We present the case of 56-year-old man who came to the emergency department with a 48-h history of fever and pain in left gluteus, radiating to posterior thigh. Three days before the onset of the symptoms, the patient had self-administered a dose of intraurethral alprostadil to treat erectile dysfunction secondary to prostatectomy for adenocarcinoma of the prostate. Physical examination revealed pain in response to pressure on left sacroiliac joint. The responses to the Lasègue test and to pressure applied on left piriformis muscle were positive. Laboratory tests revealed a C-reactive protein level of 251mg/l (normal level, 0–5mg/l) and a procalcitonin level of 1.18ng/ml (<0.25), without leukocytosis or left shift. Abdominopelvic computed tomography (Fig. 1) detected the presence of cortical erosions, predominantly on the lower half of the iliac side of left sacroiliac joint, associated with subchondral sclerosis, all of which is compatible with the radiological diagnosis of left-sided sacroiliitis.
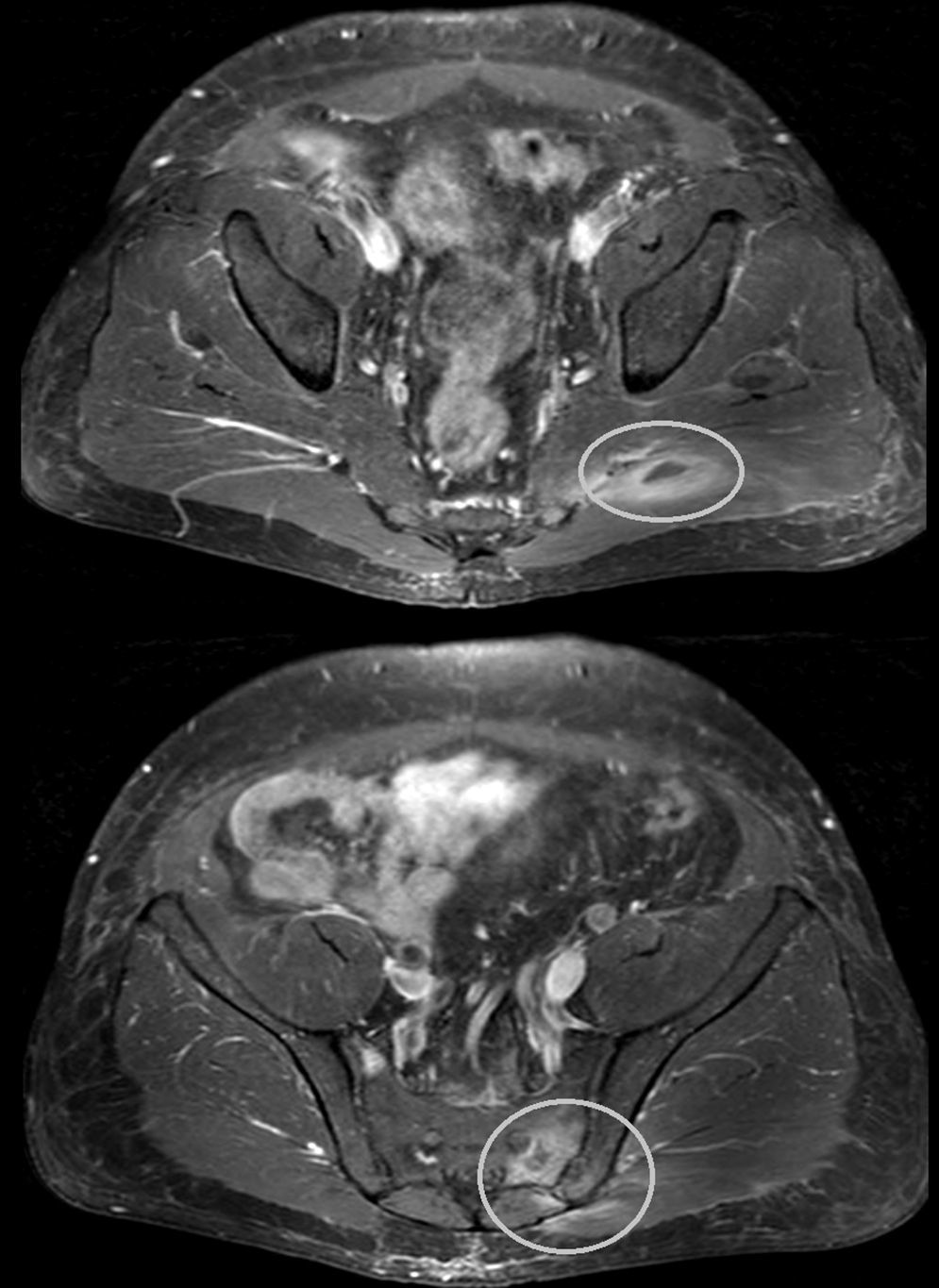
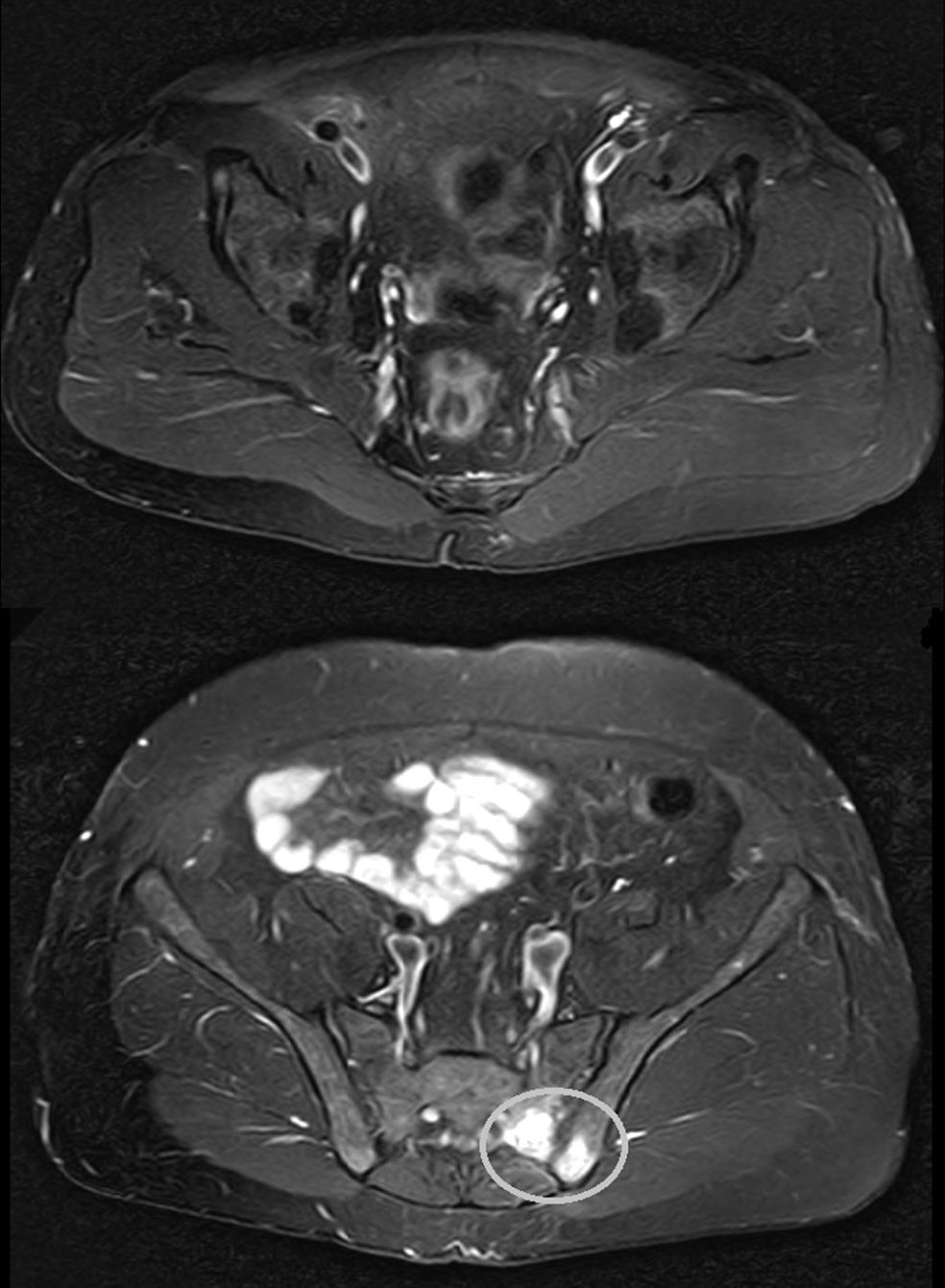
Pelvic magnetic resonance imaging (MRI) (Fig. 2) revealed subchondral bone edema on both the sacral and iliac sides of left sacroiliac joint, as well as subtle signal hyperintensity in the articular interosseous space. In addition, myositis was observed in neighboring muscles, in left rotator muscles, as well as in the gluteus maximus, where the area of myositis was greater and was accompanied by a small central abscess. Thus, empirical antibiotic therapy with ceftriaxone and cloxacillin was begun.
When methicillin-sensitive Staphylococcus aureus was isolated from the blood sample collected in the emergency department, ceftriaxone was discontinued, whereas cloxacillin administration was maintained.
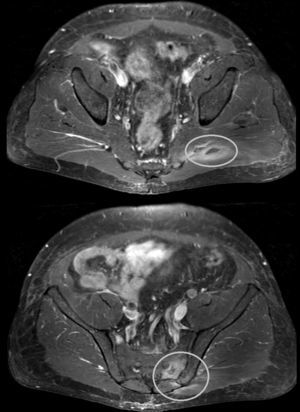
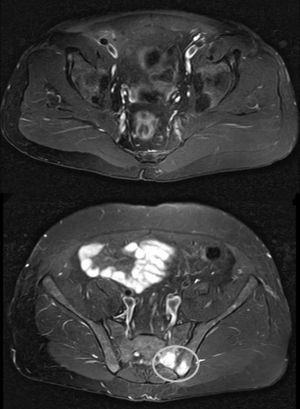
Echocardiography revealed no evidence of endocarditis. One month later, follow-up MRI (Fig. 3) showed that subchondral bone edema persisted on both the sacral and iliac sides of left sacroiliac joint, indicating the persistence of sacroiliitis; in contrast, the area of myositis and the abscess in gluteus maximus had disappeared, a foreseeable finding, given the short time elapsed since the first MRI. The patient continued to improve, both in clinical and analytical terms, with antibiotic therapy, which was maintained for 6 weeks.
DiscussionBoth infectious sacroiliitis and gluteal abscesses are uncommon conditions, representing less than 1% of all the cases of septic arthritis.1,2 The clinical diagnosis is usually difficult, as the classical signs are fever and pain, with functional incapacity of the affected joint.3,4 In this case, as in the majority of the published series, the causative agent was S. aureus.1–10
The risk factors most frequently identified in the cases of this type of joint infection reported in the literature are: intravenous drug use, pregnancy, trauma, endocarditis, hemoglobinopathies, immunosuppression, and skin, respiratory tract or genitourinary infections.5 According to different series, no predisposing agents or risk factors are identified in 40%–44% of the cases.3,5,6 In our patient, intraurethral administration of alprostadil is a plausible candidate as the route of infection responsible for the bacteremia.
Abscess management usually involves drainage by needle aspiration or surgery.8–10 However, there have been reports of complete resolution with antibiotic therapy alone,10 as in the case we present here. To date, there are no established guidelines for the duration of antibiotic therapy, but most authors opt for a minimum of 6 weeks, which can be extended depending on the clinical status of the patient.1,3–5,7–10
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Llop Vilaltella M, Maldonado Romero V, Guillén Astete C, de la Puente Bujidos C, de Casanova Peña C. Sacroilitis y absceso glúteo secundarios a infección por Staphylococcus aureus. Reumatol Clin. 2015;11:398–400.