Antineutrophil cytoplasmic antibodies (ANCA) associated vasculitides include granulomatosis with polyangiitis (GPA, previously called Wegener's), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA), previously called Churg-Strauss). In this report we used mycophenolate mofetil (MMF) and steroids to induce and maintain remission in two newly diagnosed cases with c-ANCA associated GPA. The two patients’ maintained remission with no disease relapses during one year follow-up.
Las vasculitis asociadas a anticuerpos anticitoplasma de neutrófilos (ANCA) incluyen granulomatosis con poliangeitis (GPA) anteriormente llamada de Wegener, poliangeítis microscópica (MPA) y granulomatosis eosinofílica con poliangeítis (EGPA) anteriormente llamada síndrome de Churg-Strauss. En este informe utilizamos micofenolato mofetilo (MMF) y esteroides para inducir y mantener la remisión en 2 casos recientemente diagnosticados con GPA asociado a c-ANCA. La remisión mantenida de los 2 pacientes sin enfermedad recae durante un año de duración del seguimiento.
The antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitides comprise granulomatosis with polyangiitis (GPA, in the past called Wegener's disease), eosinophilic granulomatosis with polyangiitis (EGPA, previously called Churg-Strauss) and microscopic polyangiitis (MPA).1 GPA is characterized by granulomatous inflammation of the respiratory tract and by autoantibodies against the neutrophil granule serine protease proteinase 3 in 66% of patients or against another neutrophil granule component, myeloperoxidase, in 24% of patients.2 Immunosuppressive drugs have changed the prognosis of systemic GPA. Nowadays, the main residual problems are frequent illness relapses, for which the management is largely undefined.3 Untreated generalized or severe GPA typically carries a dismal prognosis, with up to 90% of patients dying within 2 years, usually of respiratory or renal failure. Even non-renal GPA carries a mortality rate of up to 40%. For that reason the treatment should be tailored to treat GPA manifestations and at the same time minimizing long-term toxicities.4 Since cyclophosphamide (CTX) was introduced for the treatment of ANCA-associated vasculitis (AAV), the mortality of these diseases has decreased considerably. However, the treatment itself may lead to acute and chronic serious adverse effects, which can contribute much to the morbidity and mortality. Recently Rituximab (RTX), an anti-CD20 monoclonal antibody, stands at the top of new options for the treatment of AAV.5 In a single-center non-blinded clinical trial Hu et al.6 compared the clinical efficacy of mycophenolate mofetil (MMF) with that of intermittent CTX pulse therapy as induction therapy in patients with AAV and moderate renal involvement. The authors suggested that MMF effectively ameliorates disease activity and considerably improves the renal function in patients with AAV.6
In this report we present two cases with established diagnosis of GPA where we used corticosteroid and MMF for both induction and maintenance of remission with no relapse during one year of follow-up. We review the literature regarding the currently applied different therapeutic options available for induction and maintenance of remission in GPA.
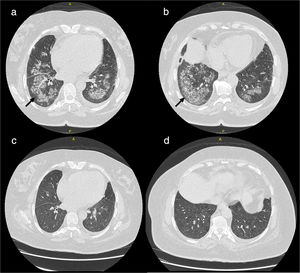
Cases presentationsCase 1A 52 year-old female patient presented with fever, anorexia, intense myalgia and weight loss during 2 months. The onset was associated was painful swollen hand joints, knees and ankles. She developed pulmonary symptoms in the form shortness of breath, chest pain, cough and orthopnea. The patient mentioned that six months before her other complaints started she had developed nasal symptoms with rhinorrhea, formation of nasal crusts and sores, which were diagnosed as allergic rhinitis. Initial laboratory investigations showed elevated markers of inflammation ESR 1st hour and CRP levels, normal liver function tests and normal serum creatinine levels and further investigations confirmed the presence of c-ANCA associated GPA. High-resolution computed tomography (HRCT) showed extensive pulmonary infiltrates (Fig. 1). The patient received oral corticosteroids (prednisolone) in a dose of 30mg/day/po combined with MMF in a dose of 2g/day/po. One month after the start of the treatment she showed much improvement of the constitutional manifestations, respiratory symptoms and laboratory markers of inflammation. The repeated HRCT showed almost complete resolution of the pulmonary infiltrates (Fig. 1). The dosage of prednisolone could be tapered over six months to 5mg/day/po and the dose of MMF was kept the same. During one year of follow up there were no signs or symptoms of disease relapse.
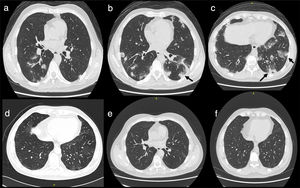
Case 2A 42 years old male patient presented in our facility with acute onset of respiratory symptoms including dry cough, dyspnea and chest pain. The disease onset was preceded by constitutional symptoms fever, anorexia, intense myalgia and weight loss of one month duration. HRCT was ordered and showed widespread pulmonary infiltrates highly suspect of GPA (Fig. 1). c-ANCA was ordered and showed positive results for c-ANCA together with elevated markers of inflammation ESR 1st hour and CRP levels. The patient started with corticosteroid prednisolone 20mg/day/po and MMF 1500mg/day/po. The patient showed dramatic response with much improvement of the respiratory symptoms and other constitutional manifestations. One month after the start of the treatment the HRCT showed almost complete resolution of the pulmonary infiltrates (Fig. 2). The dosage of Prednisolone was tapered to 5mg/day/po and the dosage of MMF was kept the same. During one year of follow up no relapse was reported.
DiscussionSeveral immunosuppressive agents can be used for maintenance therapy after induction of remission in patients with ANCA-associated vasculitis, with no firm evidence that one agent is superior to others.7 Maintenance therapy is mandatory after induction of remission to reduce the relapse rate. Among patients with GPA, up to 50% relapse within the first 5 years. Azathioprine is the main maintenance drug, although methotrexate and MMF may be used as second-line drugs. Recently biological therapy such as rituximab appeared to be successful.5,8
In a previous study Hu et al.,6 compared the clinical efficacies of MMF versus intermittent CTX pulse therapy as induction treatments in patients with AAV in 35 patients with only moderate renal impairment (28 were MPO-ANCA positive and 2 were PR3-ANCA positive). In their study the authors concluded that MMF effectively ameliorates disease activity and considerably improves renal function in patients with AAV. The authors suggested that MMF combined with corticosteroids may be useful as an alternative for CTX for induction therapy in GPA with generalized disease and moderate renal impairment.6 In our report we treated two cases with definitive GPA without renal involvement and showed that MMF can be used for both induction as well as maintenance of remission in GPA.
MMF is a prodrug of mycophenolic acid (MPA), an inhibitor of inosine monophosphate dehydrogenase (IMPDH). This is the rate-limiting enzyme in de novo synthesis of guanosine nucleotides, whereas both T- and B-lymphocytes are more dependent on this pathway than other cell types. On the other hand T cells are considered the crucial and key players in GPA disease pathogenesis and this in turn would explain the beneficial use of MMF in both induction and maintenance of remission in GPA, as documented by Hu et al.6 and confirmed by our two cases. Furthermore, MPA is a fivefold more potent inhibitor of the type II isoform of IMPDH, which is expressed in activated lymphocytes, than of the type I isoform of IMPDH, which is expressed in most cell types. Therefore MPA has a more potent cytostatic effect on lymphocytes than on other cell types. This is the principal mechanism by which MPA exerts its immunosuppressive effects. Moreover three other mechanisms may also contribute to the efficacy of MPA on T cells. First, MPA can induce apoptosis of activated T-lymphocytes, which may eliminate clones of cells responding to antigenic stimulation. Second, by depleting guanosine nucleotides, MPA suppresses glycosylation and the expression of some adhesion molecules, thereby decreasing the recruitment of lymphocytes and monocytes into sites of inflammation. Third, by depleting guanosine nucleotides MPA also depletes tetrahydrobiopterin, a co-factor for the inducible form of nitric oxide synthase (iNOS). MPA therefore suppresses the production by iNOS of NO, and consequent tissue damage mediated by peroxynitrite. The drug also suppresses primary, but not secondary, antibody responses.9
ConclusionMMF can be successfully applied as treatment of c-ANCA associated GPA. Our report showed that MMF can be used safely of both induction and maintenance of remission. Induction of remission can be achieved rapidly within one month of initiation of treatment with no disease relapse reported after one year of follow-up. Further studies are warranted in a larger cohort of patients for with longer follow-up to confirm our findings. In future studies comparison of MMF and RTX regarding both efficacy and safety profiles of each could be considered.
Conflict of interestThe authors declare that they have no conflicts of interest concerning this article.