritis, lower C4, body mass index (BMI), DNA Crithidia expression, need for bolus corticosteroids, leflunomide and belimumab and lower current SLICC and disease duration than the anti-Ro− SLE group. However, they had more xerophthalmia, xerostomia, expression of anti-La, anti-cyclic citrullinated peptide (anti-CCP) and overlap with other rheumatological entities.
When comparing patients with SLE/SS versus those with anti-Ro - SLE, patients with the overlap showed more xerophthalmia, xerostomia, fatigue, and parotidomegaly. Furthermore, they had more peripheral neuropathy, polyclonal hypergammaglobulinemia and rheumatoid factor expression than patients with anti-Ro− SLE, and more cutaneous purpura than anti-Ro+ SLE patients. On the other hand, the anti-Ro+ and overlapping SLE group showed a similarity for multiple variables, such as the higher expression of anti-La and anti-CCP or the lower presence of low C4 and need for bolus corticosteroids in comparison with anti-Ro− patients. Analytically, the anti-Ro+ and overlap SLE group were similar throughout, except for a higher expression of DNA Crithidia in the latter.
Regarding the results of patients with SLE/SS and SS, the former presented more arthritis, cutaneous lupus, alopecia, oral or nasal ulcers, Raynaud's phenomenon, and neuropsychiatric symptoms than patients with SS. Analytically, patients with SLE/SS had more hematuria, leukocyturia, hemolytic anemia, hypocomplementemia, anti-dsDNA and ACL-M and less high β2-microglobulin than patients with SS.
Regarding patients with SLE and those with SS, multiple clinical differences were evident between both groups, especially with anti-Ro− SLE patients (see Tables 1–3).
In reference to the analysis by the expressed anti-Ro subunit, Tables 4–6 show the demographic, clinical, therapeutic and analytical differences observed between groups.
Results of the demographic and therapeutic variables according to the expressed anti-Ro antibody profile and differences observed between groups.
| Groups | p value | |||||
|---|---|---|---|---|---|---|
| Variables (n, %) | Group A:Anti-Ro 60+(n=37) | Group B:Anti-Ro 52+(n=4) | Group C:Anti-Ro 52 & 60+(n=63) | Group A vs. group B | Group A vs. group C | Group B vs. group C |
| Age | 56.41±15.96 | 65.50±14.48 | 54.97±14.68 | 0.23 | 0.74 | 0.14 |
| Female sex | 34 (91.90) | 4 (100.00) | 62 (98.40) | 0.55 | 0.10 | 0.80 |
| Caucasian ethnicity | 23 (62.20) | 2 (50.00) | 46 (73.00) | 0.64 | 0.26 | 0.32 |
| Size (cm) | 160.70±6.60 | 155.75±6.85 | 159.71±6.51 | 0.16 | 0.55 | 0.24 |
| Weight (kg) | 64.50±10.57 | 64.24±10.90 | 64.62±13.84 | 0.98 | 0.67 | 0.84 |
| BMI | 25.02±4.19 | 26.45±3.84 | 25.34±5.26 | 0.35 | 0.95 | 0.50 |
| Age at diagnosis | 47.41±15.95 | 57.75±14.29 | 42.40±16.02 | 0.14 | 0.16 | 0.08 |
| Disease duration (years) | 8.00±5.42 | 7.75±2.22 | 12.24±8.30 | 0.48 | 0.00 | 0.22 |
| Corticosteroids ever | 19 (51.40) | 3 (75.00) | 43 (68.30) | 0.37 | 0.09 | 0.78 |
| Corticosteroid bolus ever | 1 (2.70) | 0 (0.00) | 3 (4.80) | 0.11 | 0.61 | 0.65 |
| Antimalarials ever | 31 (83.80) | 3 (75.00) | 55 (87.30) | 0.66 | 0.62 | 0.48 |
| Mycophenolate ever | 3 (8.10) | 0 (0.00) | 3 (9.70) | 0.55 | 0.19 | 0.36 |
| Leflunomide ever | 5 (13.50) | 1 (25.00) | 9 (14.30) | 0.54 | 0.91 | 0.56 |
| Azathioprine ever | 7 (18.90) | 0 (0.00) | 14 (22.20) | 0.34 | 0.69 | 0.29 |
| Methotrexate ever | 14 (37.80) | 1 (25.00) | 14 (22.20) | 0.61 | 0.09 | 0.90 |
| Belimumab ever | 1 (2.70) | 0 (0.00) | 1 (1.60) | 0.74 | 0.70 | 0.80 |
| Rituximab ever | 1 (2.70) | 1 (25.00) | 9 (14.20) | 0.05 | 0.06 | 0.56 |
| Anti-TNFα ever | 2 (5.40) | 0 (0.00) | 1 (1.60) | 0.63 | 0.28 | 0.80 |
| Anifrolumab ever | 0 (0.00) | 0 (0.00) | 1 (1.60) | – | 0.44 | 0.80 |
| Tacrolimus ever | 0 (0.00) | 0 (0.00) | 2 (3.20) | – | 0.27 | 0.72 |
| Total of treatments received | 1.73±1.15 | 1.50±1.73 | 1.86±1.31 | 0.52 | 0.84 | 0.46 |
BMI: body mass index. Anti-TNFα: Tumor Necrosis Factor Alpha inhibitor.
Results of the clinical variables according to the expressed anti-Ro antibody profile and differences observed between groups.
| Groups | p value | |||||
|---|---|---|---|---|---|---|
| Variables (n, %) | Group A:Anti-Ro 60+(n=37) | Group B:Anti-Ro 52+(n=4) | Group C:Anti-Ro 52 & 60+(n=63) | Group A vs. group B | Group A vs. group C | Group B vs. group C |
| ≥2 joints arthritis | 21 (56.75) | 2 (50.00) | 35 (55.60) | 0.80 | 0.90 | 0.83 |
| Cutaneous lupus (acute or chronic) | 18 (48.64) | 1 (25.00) | 24 (38.00) | 0.37 | 0.30 | 0.60 |
| Subacute cutaneous lupus | 2 (5.40) | 0 (0.00) | 7 (11.10) | 0.63 | 0.33 | 0.48 |
| Non-scarring alopecia | 9 (27.32) | 0 (0.00) | 7 (11.10) | 0.26 | 0.08 | 0.48 |
| Oral or nasal ulcers | 12 (32.43) | 1 (25.00) | 20 (31.70) | 0.76 | 0.94 | 0.78 |
| Serositis (pleuritis or pericarditis) | 1 (2.70) | 0 (0.00) | 5 (7.90) | 0.74 | 0.28 | 0.56 |
| Raynaud's phenomenon | 4 (10.81) | 2 (50.00) | 21 (33.30) | 0.03 | 0.01 | 0.50 |
| Lupus nephritis | 1 (2.70) | 0 (0.00) | 2 (3.20) | 0.74 | 0.89 | 0.72 |
| Neuropsychiatric clinic | 3 (8.10) | 1 (25.00) | 3 (4.80) | 0.28 | 0.50 | 0.10 |
| Congenital heart block | 0 (0.00) | 0 (0.00) | 0 (0.00) | – | – | – |
| Xerophthalmia | 27 (73.00) | 2 (50.00) | 46 (73.00) | 0.34 | 0.99 | 0.32 |
| Xerostomia | 26 (70.30) | 1 (25.00) | 43 (68.30) | 0.07 | 0.83 | 0.07 |
| Arthralgia without arthritis | 30 (81.10) | 3 (75.00) | 52 (82.50) | 0.77 | 0.87 | 0.70 |
| Fatigue | 16 (43.25) | 1 (25.00) | 33 (52.40) | 0.48 | 0.37 | 0.29 |
| Lymphoma | 0 (0.00) | 0 (0.00) | 4 (6.30) | – | 0.12 | 0.60 |
| Parotidomegaly | 2 (5.40) | 0 (0.00) | 10 (15.90) | 0.63 | 0.12 | 0.39 |
| DILD | 4 (10.80) | 1 (25.00) | 6 (9.50) | 0.41 | 0.83 | 0.32 |
| Peripheral neuropathy | 2 (5.40) | 1 (25.00) | 7 (11.10) | 0.15 | 0.33 | 0.40 |
| Cutaneous purpura | 1 (2.70) | 0 (0.00) | 3 (4.80) | 0.74 | 0.61 | 0.65 |
| Interstitial nephritis | 0 (0.00) | 0 (0.00) | 2 (3.20) | – | 0.27 | 0.72 |
| Clinical APS | 2 (5.40) | 0 (0.00) | 1 (1.60) | 0.63 | 0.28 | 0.80 |
| Other overlaps | 12 (32.40) | 0 (0.00) | 11 (17.50) | 0.17 | 0.08 | 0.36 |
| Overlap typea | 0.82 | 0.15 | 0.93 | |||
| SLICC one year after diagnosis | 0.58±1.07 | 1.50±0.70 | 0.41±0.99 | 0.08 | 0.65 | 0.02 |
| Current SLICC | 1.00±1.44 | 1.50±0.70 | 0.80±1.37 | 0.32 | 0.75 | 0.13 |
DILD: diffuse interstitial lung disease. APS: antiphospholipid syndrome. SLICC: Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus.
Results of the analytical variables according to the expressed anti-Ro antibody profile and differences observed between groups.
| Groups | p value | |||||
|---|---|---|---|---|---|---|
| Variables (n, %) | Group A:Anti-Ro 60+(n=37) | Group B:Anti-Ro 52+(n=4) | Group C:Anti-Ro 52 & 60+(n=63) | Group A vs. group B | Group A vs. group C | Group B vs. group C |
| Hematuria | 20 (58.82) | 1 (33.30) | 22 (37.30) | 0.40 | 0.04 | 0.89 |
| Leukocyturia | 20 (58.82) | 2 (66.70) | 31 (52.50) | 0.80 | 0.56 | 0.63 |
| Proteinuria>0.5g/24h | 3 (12.00) | 0 (0.00) | 4 (9.30) | 0.52 | 0.72 | 0.58 |
| Hemolytic anemia | 1 (2.70) | 0 (0.00) | 2 (3.20) | 0.74 | 0.88 | 0.71 |
| Leukopenia<4000/mm3 | 13 (35.13) | 3 (75.00) | 39 (61.90) | 0.12 | 0.01 | 0.60 |
| Lymphopenia>1500/mm3 | 28 (75.67) | 4 (100.00) | 55 (87.30) | 0.26 | 0.13 | 0.45 |
| Thrombocytopenia<100,000/mm3 | 1 (2.70) | 1 (25.00) | 4 (6.30) | 0.06 | 0.42 | 0.17 |
| Low C3 | 12 (32.43) | 1 (25.00) | 16 (25.40) | 0.76 | 0.45 | 0.97 |
| Low C4 | 4 (10.81) | 0 (0.00) | 7 (11.10) | 0.49 | 0.96 | 0.48 |
| Low CH50 | 3 (8.33) | 1 (25.00) | 6 (9.50) | 0.29 | 0.84 | 0.32 |
| Low complement ever | 12 (32.43) | 2 (50.00) | 21 (33.30) | 0.48 | 0.92 | 0.50 |
| Anti-La | 7 (18.91) | 0 (0.00) | 46 (73.00) | 0.34 | 0.00 | 0.00 |
| Anti-RNP | 3 (8.33) | 1 (33.30) | 8 (12.70) | 0.17 | 0.50 | 0.31 |
| Anti-Sm | 1 (2.77) | 1 (33.30) | 5 (7.90) | 0.02 | 0.30 | 0.13 |
| Anti-dsDNA | 4 (12.50) | 0 (0.00) | 6 (9.80) | 0.51 | 0.69 | 0.57 |
| ANA maximum title | 467.01±382.05 | 2080±2285.25 | 1969.58±1373.07 | 0.17 | 0.00 | 0.64 |
| Rheumatoid factor | 12 (33.30) | 2 (50.00) | 44 (71.00) | 0.50 | 0.00 | 0.37 |
| Polyclonal hypergammaglobulinemia | 6 (18.18) | 0 (0.00) | 24 (42.10) | 0.35 | 0.02 | 0.09 |
| High β2-microglobulin | 7 (29.16) | 1 (33.30) | 23 (43.40) | 0.88 | 0.23 | 0.73 |
| ACL-G | 2 (6.45) | 0 (0.00) | 1 (1.80) | 0.65 | 0.26 | 0.81 |
| ACL-M | 5 (16.12) | 0 (0.00) | 2 (3.60) | 0.45 | 0.04 | 0.73 |
| Anti-β2GPP IgG | 3 (9.67) | 0 (0.00) | 2 (3.60) | 0.57 | 0.25 | 0.73 |
| Anti-β2GPP IgM | 6 (19.35) | 0 (0.00) | 1 (1.80) | 0.40 | 0.00 | 0.81 |
| Lupus anticoagulant | 9 (29.03) | 0 (0.00) | 4 (7.30) | 0.27 | 0.00 | 0.63 |
| Anti-CCP | 5 (16.13) | 0 (0.00) | 8 (15.70) | 0.54 | 0.96 | 0.54 |
| APS antibodies | 10 (31.25) | 0 (0.00) | 5 (9.30) | 0.25 | 0.01 | 0.58 |
ACL-G: anticardiolipin IgG. ACL-M: anticardiolipin IgM. Anti-β2GPPP: anti-β2glycoprotein. Anti-CCP: anti-cyclic citrullinated peptide antibody. APS: antiphospholipid syndrome.
The group with isolated anti-Ro60+ had less Raynaud's phenomenon than the other groups, less need for rituximab than the group with isolated anti-Ro52+, and shorter disease duration than the group with both subunits. Analytically, a lower expression of anti-Sm was observed in comparison to anti-Ro52+ patients. Likewise, they had more hematuria, ACL-M, anti-β2GPP IgM, lupus anticoagulant and APS antibodies than the group with both subunits and less leukopenia, anti-La, maximum ANA titers, rheumatoid factor and polyclonal hypergammaglobulinemia than the latter.
On the other hand, anti-Ro52+ patients showed more Raynaud's phenomenon, use of rituximab and anti-Sm expression than anti-Ro60+ patients. Likewise, they had a higher SLICC at diagnosis and lower anti-La expression than patients with both subunits.
Finally, patients with both subunits had more Raynaud's phenomenon and disease duration than those with isolated anti-Ro60+, and less SLICC one year after diagnosis than the anti-Ro52+ group. Analytically, multiple differences were observed between the anti-Ro52 and 60+ group and the isolated anti-Ro60+ group. Thus, the former showed less hematuria, expression of ACL-M, anti-β2GPP IgM and APS antibodies and more leukopenia, maximum ANA titer, rheumatoid factor and polyclonal hypergammaglobulinemia than the anti-Ro60+ group. The greater expression of anti-La stood out compared to the other two groups.
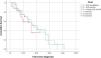
When analyzing difference in survival free of damage (SLICC=0), we did not find any statistical differences between the three groups with SLE, with pairwise comparison with p-values of 0.606 between groups 1 and 2, 0.839 between groups 1 and 3 and 0.742 between groups 2 and 3 (see Fig. 2).
DiscussionTo date, various studies have been published that compare the characteristics between patients with SLE, SS and the overlap of both entities, as well as, according to the serological profile of the anti-Ro antibody expressed. However, there are no studies available to date that compare the characteristics of patients with anti-Ro+ and − SLE.
Despite the associations described in the literature between anti-Ro antibodies and the presence of photosensitivity, subacute cutaneous lupus and neonatal lupus,3 no significant differences were found in our study for these variables between anti-Ro+ and − patients, presumably due to the sample size of the study. The lower use of belimumab in patients with anti-Ro+ SLE compared to those with anti-Ro− responds to the Spanish Agency for Medicines and Health Products’ online drug information center's (CIMA) indication of use in patients with active SLE, positive autoantibodies and a high degree of disease activity (e.g. positive anti-dsDNA and low complement level) despite standard treatment.12,13 Thus, there is a tendency toward a greater use of this drug in the group with anti-dsDNA+ and, therefore, anti-Ro− SLE, according to the selection criteria of our study. Patients with anti-Ro+ SLE had a lower current SLICC, but that could be explained by the shorter duration of the disease in that group. In fact, the survival analysis did not show any differences in the presence of any damage measured by SLICC≥1 at the end of the study between the 3 groups with SLE.
Most of the differences found between patients with SLE/SS and anti-Ro− SLE were expected, as these are symptoms, pathology and analytical data typically associated with SS, and therefore will be more expressed in patients with overlap.14 On the other hand, the intermediate expression of the group with anti-Ro+ SLE compared to patients with anti-Ro− SLE and overlap for the xerophthalmia and xerostomia variables was notable. The above reflects the overlap of sicca syndrome in patients with anti-Ro+ SLE and those with SS observed in clinical practice and referred to at the beginning of the work, which can make it difficult to distinguish between both entities.
In reference to previous studies, a recent meta-analysis14 postulates that SS developed in patients with SLE resembles a low-grade SLE with SS developed at an older age. Thus, patients with SLE/SS may represent a special subgroup of SLE patients characterized by less internal organ involvement, a characteristic serological profile, and a potentially more favorable prognosis. This would include less use of glucocorticoids and immunosuppressive agents, with reduced mortality.14 The above matches the results obtained in the present work, where patients with the overlap showed lower corticosteroid bolus requirements compared to patients with anti-Ro− SLE (2% vs 18.4%, p<0.05), being also interesting the similar behavior already mentioned between the SLE anti-Ro+ group and the overlap group for this variable.
Regarding the results of patients with SLE/SS and SS, the former showed, as expected, more manifestations typically associated with SLE.15 Analytically, we highlight the greater expression of β2-microglobulin in the group with SS compared to the overlap. Given that elevated levels of β2-microglobulin have been significantly related to the risk of lymphoma in patients with SS,16 this could imply a lower tendency toward the development of lymphoma in patients with overlap. On the other hand, the overlap group seemed to show numerically a greater expression of certain autoantibodies, such as anti-Sm or anti-RNP, compared to the SS group, although no statistically significant differences were found. This retention of antibodies in patients with SLE/SS, which does not allow them to be distinguished from patients with SLE without SS, has already been described in other studies.17 No statistically significant differences were found in sicca symptoms and other SS typical symptoms (fatigue and parotid enlargement), matching the reports of a previous study which stated that the clinical presentation of sicca syndrome that occurs in patients with SLE/SS is very similar to that of patients with primary SS.17
Regarding the analysis according to the expressed anti-Ro profile, several studies suggest that patients with isolated anti-Ro52+ more frequently present idiopathic inflammatory myopathy (IIM) and anti-Jo1+,18 as well as higher probabilities of suffering from DILD and PHT compared to the other two groups,6 presumably in a context of IIM-related lung injury.19 Likewise, anti-Ro52 has been independently associated with PHT and mortality in patients with other rheumatological diseases such as systemic sclerosis20 and with pulmonary fibrosis in mixed connective tissue disease.21 However, these results could not be corroborated in the present study, probably due to the small sample size and low prevalence of both DILD and PTH in our cohort.
Other studies have associated the presence of isolated anti-Ro52+ with more Raynaud's phenomenon.6 In our work, 50% of the patients in this group presented it, finding statistically significant differences with the isolated anti-Ro60+ group. This is of interest, since the prevalence of lung involvement has been shown to be significantly higher in patients with SS and Raynaud's phenomenon.22 Furthermore, the anti-Ro52+ group required more rituximab than anti-Ro60+ patients and presented a higher SLICC one year after diagnosis than patients with both subunits. Both the higher requirement for rituximab and the increased SLICC compared to the other groups suggest that, although a higher prevalence of lung disease or mortality have not been demonstrated in anti-Ro52+ patients, patients with positivity for this antibody seem to have greater severity of the disease, as other studies also conclude.23
On the other hand, we consider noteworthy the statistically significant higher prevalence of lupus anticoagulant and antiphospholipid antibodies in the anti-Ro60+ group compared to the group with both subunits. This finding has recently been published in another study, which suggests that patients with isolated anti-Ro60 could have more lupus anticoagulant and anticardiolipin antibodies, an association that has rarely been described or studied to date in other publications.24 The absence of isolated anti-Ro52+ patients with anti-La or antiphospholipid antibodies is also worth mentioning.
Regarding the group of patients with anti-Ro52 and 60+, the higher positivity of anti-La and rheumatoid factor found in this group is consistent with other studies, where they also report a greater tendency in these patients to suffer from xerophthalmia and xerostomia and to be diagnosed with SS.6,25
In reference to the limitations of the study, the small sample size when stratifying the patients in four groups, especially in the group of patients with isolated anti-Ro52+, and the lack of determination of certain analytical parameters in some patients, in line with the nature of a retrospective design of the study, may have limited the results obtained. We also did not include the group of patients anti-dsDNA+, anti-Ro+ in the comparison groups, which could have given us more extensive information. Additional multicenter longitudinal studies should be performed to achieve a better understanding of the significance that the anti-Ro antibody, and its different subunits, provides to SLE patients.
ConclusionsThe presence of anti-Ro+ in patients with SLE provides clinical and analytical differences compared to patients with anti-Ro− SLE and SLE/SS. The group with anti-Ro+ SLE presented more sicca syndrome and overlap with other rheumatological entities, but less arthritis, need for bolus corticosteroids and current SLICC than patients with anti-Ro− SLE, suggesting a possible lower activity and chronic damage in anti-Ro+ patients. Furthermore, this group appears to oscillate between a similar behavior to the overlap group and an intermediate behavior between the latter and the anti-Ro− SLE group for multiple variables. For all these reasons, the groups with anti-Ro+ and overlapping SLE are considered similar entities, but with differential characteristics that postulate them as different and independent phenotypes of the disease. On the other hand, the greater expression of β2-microglobulin in the group with SS compared to the overlap group is of interest, as it could translate into a lower risk of lymphoma in patients with overlap. However, both groups do not show differences in the clinical presentation of sicca syndrome.
Regarding the analysis by the anti-Ro subunit expressed, we must pay attention to patients with an isolated anti-Ro52+ expression, given the possibility of developing a more serious disease. Likewise, the expression of isolated anti-Ro60+ has been associated with a greater positivity for lupus anticoagulant and APS antibodies. For all these reasons, we conclude that the different serological profiles of anti-Ro confer specific clinical and analytical characteristics in patients with SLE and SS, confirming their significance in clinical practice. Knowing these differences is essential to improve the diagnosis, treatment and prognosis of these patients. However, more studies are needed to achieve a better characterization of them.
Ethical considerationsThis project has been approved by the Ethics Committee of Hospital del Mar (project approval code: 2023/11269).
Conflicts of interestThe authors have declared that they have no competing interests.