Bursae are small, jelly-like sacs that are located throughout the body, mainly around the shoulder, elbow, hip, knee, and heel in a number over 150. They contain a small amount of fluid, and are positioned between bones and soft tissues, acting as cushions to help reduce friction. Pes anserinus bursae, despite being clinically frequent, are not visible either by ultrasound (US) or magnetic resonance image (MRI). In some cases, we may observe a small fluid collection. The present case-report demonstrates the full clinical picture of a giant pes anserinus bursae beginning from clinical observation to its final pathology exam.
Las bursas son estructuras saculares gelatinosas distribuidas por todo el cuerpo; hombro, codo, cuerpo, cadera, rodilla y tobillo. Existen más de 150 y son fisiológicas. Contienen fluido y su función es protectora, evitando la fricción entre estructuras como huesos, tendones y ligamentos. La bursa anserina, a pesar de ser clínicamente frecuente, normalmente no es visible, ni mediante ecografía, ni mediante resonancia magnética. En algunos casos puede tener una pequeña colección líquida. El presente caso muestra toda la evolución de una bursa anserina gigante desde el inicio de la observación clínica, hasta su análisis anatomopatológico.
An 85-year old patient followed in our rheumatology clinic since 2010 with a past medical history of glaucoma, hypertension, and moderate to severe osteoarthritis presented with enlargement of the medial aspect with a large soft tissue mass with pain, and progressive impairment of the knee.
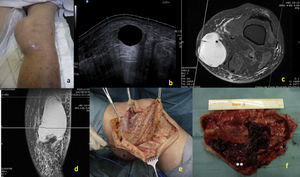
Clinical observationA gray scale ultrasound (US) showed a large anechoic mass over 16 x 11cm (area>15.6cm2) without synovial hypertrophy nor Power Doppler signal (Fig. 1a, b). A subsequent magnetic resonance image (MRI) confirmed in T1 (Fig. 1c, d), a 14cm mass observed in the coronal and axis views. Laboratory and immunology studies showed no important abnormalities related to the present case.
(a) Clinical aspect of the soft tissue mass in the medial knee, (b) gray scale ultrasound showing a 16cm long well defined anechoic mass (area: >15.6cm2) without synovial hypertrophy in the pes anserinus bursa, (c) MRI with axial T1 view showed a homogeneous soft tissue mass at the enthesis of pes anserinus conjoint tendon with peripheral enhancement (*). Absence of hemosiderin deposits and no evidence of bone or joint involvement, (d) T1 coronal view of the bursa, (e) Intraoperative image of the lesion showed multiple yellow to brown nodules inside the pes anserinus bursa, (f) 15cm large bursa excision pathology confirmed the pathology (**).
The patient followed ice local therapy, nonsteroidal anti-inflammatory drugs, repeated US guided aspiration with posterior injection of local steroids and physical therapy. To avoid progressive local compression, excision surgery was then decided. A large saccular mass of 17×11×3cm with peripheral adipose tissue with clots drawing an inflammatory cystic cavity due to a giant pes anserinus bursitis (Fig. 1e, f).
DiscussionBursae are small, jelly-like sacs that are located throughout the body, mainly around the shoulder, elbow, hip, knee, and heel in a number over 150. They contain a small amount of fluid, and are positioned between bones and soft tissues, acting as cushions to help reduce friction. Pes anserine bursitis is an inflammation of the bursa located between the tibia and three tendons of the hamstring muscle (sartorius, gracilis, and semitendinosus), which lie superficial to the tibial insertion below the medial collateral ligament (MCL). Bursitis results from stress of continuous friction to this area, when tight hamstring muscles, obesity, knee osteoarthritis, and meniscal lesions, and presents with pain, tenderness, and local swelling. Rennie & Saifuddin after analyzing 488 knee MRI, confirmed the presence of a pes anserinus bursitis only in a 2.5%.1
Several groups have demonstrated by MRI the characteristics of distal superficial medial collateral ligament (sMCL) tears to identify features of those tears superficial to the pes anserinus (Stener-like lesion (SLL)). This lesion, defined as a distal tear with interposition of osseous or soft-tissue structures between the ligament and its tibial attachment, often requires surgical intervention. Interestingly, distal sMCL tears have a frequent association with concomitant knee injuries, especially ACL tears and lateral femorotibial osseous injuries.2 Alaia et al. reviewed 65 knee MRI examinations where identified 20 cases of distal tibial grade 3 sMCL tear.3 Beside the pathological pattern, some authors consider the major cause for a pes anserinus bursitis is an aberrant structural framework and differences in the constitution of the tendons of the full enthesis.4 Together with this structural disorganization and the tears of the sMCL, other space-occupying lesions within the medial knee include, lipoma, tuberculosis, giant cell tumor, hemangioma, liposarcoma, and myelolipoma.5
ConclusionsThe present case shows an uncommon and extreme presentation of a giant pes anserinus bursitis. US is a practical diagnostic and therapeutic tool that allows bed-side diagnosis and monitorization, and emerges to be a convenient procedure for routine work-up to understand this soft tissue complication.
Conflict of interestThe authors declare that they have no conflict of interest.