Most patients describe gout attacks as especially painful. Effective treatments – colchicine, NSAIDs, systemic or intra-articular corticosteroids, interleukin-1 blockers – result in an effective resolution of the attacks; however, it usually requires 1–3 days1–4 to relieve the symptoms, and at least a few hours to start lessening them. After an initial observation, intra-articular triamcinolone with added 2% mepivacaine has become a usual procedure in our clinics, as we have repeatedly observed a very rapid and persistent subsidence of pain. Here we aimed to prospectively document this outcome.
Consecutive patients with crystal-proven gout, suffering from an acute, monoarticular and still untreated flare were recruited. All cases were treated with an intra-articular injection of triamcinolone acetonide (16mg in knees, 8mg in 1st metatarso-phalangeal (1stMTP) joint and 12mg in intermediate sized joints) adding 2ml of 2% mepivacaine in knees, 1–1.5ml in intermediate sized joints, and 0.2–0.4ml in 1stMTP joints, in accordance to our usual clinical practice.5 Joint pain was registered using a 0–4 Likert semiquantitative scale (0=absent; 4=severe) at baseline and 15min, 6h, 24h, and 72h after the injection. Presence of joint swelling and erythema were also collected at baseline and after 72h. Treatment response after 72h was evaluated by both the physician and the patient on a 0–4 Likert scale (0=no effect; 4=complete resolution). Between-after comparisons were analysed using Friedman and Wilcoxon signed-rank tests.
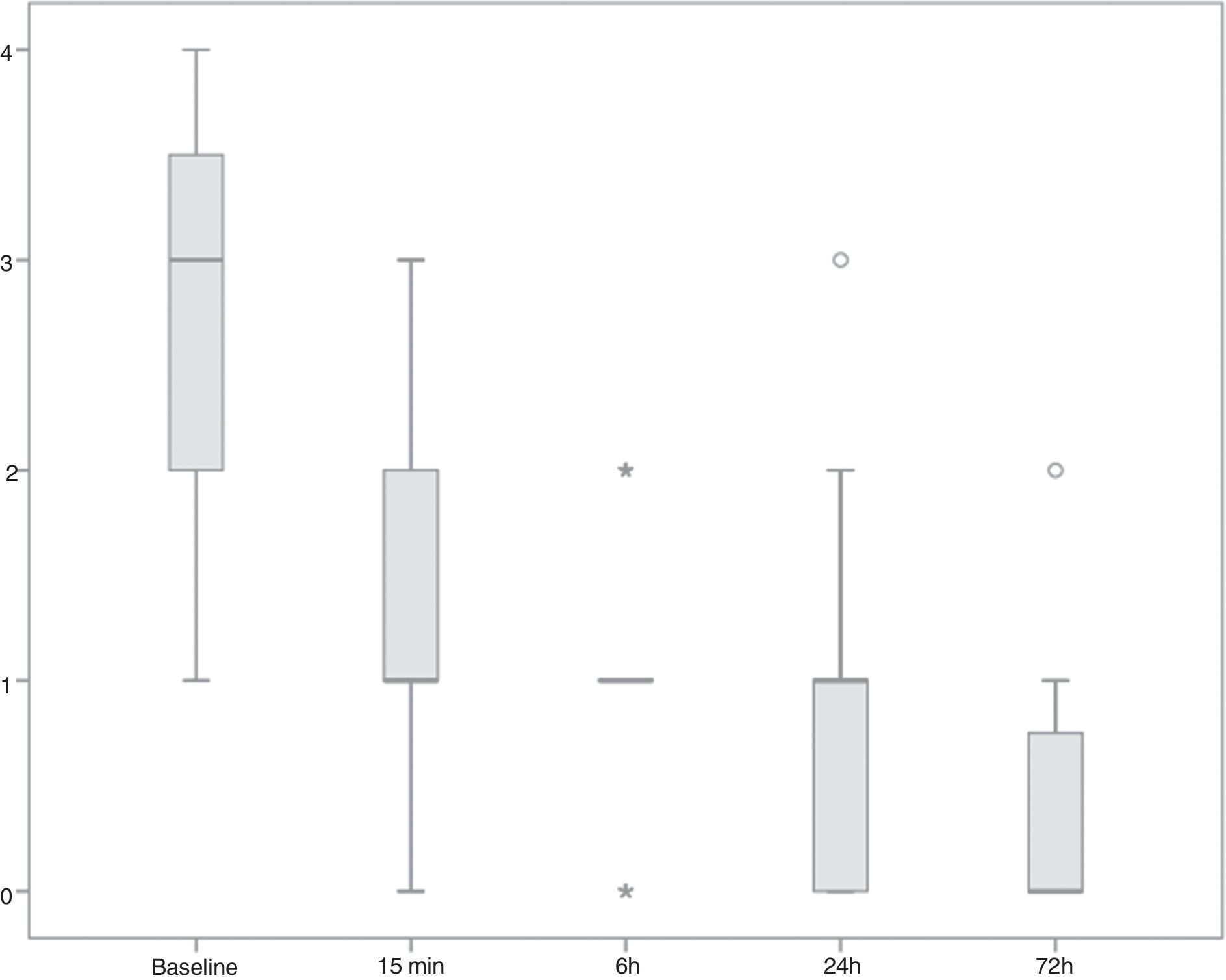
Twenty-four patients were recruited; median (±SD) aged 64.8 years (±12.7), 22 males. Involved joints were sixteen 1stMTPs, five knees, two wrists, and one ankle. Median (p25–75) pain score at baseline was 3 (2.0–3.8), joint swelling was present in all cases, and in 13 cases (54.2%) erythema was observed. After a few minutes of the intra-articular injection, a rapid pain reduction was observed and maintained up to 72h, the end of the registrations, as patients reported it (Fig. 1). In only three cases (12.5%), all with 1stMTP attacks, the pain intensity rebounded between 15min and 6h after the injection. Treatment was clearly effective as assessed by both patients and rheumatologists (3 (3–4) and 3.5 (3–4), respectively).
This small study supports our observation from clinical practice: adding mepivacaine to a low dose of intra-articular triamcinolone acetonide leads to an almost immediate relief of gout attacks, with a clear response even 15min after the injection and maintenance of a symptom – free to tolerable pain until subsidence of the symptoms.
The almost immediate pain relief can be attributed to mepivacaine. There are few data on the duration of anaesthesia with this agent, but when used for brachial plexus blockade, it lasts between 3 and 4h.6 Interestingly, dexamethasone added to mepivacaine in brachial plexus anaesthesia prolonged the time of anaesthesia from a mean of 228min up to 332min, a highly significant change.7 A similar effect may occur when triamcinolone and mepivacaine are conjointly injected in a joint affected by a gout flare. An early effect of triamcinolone on the synovial irrigation could reduce the local inflammation-related blood flow, retarding mepivacaine clearance from the joint. The pain reappeared in a number of patients after its initial marked reduction, but with a moderate intensity, likely indicating that by that time, the steroid action has already begin; afterwards the flare totally subsided, although the total time to subsidence in some patients maybe as long as it would be if only steroids would have been injected. These results were highly welcomed both by physicians and especially by patients.
FundingThis study had no external funding source
Conflict of interestMA has received speaking and advisory fees from Menarini, Grünenthal and Horizon. FS has received speaking and advisory fees from Menarini, Grünenthal and Horizon. The rest of authors declare no conflicts of interest in relation to this work.