Streptococcus equi is a Gram-positive, Lancefield group C coccal bacterium that has a close genetic link to Streptococcus zooepidemicus,1 of which it is thought to be a direct ancestor, and is the cause of less than 2% of all the group C streptococcal infections.2 It is a common pathogen in horses, cows and dogs, and can be isolated from the serous discharge of wounds.3,4
Streptococcus equi infection has been documented in humans who are in direct or indirect contact with animals, especially horses, although in most cases, the route of transmission has not been clarified.4
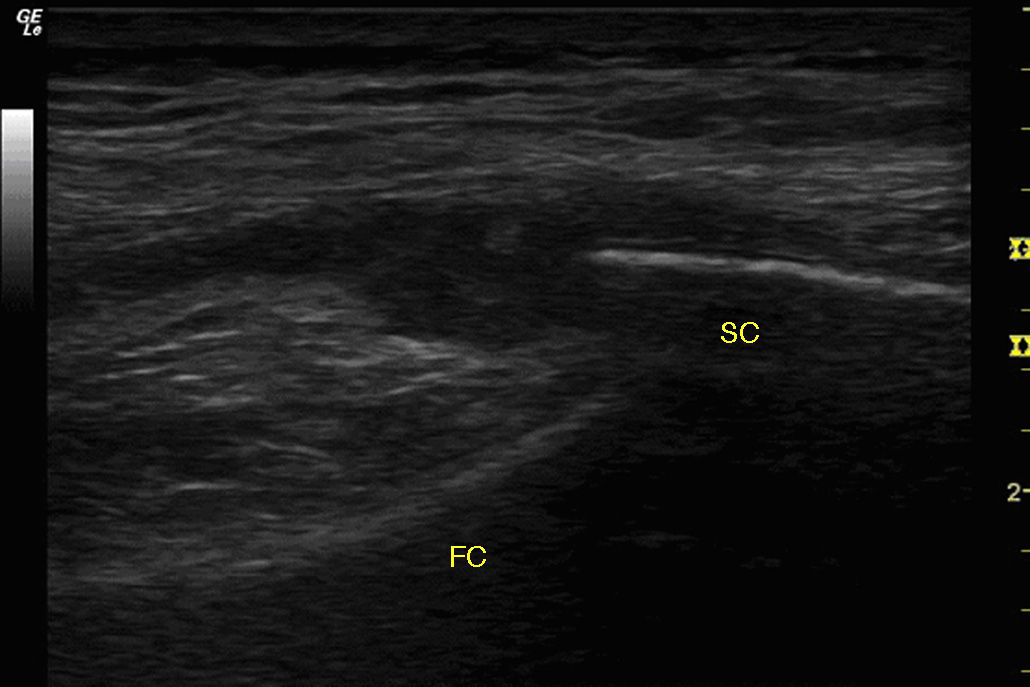
We report a case of septic arthritis caused by Streptococcus equi in a person who may have acquired the infection through a relative who was in contact with horses. The patient was a 72-year-old woman who presented with a 4-day history of pain, swelling and functional limitation in right knee. She had had no injuries. Her granddaughter was a veterinarian at a racetrack. She had a temperature of 38.5°C, increased knee volume, fixed flexion of 30°, erythema and local warmth. There was no evidence of tegmental damage either in or around the knee. Ultrasound showed degenerative changes in the knee, a compressible anechoic area in both suprapatellar recesses associated with a marked proliferation of homogeneous synovial fluid (SF) (Fig. 1) and the power Doppler signal was 1+/3+. In the other knee, only similar degenerative changes were observed.
Arthrocentesis yielded 90mL of synovial fluid with inflammatory features.
The results of laboratory tests included a leukocyte count of 16000/mm3 (90% neutrophils), C-reactive protein level of 210mg/L and procalcitonin level of 1.70ng/mL. In SF, there were no signs of microorganisms, the cell count was 20000cells/mL, and the glucose and protein concentrations were 30mg/dL and 2.3g/dL, respectively.
The patient underwent surgical lavage and was admitted to the hospital, and empirical treatment with ceftriaxone 2g/day and cloxacillin 500mg/6h was begun.
As SF and peripheral blood cultures were positive for Streptococcus equi, treatment was changed to 1,200,000U/day of penicillin G. As the patient's fever and pain persisted, surgical lavage was repeated 10 days after her admission. The outcome was favorable and she was discharged after 5 weeks of intravenous therapy.
Streptococcus equi is a pathogen that causes “strangles”, a lymphoproliferative disease that can affect horses, donkeys and cattle, although subclinical infection has also been documented in dogs.3,5 This disease produces enlargement of the cervical lymph nodes and is associated with upper airway symptoms in animals. The lymphocyte proliferation can produce skin necrosis and neck abscesses. Both the serous discharges from abscesses and saliva of the diseased animal are sources of transmission to other animals or to humans.3,5–7 Infection in humans mediated by the consumption of dairy products from infected animals has also been documented.8,9
Although a number of cases of Streptococcus equi infection have been reported in humans,2,10–13 septic arthritis is a highly uncommon finding.9,11,14–16 Information on the epidemiological burden of this pathogen as the causative agent is not available.
A history involving a connection to horses, as occurred in our patient, has not been demonstrated in most of the case reports.17 However, despite this link, it was not possible to determine the mechanism that produced the infection.
Streptococcus equi infection responds favorably to treatment with penicillins, although cases of drug resistance have been reported and the clinical course is variable.17
Another interesting finding was the marked synovial proliferation, which could hardly be attributed to the similar degenerative changes in both knees.
Streptococcus equi is an uncommon cause of arthritis due to group C streptococci that should be considered in the differential diagnosis of arthritis in a single joint in patients who are in contact with animals, especially horses. The clinical course is variable and, although, theoretically, it is sensitive to beta-lactams, antibiotic resistance has been documented. Our patient also had a marked synovial proliferation and an increased procalcitonin level, but the cellularity in SF was not consistent with joint infection. This protein is a precursor of calcitonin, and has been included as a key test in the diagnosis of inflammatory processes mediated by bacterial agents. Its concentration increases within the first 6h of the production of bacteremia, and its specificity ranges between 91% and 93%, depending on the disease.18 A recent study demonstrated the value of procalcitonin in cases in which the suspicion of septic arthritis overlapped that of gout.19 It was this finding that, despite the low cellularity of the SF, induced us to continue to suspect septic arthritis.
Please cite this article as: Guillén Astete CA, Sánchez Gómez N, Luque Alarcón M. Artritis infecciosa por Streptococcus equi. Reumatol Clin. 2016;12:237–238.