To describe the demographic and clinical features, as well as the frequency of the HLA-B*51 allele in Behçet disease (BD) patients in Latin American countries.
MethodsA systematic literature review of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines was conducted without performing a meta-analysis. We included observational studies (cross-sectional or cohort) of BD patients fulfilling the International Study Group for BD classification criteria and reported the demographic, clinical, and laboratory features of the disease in adult patients.
ResultsTwelve studies were included in the SLR. Information from 532 patients across 5 Latin American countries was included for the analysis. Mean age at disease diagnosis was 33 years, 58.3% were female and 41.7% male; most patients were non-Caucasian. The most common clinical manifestations were recurrent oral ulcers and genital ulcers, followed by skin, eye, joint, neurological, gastrointestinal, vascular, and cardiac involvement. The prevalence of BD was described in 2 studies, 1 conducted in Brazil that reported a prevalence of .3/100,000 inhabitants, and another in Colombia with a prevalence of 1.1/100,000 inhabitants. The frequency of HLA-B*51 allele in BD patients was 38%, 30.1%, and 9% in Argentina, Brazil, and Mexico, respectively.
ConclusionsThe prevalence of BD in the Latin American countries seems to be low, as well as the frequency of HLA-B*51 allele. However, the strength of association between HLA-B*51 and BD remains high in our population. The key clinical features of BD are like those reported in countries/regions where BD is endemic.
Describir las características demográficas, clínicas y la frecuencia del alelo HLA-B*51 en pacientes con enfermedad de Behçet (EB) en países de América Latina.
MétodosSe llevó a cabo una revisión sistemática de la literatura (RSL) según la guía PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) sin realizar un metaanálisis final. Se incluyeron estudios observacionales (transversales o de cohortes) de pacientes con EB que cumplieron con los criterios de clasificación del Grupo Internacional de Estudio de la EB e informaron las características demográficas, clínicas y de laboratorio en pacientes adultos con EB.
ResultadosDoce estudios fueron incluidos para la RSL. La información de 532 pacientes provenientes de 5 países de América Latina se incluyó para el análisis. La edad media al diagnóstico fue de 33 años, el 58,3% fueron mujeres y el 41,7% hombres; la mayoría de los pacientes fueron no caucásicos. Las manifestaciones clínicas más comunes fueron las úlceras orales y genitales recurrentes, seguidas del compromiso cutáneo, ocular, articular, neurológico, gastrointestinal, vascular y cardíaco. La prevalencia de la EB fue descrita en 2 estudios, uno realizado en Brasil que reportó una prevalencia de 0,3/100.000 habitantes, y otro en Colombia con una prevalencia de 1,1/100.000 habitantes. La frecuencia del HLA-B*51 en pacientes con EB fue del 38%, 30,1% y 9% en Argentina, Brasil y México, respectivamente.
ConclusionesLa prevalencia de la EB en los países latinoamericanos parece ser baja, así como la frecuencia del alelo HLA-B*51. Sin embargo, la fuerza de asociación entre el HLA-B*51 y la EB sigue siendo alta en nuestra población. Las características clínicas claves de la EB son similares a las reportadas en países/regiones donde es endémica.
Behçet disease (BD) is classified as an inflammatory vascular condition, affecting all kind and size of vessels.1 Although BD is distributed worldwide, its demographic and clinical features are strongly associated with the ethnic group and the geographic area involved.2
The highest prevalence of BD was observed in Asia, especially in Turkey, Israel, Iran, and Japan (prevalence range: 13–420/100,000 inhabitants). In Southern and Western European countries (Italy, Spain, and France) the prevalence rate was intermediate (prevalence range: 1.5–16/100,000 inhabitants), while Northern European countries (Sweden, England, and Scotland) and the United States reported the lowest prevalence (prevalence range: 0.3–5.2/100,000 inhabitants).3
BD usually begins in the third or fourth decade of life, with onset in childhood or late adulthood being rare. The female/male ratio varies among different ethnic groups and geographic regions, with male predominance in Middle Eastern countries and female predominance in European and North American countries. Most series agree that male gender has a more severe disease, regardless of demographic characteristics.2
The disease has a broad spectrum of clinical features and is characterized by periods of exacerbation and remission. Its phenotypic expression also varies according to the ethnic group and country. Skin and mucosal lesions comprising oral and genital ulcers, papulopustular lesions, and erythema nodosum-like lesions are observed in most patients. On the other hand, uveitis, venous thrombosis, arterial thrombosis and aneurysms, nervous system and gastrointestinal involvement occur in a smaller number of patients.4
The genetic predisposition for BD is suggested by the higher concordance for BD in monozygotic twins compared to dizygotic twins.5 The genetic approach identified associations between different genetic markers and BD, with HLA-B*51 allele being the strongest susceptibility factor for the disease. It is estimated that carriers of HLA-B*5/B*51 have a pooled odds ratio of 5.78 for the development of BD (95% confidence interval: 5–6.7) compared with non-carriers. Moreover, the population-attributable risk for BD concerning the presence of HLA-B*5/B*51 within different geographic areas was estimated at 32–52%.6
Limited data exist on the demographic, clinical features and the HLA-B*51 frequency of BD in Latin American countries. This region is characterized by being multi-ethnic (White, Mestizo, African Latin Americans and Pure Amerindians) and multicultural. Data from the GLADEL (Grupo Latino Americano De Estudio de Lupus) cohort demonstrated that patients with mestizo systemic lupus erythematosus have significant differences (demographic and clinical characteristics) compared to white patients. Indeed, these differences are associated with a worsening overall prognosis for mestizo SLE patients.7 It is therefore necessary to better describe the demographic and clinical characteristics of BD patients in Latin America countries that may be unique to this population.
The aim of this work was to describe through a systematic literature review (SLR) the demographic and clinical features, as well as the frequency of HLA-B*51 allele in BD patients in Latin America countries.
Materials and methodsAn SLR was carried out according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines without performing a meta-analysis.8
Search strategyWe searched PubMed database from inception until December 30, 2021. We used all possible keywords combinations with Boolean operators and the subsequent search strategy: “Behçet Disease”, “Argentina”, “Bolivia”, “Brazil”, “Chile”, “Colombia”, “Ecuador”, “Mexico”, “Paraguay”, “Peru”, “Uruguay”, “Venezuela”, “Caribbean” and “Latin America”. The search was restricted to the Spanish and English languages. In order to improve this work, a hand search was performed in the reference lists of the selected full-text articles to find additional references that could be relevant for this review. Two investigators (S.A.M. & A.O.O.) carried out this review, analyzed each selected article, and collected the data independently. In case of disagreement, a third investigator was consulted (A.A.). Any discrepancies were resolved through a consensus discussion.
We included observational studies (either cross-sectional or cohort) of BD patients fulfilling the International Study Group for Behçet Disease classification criteria and reported the demographic, clinical and laboratory features of the disease in adult patients (≥18 years).9 A minimum sample size was not an inclusion/exclusion criterion for an article. Studies published only as abstracts or presented at professional meetings were not included.
Data collectionTwo investigators reviewed the data from the selected articles using a predetermined collection form. Information about the study characteristics (design, country, sample size), number of participants, gender, ethnicity, age at diagnosis, clinical and laboratory features was gathered.
The studies selected were summarized using a narrative synthesis approach. Summary tables and structured narrative were used to descriptively summarize and compare each of the studies herein included.
Ethical aspectsThe research methods were in conformity with the principles of the Helsinki Declarations.
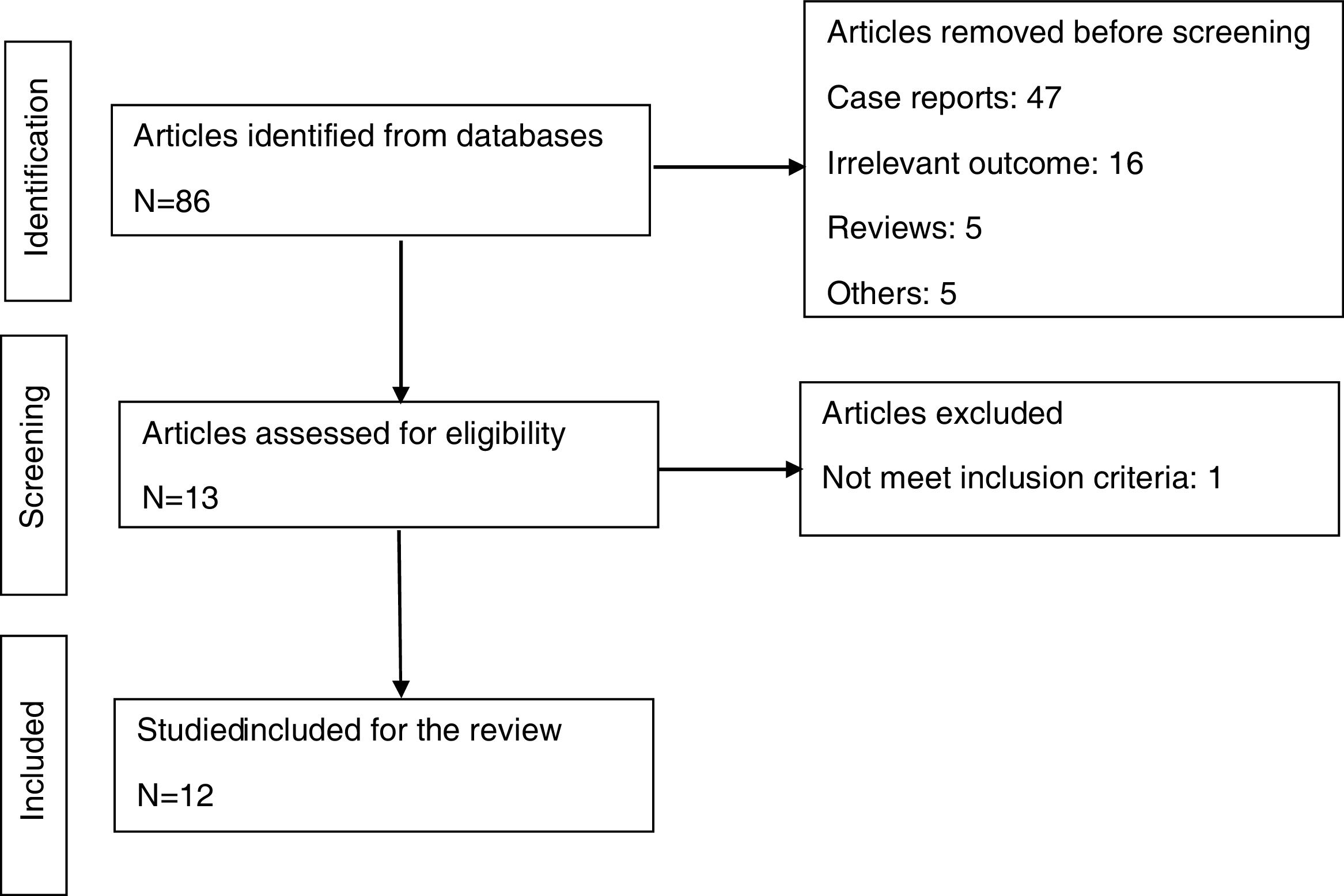
ResultsThe literature search yielded 86 articles, as shown in Fig. 1. A total of 74 articles were excluded for several reasons, and 12 were considered for analysis in this SLR.3,10–20 Seven articles were from Brazil, two from Colombia and one from each of the following countries: Argentina, Chile, and Mexico. Ten articles refer to the demographic and clinical findings of BD patients (Table 1). Two articles deal with the prevalence of BD,19,20 and three articles with the frequency of HLA-B*51 in BD patients10,17,18 and are discussed separately in the corresponding section.
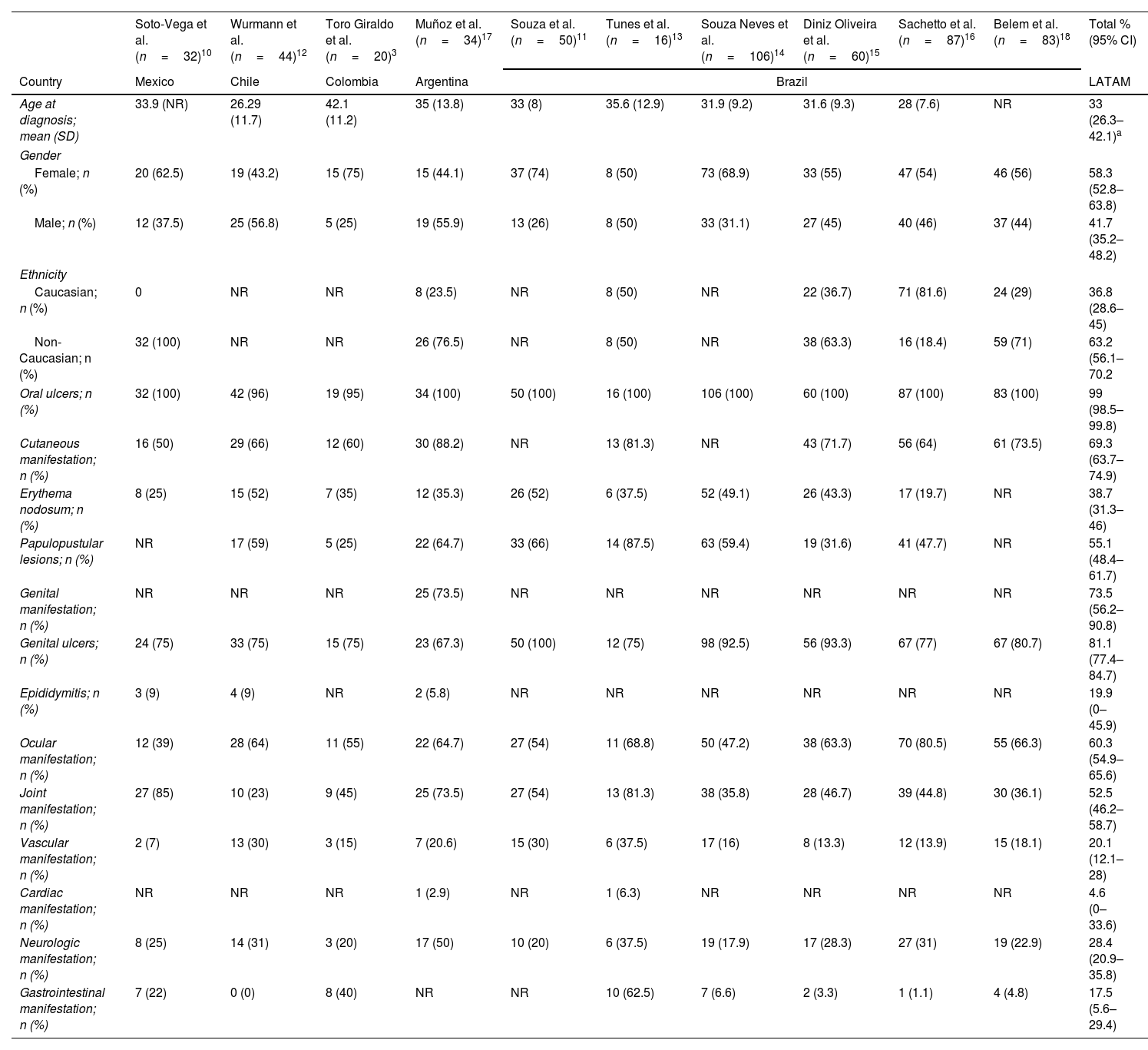
Demographic and key clinical features of the Latin American Behcet studies.
| Soto-Vega et al. (n=32)10 | Wurmann et al. (n=44)12 | Toro Giraldo et al. (n=20)3 | Muñoz et al. (n=34)17 | Souza et al. (n=50)11 | Tunes et al. (n=16)13 | Souza Neves et al. (n=106)14 | Diniz Oliveira et al. (n=60)15 | Sachetto et al. (n=87)16 | Belem et al. (n=83)18 | Total % (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Mexico | Chile | Colombia | Argentina | Brazil | LATAM | |||||
| Age at diagnosis; mean (SD) | 33.9 (NR) | 26.29 (11.7) | 42.1 (11.2) | 35 (13.8) | 33 (8) | 35.6 (12.9) | 31.9 (9.2) | 31.6 (9.3) | 28 (7.6) | NR | 33 (26.3–42.1)a |
| Gender | |||||||||||
| Female; n (%) | 20 (62.5) | 19 (43.2) | 15 (75) | 15 (44.1) | 37 (74) | 8 (50) | 73 (68.9) | 33 (55) | 47 (54) | 46 (56) | 58.3 (52.8–63.8) |
| Male; n (%) | 12 (37.5) | 25 (56.8) | 5 (25) | 19 (55.9) | 13 (26) | 8 (50) | 33 (31.1) | 27 (45) | 40 (46) | 37 (44) | 41.7 (35.2–48.2) |
| Ethnicity | |||||||||||
| Caucasian; n (%) | 0 | NR | NR | 8 (23.5) | NR | 8 (50) | NR | 22 (36.7) | 71 (81.6) | 24 (29) | 36.8 (28.6–45) |
| Non-Caucasian; n (%) | 32 (100) | NR | NR | 26 (76.5) | NR | 8 (50) | NR | 38 (63.3) | 16 (18.4) | 59 (71) | 63.2 (56.1–70.2 |
| Oral ulcers; n (%) | 32 (100) | 42 (96) | 19 (95) | 34 (100) | 50 (100) | 16 (100) | 106 (100) | 60 (100) | 87 (100) | 83 (100) | 99 (98.5–99.8) |
| Cutaneous manifestation; n (%) | 16 (50) | 29 (66) | 12 (60) | 30 (88.2) | NR | 13 (81.3) | NR | 43 (71.7) | 56 (64) | 61 (73.5) | 69.3 (63.7–74.9) |
| Erythema nodosum; n (%) | 8 (25) | 15 (52) | 7 (35) | 12 (35.3) | 26 (52) | 6 (37.5) | 52 (49.1) | 26 (43.3) | 17 (19.7) | NR | 38.7 (31.3–46) |
| Papulopustular lesions; n (%) | NR | 17 (59) | 5 (25) | 22 (64.7) | 33 (66) | 14 (87.5) | 63 (59.4) | 19 (31.6) | 41 (47.7) | NR | 55.1 (48.4–61.7) |
| Genital manifestation; n (%) | NR | NR | NR | 25 (73.5) | NR | NR | NR | NR | NR | NR | 73.5 (56.2–90.8) |
| Genital ulcers; n (%) | 24 (75) | 33 (75) | 15 (75) | 23 (67.3) | 50 (100) | 12 (75) | 98 (92.5) | 56 (93.3) | 67 (77) | 67 (80.7) | 81.1 (77.4–84.7) |
| Epididymitis; n (%) | 3 (9) | 4 (9) | NR | 2 (5.8) | NR | NR | NR | NR | NR | NR | 19.9 (0–45.9) |
| Ocular manifestation; n (%) | 12 (39) | 28 (64) | 11 (55) | 22 (64.7) | 27 (54) | 11 (68.8) | 50 (47.2) | 38 (63.3) | 70 (80.5) | 55 (66.3) | 60.3 (54.9–65.6) |
| Joint manifestation; n (%) | 27 (85) | 10 (23) | 9 (45) | 25 (73.5) | 27 (54) | 13 (81.3) | 38 (35.8) | 28 (46.7) | 39 (44.8) | 30 (36.1) | 52.5 (46.2–58.7) |
| Vascular manifestation; n (%) | 2 (7) | 13 (30) | 3 (15) | 7 (20.6) | 15 (30) | 6 (37.5) | 17 (16) | 8 (13.3) | 12 (13.9) | 15 (18.1) | 20.1 (12.1–28) |
| Cardiac manifestation; n (%) | NR | NR | NR | 1 (2.9) | NR | 1 (6.3) | NR | NR | NR | NR | 4.6 (0–33.6) |
| Neurologic manifestation; n (%) | 8 (25) | 14 (31) | 3 (20) | 17 (50) | 10 (20) | 6 (37.5) | 19 (17.9) | 17 (28.3) | 27 (31) | 19 (22.9) | 28.4 (20.9–35.8) |
| Gastrointestinal manifestation; n (%) | 7 (22) | 0 (0) | 8 (40) | NR | NR | 10 (62.5) | 7 (6.6) | 2 (3.3) | 1 (1.1) | 4 (4.8) | 17.5 (5.6–29.4) |
95% CI: confidence interval 95%; NR: not reported; LATAM: Latin American; SD: standard deviation.
Information from 532 patients across 5 Latin American countries was included for the analysis. Mean age at disease diagnosis was 33 years (min–max age: 26.3–42.1 years); 313 (58.3%) were female and 219 (41.7%) male (female-to-male ratio: 1.4:1), and most patients were non-Caucasian (Table 1).
The most common clinical manifestations were recurrent oral ulcers (99%) and genital ulcers (81.1%), followed by skin (69.3%), eye (60.3%), joint (52.5%), neurological (28.4%), vascular (20.1%), gastrointestinal (17.5%), and cardiac (4.6%) involvement. Frequencies and their 95% confidence intervals for clinical findings are shown in Table 1.
BD prevalence in Latin American countriesThe prevalence of BD was described in 2 studies. Tunes et al. from Brazil reported a prevalence of 0.3/100,000 inhabitants in Bahia State (Northeast of Brazil), and more recently, Fernández Avila et al. from Colombia reported a prevalence of 1.1/100,000 inhabitants.19,20
Frequency of HLA-B*51 allele in BD patients from Latin American countriesThe frequency of HLA-B*51 allele in BD patients and controls was described in three different countries, Mexico, Argentina, and Brazil.10,17,18 The frequency of HLA-B*51 was higher in BD patients compared to healthy controls in the Argentine (38% vs. 14.1%; p=0.0012) and Brazilian (30.1% vs. 15.5%; p=0.003) studies, while no difference was observed in the frequency of HLA-B*51 in the Mexican (9% vs. 5%; p=0.24) study. Non-Caucasian ethnicity predominated in all series.15,16 In the Argentine study, Mestizo (20/34, 58.8%) population accounted for most ethnicity, followed by Caucasian (8/34, 23.5%) and Amerindian (6/34, 17.7%) subjects.17 Belem et al. from Brazil reported that 71% of BD patients were non-Caucasian, and most of them (65.1%) were born in the Southeast region.18 In the study carried out by Soto Vega et al. all BD patients were Mexican Mestizos.10
DiscussionLatin America is an ethnic-geographical concept that emerged in the 19th century to identify a region of the American continent where most languages are derived from Latin (mainly Spanish or Portuguese and, to a lesser extent, French). The concept was introduced to differentiate between regions of the continent with Latin, Catholic and mestizo influence, and those characterized by the Anglo-Saxon, Protestant culture, with little or no miscegenation. However, Latin America is a vast region with heterogeneous geographic, ethnic, socioeconomic, and cultural characteristics.21 This fact could modify features of BD, such as its prevalence, genetics, clinical findings, and prognosis.
Through a systematic literature review, we described the demographic, clinical features, and HLA-B*51 allele frequency of BD in Latin American countries.
Data on the prevalence of BD in Latin American countries is scarce, with only 2 studies reported on this topic.19,20 In 2008 Tunes et al. from Brazil reported a prevalence of 0.3/100,000 inhabitants in Bahia State (Northeast Brazil), with a total population of 385,109. The study objective was to evaluate the prevalence of BS in patients with recurrent aphthous ulceration (RAU) followed up in a specialized ambulatory clinic from a university institution. Furthermore, cases of BS with less symptomatic oral aphthae, and hence not meeting the RAU criteria are not included in this study. Therefore, the authors stated that the prevalence of BD in the population could be underestimated due to the “excluded third party” bias.19 More recently, Fernández Avila et al. from Colombia reported a prevalence of 1.1/100,000 inhabitants. Their study was designed to establish the prevalence of BD in Colombia based on the administrative clinical records from the Ministry of Health.20 These studies showed a low prevalence of BD in our region, similar to that in North America (0.3–5.2/100,000) or Northern European countries (prevalence range 02–4.9/100,000).3
BD demographic and clinical features differ worldwide.2 In this SLR, the mean age at disease onset was 33 years (range 26.3–42.1), which is in agreement with previous reports of disease onset in the third/fourth decade.22 The female-to-male ratio was 1.4:1; this slight female gender predominance is consistent with the results described in North America and Western European countries.23 The frequency of major clinical manifestations suggests that BD pattern in Latin America is similar to that described in other regions where this condition is endemic. In order of frequency, oral and genital ulcers, skin, eye, and joint involvement were the most commonly observed manifestations. Similar results were shown in large series of BD patients from endemic areas. Gastrointestinal (GI) involvement is an uncommon manifestation in BD, except in Japan, where the reported prevalence is higher than in the rest of the countries/regions worldwide.24 Interestingly, in this SRL, the frequency of GI manifestation (17.5%) was even higher than that reported in Japan (14%). Soto-Vega et al. reported that 7 of 32 (22%) BD patients had GI lesions; however, the study failed to outline the type of lesions they presented. Toro Giraldo et al. reported a high frequency of GI involvement (8/20; 40%). The type and frequency of manifestation were abdominal pain (25%), mucosal ulcerative lesion (25%), lower GI bleeding (20%), recurrent diarrhea (15%), and intestinal perforation (5%).3 Tunes et al. reported a very high frequency of GI manifestation (10/16; 65.2%); however, except for gastroduodenitis (18.8%), no other manifestation was mentioned in their cohort.13
HLA-B*51 allele is known to be an important susceptibility gene in BD, regardless of geographical region and ethnicity, with a close correlation between the geographical distribution of HLA-B*51 and prevalence of BD. De Menthon et al. in a systematic literature review and meta-analysis observed that the pooled prevalence of HLA-B*51/B*5 allele was 57.2% (95% CI 53.4–60.9) and 18.1 (95% CI 16.1–20.3) for BD patients and healthy controls, respectively. The OR of HLA-B*51/B*5 allele carriers to develop BD compared with non-carriers was 5.78 (95% CI 5.00–6.67). The subgroup analyses stratifying studies by geographic locations showed the highest prevalence of HLA-B*51/B*5 allele in BD patients from Eastern Asia, Middle East/North Africa, and Southern Europe (prevalence range 55–63.5%).6 The OR range (5.18–7.20) for these regions was consistent with the overall OR. Although the prevalence of HLA-B*51/B*5 allele in BD patients (39%) was lower in the Northern/Eastern Europe region, the OR (5.31; 95% CI 3.35–8.40) continues to be consistent with the overall OR. On the other hand, in the North America region, the prevalence of HLA-B*51/B*5 allele (34.2%) was even lower than that in Northern/Eastern Europe and the OR (2.35; 95% CI 0.56–9.82) showed no association with BD presence. The Latin American region was underestimated in this meta-analysis due to the lack of scientific studies evaluating the prevalence of HLA-B*51 in BD patients. In fact, only one Latin American study carried out in Mexico had been included. Lavalle et al. in a small study (10 BD patients and 105 healthy controls) found that HLA-B*5 (HLA-B*51 is a split product of HLA-B*5) allele was more frequent in Mexican Mestizo patients with BD than in ethnically matched controls (70% vs. 31%, p<0.05).25 More recently, 3 Latin American studies reported the prevalence of HLA-B*51 allele in patients with BD and in healthy controls. Soto Vega et al. found no difference in the prevalence of HLA-B*51 allele between Mexican Mestizo BD patients and healthy controls (9% vs. 5%; OR 1.88, 95% CI 0.58–5.93). On the other hand, studies from Brazil and Argentina revealed a prevalence of HLA-B*51 in BD patients of 30.1% and 38%, respectively; these results are similar to those reported in the Northern/Eastern Europe region.3,10,17,18 Both Brazilian and Argentine studies demonstrated an association between HLA-B*51 allele and BD presence (OR=2.34, 95% CI 1.32–4.14 and OR=3.75, 95% CI 1.71–8.19, respectively).17,18 It is noteworthy that the difference between Soto Vega study and Brazil and Argentina studies could be ethnic. While the Mexican study included all mestizo patients, Brazilian and Argentinean studies were comprised of mestizos and other ethnicities (mainly Caucasian and Amerindian).10,17,18
Study limitationsThe data shown and summarized in this systematic review of the literature have a bias because most of the cohorts come from Brazil, which differs from Mexico, Argentina, Colombia, and Chile in terms of ethnicity, sociocultural and economic features, and health access.
ConclusionsThe prevalence of BD in the Latin American region, as well as the prevalence of HLA-B*51 allele, seems to be low; however, the strength of association between HLA-B*51 and BD remains high in our population. The key clinical features of BD are similar to those in countries/regions where BD is endemic. Finally, more studies of the prevalence, demographic and clinical features of BD in Latin American countries are required to confirm these findings.
Conflict of interestsThe authors declare they have no conflict of interest.
The authors greatly appreciate the help of Valeria Melia for the English revision of the manuscript.