Ixekizumab (IXE) is a selective interleukin 17A (IL-17A) monoclonal antibody approved for the treatment of psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA). Limited real-world data are available on its retention rate and effectiveness. The objective of this study was to assess the one-year retention rate of IXE in a real-world cohort of patients with axSpA and PsA and to identify potential predictive factors for drug retention.
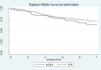
MethodProspective and observational study derived from BIOBADASER 3.0, a multicenter registry of advanced therapies including patients who have ever received IXE for PsA or axSpA. The one-year retention rate of the treatment in both diseases was evaluated using Kaplan–Meier curves and multivariable Cox regressions.
ResultsA total of 335 patients ever exposed to IXE were included (PsA=250; axSpA=85). IXE was used as first-line treatment only in 5.3% of patients, and after TNFi in 94.7% of patients. In axSpA and PsA, drug survival at 12 months was 69.5% (95% CI 64.0–74.3), slightly higher in PsA (71.3% (95% CI 65.0–75.6)) versus axSpA (63.8% (95% CI 51.5–73.7)). The multivariable Cox regression models showed that female sex and longer disease duration were factors associated with IXE withdrawal in the whole population, while concomitant use of methotrexate reduced the risk of discontinuation.
ConclusionsIn this real-world study, IXE showed an acceptable retention rate in patients with PsA and axSpA after one year of follow-up. Female sex and longer disease duration were associated with risk of withdrawal.
Ixekizumab (IXE) es un anticuerpo monoclonal selectivo de la interleucina 17A (IL-17A) aprobado para el tratamiento de la artritis psoriásica (PsA) y la espondiloartritis axial (EspAax). Existen datos limitados de vida real sobre su tasa de retención y efectividad. El objetivo de este estudio fue evaluar la tasa de retención a un año de IXE en una cohorte de vida real de pacientes con EspAax y PsA, y determinar los posibles factores predictivos de la retención del fármaco.
MétodosEstudio prospectivo y observacional derivado de BIOBADASER 3.0, un registro multicéntrico de terapias avanzadas que incluye a pacientes que alguna vez han recibido IXE para PsA o EspAax. La tasa de retención del tratamiento a un año en ambas enfermedades se evaluó utilizando curvas de Kaplan-Meier y regresiones de Cox multivariables.
ResultadosSe incluyeron un total de 335 pacientes que alguna vez estuvieron expuestos a IXE (PsA=250; EspAax=85). IXE se utilizó como tratamiento de primera línea solo en el 5,3% de los pacientes y, después de TNFi, en el 94,7% de los pacientes. En EspAax y PsA, la supervivencia del fármaco a los 12 meses fue del 69,5% (IC95%: 64,0-74,3), ligeramente mayor en PsA (71,3%; IC95%: 65,0-75,6) frente a EspAax (63,8%; IC95%: 51,5-73,7)). Los modelos de regresión de Cox multivariables mostraron que el sexo femenino y una mayor duración de la enfermedad fueron factores asociados con la interrupción de IXE en toda la población, mientras que el uso concomitante de metotrexato redujo el riesgo de interrupción.
ConclusionesEn este estudio del mundo real, IXE mostró una tasa de retención aceptable en pacientes con PsA y EspAax después de un año de seguimiento. El sexo femenino y una mayor duración de la enfermedad se asociaron con el riesgo de interrupción.
Spondyloarthritis (SpA) comprises a heterogeneous group of immune-mediated diseases characterized by inflammation affecting the axial skeleton and/or peripheral joints, enthesis and extra-musculoskeletal manifestations, such as skin/nail psoriasis, uveitis, and inflammatory bowel disease (IBD).1 The most prevalent subtypes of SpA are represented by psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA), which share both genetic and clinical characteristics and are usually placed under the umbrella of SpA.2 These diseases represent a public health burden due to the significant morbidity associated which may result in permanent mobility limitations and poorer quality of life.
A wide array of therapeutic options is now available for treating patients with PsA and axSpA after demonstrating safety and efficacy in randomized controlled trials. Available drugs target different signaling pathways, such as inhibitors of tumor necrosis factor (TNF), interleukin (IL)-17 and JAK-STAT pathways. In addition, patients with PsA can be treated with inhibitors of IL-12/23, IL-23, and phosphodiesterase type 4 (PDE4). The European Alliance of Associations for Rheumatology (EULAR), the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA), and the Pan American League of Associations for Rheumatology (PANLAR) have developed updated recommendations for the management of PsA, encompassing all currently available treatment options to support physicians in decision-making.3–5
Ixekizumab (IXE) is an IgG4 monoclonal antibody that specifically binds to interleukin 17A approved for both PsA and axSpA, among other conditions. IXE has been shown to be effective in several phase III clinical trials in patients with PsA (SPIRIT-P1 and SPIRIT-P2),6,7 as well as in patients with radiographic axSpA (COAST-V and COAST-W)8,9 and non-radiographic axSpA (COAST-X).10 However, there are limited real-world data on drug survival in routine clinical practice, making the Spanish registry BIOBADASER 3.0 a key resource to evaluate real-world data in an observational cohort of patients treated with IXE.11 Accordingly, the objective of this study was to evaluate the 12-months retention rate to IXE and to identify potential predictive factors for drug withdraw in patients with axSpA and PsA.
Materials and methodsDesignThis was a 12-months prospective, observational study conducted using real-world data from the BIOBADASER 3.0 nationwide multicenter registry, which comprises patients with rheumatic diseases undergoing treatment with biologic disease-modifying antirheumatic drugs (bDMARDs) (including biosimilars) and targeted synthetic DMARDs (tsDMARDs).11 Established in 2001 and promoted by the Spanish Foundation of Rheumatology, BIOBADASER has consistently collected data from routine clinical practice, which is then monitored yearly for quality control. The full protocol of BIOBADASER 3.0 is available online (https://biobadaser.ser.es/protocolo.aspx). The collection of IXE treatments started after the approval of this drug by the Spanish Health Ministry, which was in 2019, and thus, the information presented in this manuscript includes data from BIOBADASER phase 3.0 up to October 2023, when the data was locked for the current analysis.
Human rightsEthical approval for the registry was obtained from the Hospital Clínic de Barcelona Research Ethics Committee (FER-ADA-2015-01), while the current reference committee is the Hospital de Canarias. All participants willingly signed an informed consent to participate in the BIOBADASER registry.
PopulationFor this study, we included adult patients (≥18 years) diagnosed with PsA or axSpA based on their clinician's assessment and fulfilling the CASPAR and ASAS (Assessment of Spondyloarthritis International Society) classification criteria,12,13 respectively. Patients treated with IXE in this registry include both those naïve to other ts/bDMARDs and also those treated in subsequent lines.
In this analysis, we restricted our focus to the initial 12-months of follow-up, since at the time of the database lock many patients were not evaluated at the 2-year visit.
VariablesA specific case report form was used to collect clinical data. The variables included in this analysis were:
- -
Sociodemographic data such as age at the initiation of the IXE, sex and smoking status (never, ever or current) were collected at the baseline assessment.
- -
Disease-related variables, disease duration (time since the diagnosis until treatment initiation) and uveitis ever.
- -
Disease activity was assessed at the time of the IXE initiation, and included tender joints count, swollen joints count and patient's global health assessment using a visual analogue scale ranging from 0 to 10. Erythrocyte sedimentation rate (ESR) in mmHg and C-reactive protein (CRP) in mg/L were also collected. In addition, the composite disease activity score 28 (DAS28), the Disease Activity index for Psoriatic Arthritis (DAPSA)14,15 and the Axial Spondyloarthritis Disease Activity Score (ASDAS)16 were evaluated at baseline.
- -
Treatments: all patients included in this study were about to initiate IXE treatment at any line. Data on the dates of therapy initiation and withdrawal were collected to evaluate the drug retention rate, as well as the reason of withdrawal.
First, a descriptive analysis of baseline variables was performed using means and standard deviation (SD) for continuous variables, and absolute and relative frequencies for qualitative variables.
The retention rate of IXE in the PsA and axSpA populations was evaluated using a Kaplan–Meier curves. Retentions rates were also stratified according to whether the patient received IXE in first line versus second or subsequent lines. The reasons of discontinuation were also described per group.
Finally, multivariate Cox regressions were performed to evaluate baseline predictive factors associated with drug discontinuation (hazard ratios, HR), stratified by disease.
All contrasts were bilateral and considered significant when the p-value <0.05. Data were analysed using Stata 13.1 (StataCorp®).
ResultsA total of 335 patients who received at least one dose of IXE were included in this analysis. Among these, 85 (25.4%) and 250 (74.6%) had a diagnosis of axSpA and PsA, respectively. Baseline demographic and clinical characteristics in the overall population and stratified by disease are represented in Table 1. The mean age at treatment initiation was 52.1 (SD=10.9) years. Males represented 46.6% of the total population, with a higher proportion in axSpA (60%) compared to PsA (42%). Mean disease duration was 10.9 (SD=8.9) years. IXE was prescribed as initial biologic DMARD in 5.3% of patients only and as second or subsequent line in 94.7%.
Baseline characteristics of the overall population and per disease.
| OverallN=335 | axSpAN=85 | PsAN=250 | |
|---|---|---|---|
| Age at treatment initiation, mean (SD) | 52.1 (10.9) | 50.3 (11.2) | 52.7 (10.8) |
| Age at diagnosis, mean (SD) | 41.2 (11.6) | 37.6 (11.0) | 42.4 (11.5) |
| Gender (male), n (%) | 156 (46.6) | 51 (60.0) | 105 (42.0) |
| Smoker, n (%) | |||
| No | 174 (51.9) | 43 (50.6) | 131 (52.4) |
| Yes | 79 (23.6) | 24 (28.2) | 55 (22.0) |
| Former smoker | 56 (16.7) | 13 (15.3) | 43 (17.2) |
| Unknown | 26 (7.8) | 5 (5.9) | 21 (8.4) |
| Disease duration, mean (SD) | 10.9 (8.9) | 12.7 (11.0) | 10.3 (8.1) |
| CRP (mg/L), mean (SD) | 11.5 (21.1) | 13.8 (21.3) | 11.1 (21.1) |
| ESR (mm/h), mean (SD) | 21.8 (21.7) | 21.2 (21.3) | 21.8 (21.8) |
| HLA-B27, n (%) | 78 (23.3) | 54 (63.5) | 24 (9.6) |
| Uveitis, n (%) | 6 (1.8) | 5 (5.9) | 1 (0.4) |
| Radiographic axSpA, n (%) | – | 67 (78.8) | – |
| BASDAI, mean (SD) | – | 6.2 (2.4) | – |
| ASDAS, mean (SD) | – | 3.6 (1.1) | – |
| DAS28-ESR, mean (SD) | – | – | 4.2 (1.4) |
| DAPSA, mean (SD) | – | – | 29.4 (13.9) |
| Number of treatments, n | 341 | 86 | 255 |
| Order of IXE treatment, n (%) | |||
| First line | 18 (5.3) | 3 (3.5) | 15 (5.9) |
| Second or later lines | 323 (94.7) | 83 (96.5) | 240 (94.1) |
| Prior exposure to b/tsDMARDs (for IXE treatments on 2nd or later lines), n (%) | |||
| TNFi | 292 (92.1) | 78 (95.1) | 214 (91.1) |
| JAKi | 22 (6.9) | 3 (3.7) | 19 (8.1) |
| IL-17Ai | 97 (30.6) | 28 (34.1) | 69 (29.4) |
| IL-12/23i | 68 (21.5) | 3 (3.7) | 65 (27.7) |
| PDE4i | 4 (1.3) | 0 (0.0) | 4 (1.7) |
| Concomitant use of methotrexate | 97 (28.5) | 7 (8.1) | 90 (35.3) |
| Concomitant use of other csDMARDs* | 33 (9.7) | 4 (4.6) | 29 (11.4) |
| Concomitant use of glucocorticoids | 88 (25.81) | 11 (12.8) | 77 (30.2) |
ASDAS: Ankylosing Spondylitis Disease Activity Score; axSpA: axial spondyloarthritis; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; CRP: C-reactive protein; DAPSA: Disease Activity Psoriatic Arthritis Score; DAS28-ESR: Disease Activity Score 28 – Erythrocyte Sedimentation Rate; ESR: erythrocyte sedimentation rate; IL-12/23i: interleukin 12/23 inhibitors; IL-17Ai: interleukin 17A inhibitors; IXE: ixekizumab; JAKi: janus kinase inhibitors; PDE4i: phosphodiesterase 4 inhibitors (PDE4i); PsA: psoriatic arthritis; SD: standard deviation; TNFi: tumour necrosis factor inhibitors.
A total of 341 treatments for 335 patients were included in this analysis. In the overall population, the probability of IXE retention after 12 months of follow-up was 69.5% (95% CI: 64.0–74.3) (Table 2). Drug retention was higher in patients treated in first line (81.7% (95% CI: 53.1–93.8)) in comparison with those treated in second or later lines (68.8% (95% CI: 63.1–73.8)).
Probability of retention after 12-months of treatment with IXE and reasons of discontinuation.
| Overall treatmentsN=341 | axSpAN=86 | PsAN=255 | |
|---|---|---|---|
| Probability of retention (95% CI) 1 year | |||
| Total | 69.5 (64.0–74.3) | 63.8 (51.5–73.7) | 71.3 (65.0–76.6) |
| First line | 81.7 (53.1–93.8) | – | 92.3 (56.6–98.9) |
| Second or later lines | 68.8 (63.1–73.8) | 65.2 (52.7–75.1) | 70.0 (63.4–75.6) |
| Discontinuation, n (%) | 135 (40.3) | 29 (34.1) | 106 (42.4) |
| Discontinuation due to inefficacy, n (%) | |||
| Among patients who discontinued | 94/135 (69.6) | 22/29 (75.9) | 72/106 (67.9) |
| Among the total population | 94/335 (28.1) | 22/85 (25.9) | 72/250 (28.8) |
| Discontinuation due to adverse event, n (%) | |||
| Among patients who discontinued | 30/135 (22.2) | 7/29 (24.1) | 23/106 (21.7) |
| Among total population | 30/335 (9.0) | 7/85 (8.2) | 23/250 (9.2) |
axSpA: axial spondyloarthritis; PsA: psoriatic arthritis.
When stratifying patients by diagnosis, we found that the probability of retention after one year was slightly higher in PsA patients in comparison with axSpA (71.3% (95% CI: 65.0–76.6) versus 63.8% (95% CI: 51.5–73.7), respectively), but with no significant differences (p=0.23) (Table 2 and Fig. 1). The number of discontinued treatments in the overall population after 12-months follow-up was 135 (40.3%), mainly due to inefficacy (69.6%), with no differences between axSpA and PsA, and 22.2% of withdrawals were due to adverse events. The description of adverse events is provided in Supplementary Table 1.
Baseline factors associated with IXE withdrawalA multivariate Cox regression in the overall population and stratified by disease was conducted to evaluate factors associated with IXE withdrawal (Table 3).
Baseline factors independently associated with the withdrawal of IXE per disease.
| Overall | axSpA | PsA | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| PsA (ref. axSpA) | 0.89 (0.55–1.43) | 0.629 | – | – | – | – |
| Second or later lines (ref. first line) | 1.44 (0.45–4.58) | 0.537 | 0.14 (0.03–0.71) | 0.018 | 4.32 (0.60–31.23) | 0.147 |
| Female (ref. male) | 2.20 (1.41–3.44) | 0.001 | 1.27 (0.53–3.04) | 0.593 | 2.59 (1.48–4.54) | 0.001 |
| Age at treatment initiation | 1.00 (0.98–1.02) | 0.680 | 1.03 (0.99–1.07) | 0.113 | 0.98 (0.96–1.00) | 0.083 |
| Disease duration | 1.03 (1.00–1.05) | 0.018 | 1.04 (1.01–1.08) | 0.025 | 1.01 (0.98–1.05) | 0.495 |
| Concomitant use of MTX (ref. no MTX) | 0.53 (0.31–0.89) | 0.017 | 0.97 (0.23–4.20) | 0.971 | 0.50 (0.29–0.88) | 0.016 |
axSpA: axial spondyloarthritis; CI: confidence interval; HR: hazard ratio; MTX: methotrexate; PsA: psoriatic arthritis; ref.: reference.
Bold: significant differences.
In the overall population, the factors associated with a greater risk of IXE discontinuation were female sex (HR 2. 20 (95% CI: 1.41–3.44)) and longer disease duration (HR 1.03 (95% CI: 1.00–1.05)), whereas is the concomitant use of methotrexate decreases the risk of discontinuation (HR 0.53 (95% CI: 0.31–0.89)). In patients with axSpA, the treatment in second or later lines notably reduces the risk of IXE withdrawal compared to first-line treatments (HR 0.14 (95% CI: 0.03–0.71)) while the longer disease duration increases this risk (HR 1.04 (95% CI: 1.01–1.08)). In patients with PsA, the factors significantly associated with IXE withdrawal were being a female (HR 2.59 (95% CI: 1.48–4.54)) and using methotrexate concomitantly (HR 0.50 (95% CI: 0.29–0.88)).
DiscussionIn this multicentre real-world study, IXE exhibited an acceptable retention rate of 69.5% in patients with PsA and axSpA after one-year of follow-up, with a higher rate in those treated in the first line (81.7%). When stratifying by disease, the probability of retention was 71.3% for PsA and 63.8% for axSpA after one year. Overall, 40.3% of patients discontinued the treatment after one year, most of them due to inefficacy.
To date, real-world data on the use of IXE for PsA and, most importantly, in axSpA, is scarce. For this reason, this study provides new evidence on the use of this drug in clinical practice. The retention rate of IXE in Spain was quite similar to that observed in a single-centre study from the United Kingdom, with a 69% probability in both studies.17 This reflects a consistency in our findings, which can mirror the clinical practice in other regions. When stratifying by disease, we again found a similar retention rate in both studies, with a slightly higher probability in PsA patients. The retention rate in PsA was around 71.3% in our study, which is subtly higher compared to that reported by Braña et al.18 This can be explained by the lower number of patients included and by the single-centre design of that study.
Factors associated with a greater risk of IXE withdrawal in the overall population were female sex and longer disease duration, whereas concomitant methotrexate decreased the risk of withdrawal. Interestingly, neither the diagnosis nor the fact of initiating IXE as a first or second/later lines seemed to have an influence on the retention rate. Female sex has been previously reported as a risk factor for drug withdrawal among PsA patients. A previous analysis on secukinumab (another IL-17A inhibitor) reported that females had a higher risk of drug discontinuation in axSpA and PsA compared to male patients.19 Similarly, other studies reported that female sex represents a risk factor for treatment discontinuation in PsA, probably due to the higher prevalence of polyarticular patterns and the greater incidence of concomitant fibromyalgia in this population.20,21 Unfortunately, in this cohort, the presence of fibromyalgia was not collected to verify whether this factor explains the lower retention rate in the female population. While female sex was not associated with a lower retention rate in axSpA patients in our analysis, this has been reported in other studies with bDMARDs.22,23
Methotrexate was, conversely, associated with a decreased risk of IXE withdrawal in the overall population and in PsA. Concomitant use of methotrexate has previously demonstrated an improved retention rate of infliximab and golimumab in patients with PsA.24,25 However, clinical trials with IXE indicate that concomitant use of methotrexate does not impact the therapeutic response or retention rate of the drug.26–28 Our results showed the opposite, while these results need to be interpreted with caution since this is an observational study with a potential prescription bias.
In our study, the majority of patients were treated with IXE in second or later lines, as reported in previous real-world data from our country.29,30 However, this had no impact on the retention rate in the overall population, as shown in the Cox regression. Curiously, in our axSpA patients, being treated in second or later lines was found as a protective factor against IXE withdrawal. However, due to the small number of patients treated in the first line and the potential use of IXE as the last alternative for patients who did not respond to previous treatments, these results should be interpreted with caution. The high percentage of patients treated with IXE in second or later lines reflects the Spanish regulations regarding the prescription of biological drugs which generally position the use of biosimilar anti-TNFs as the first therapeutic option for these patients.
Among patients who discontinued treatment, the primary reason for withdrawal was inefficacy (70%), while 22% discontinued due to adverse events, which in line with data reported previously.17 These percentages were very similar when stratified by both diseases, although there was a slightly higher rate of discontinuation in PsA compared to axSpA. This slightly increased discontinuation in PsA may be explained by the greater heterogeneity of the disease, with multiple affected domains, and the challenge of achieving efficacy across all domains (e.g., joints, enthesis and skin).
This study has both limitations and strengths. One limitation is that we did not report the effectiveness of these drugs. The prospective nature of the study meant that some patients did not complete the follow-up visits, resulting in fewer patients with available data regarding disease activity. Therefore, we focused this analysis on the retention rate, which accounts for patient loss of follow-up. Another limitation is the absence of certain clinical information in this registry, such as the presence of concomitant IBD. One strength of this study is its prospective design, which reduces recall bias and missing data typically seen in retrospective analyses. Additionally, the observational nature of this study, using real-world data, enhances the external validity of the findings. Lastly, the quality of the collected data is significant, as BIOBADASER is a well-known registry that includes both online and on-site monitoring by a specialized Clinical Research Associate once a year, ensuring the reliability of the results.
In conclusion, this multicentre analysis provided new real-world data on the use of IXE in the BIOBADASER Spanish registry, showing an optimal retention rate in patients with PsA and axSpA after one year of follow-up. Overall, female sex and longer disease duration were associated with an increased risk of treatment withdrawal while the concomitant use of methotrexate with a reduced risk. The reasons for drug discontinuation were consistent with previous literature.
CRediT authorship contribution statementData curation: VJ, SB, SM-D, YP-V, PP-R, JM, AM-V, LM, DR-M, LM, TP-P. Methodology: CL-M, LO-V, FS-A, I-C. Statistical analysis: LO-V, FS-A. Supervision: CL-M, IC. Interpretation of the data: CL-M, LO-V, FS-A, IC. Writing original manuscript: CL-M. Reviewing and manuscript approval: all.
Ethical approvalThe study was approved by the Ethics Review Committee of the Hospital Universitario Clinic Barcelona (approval code FER-ADA-2015-01), although the Hospital de Canarias Ethics Committee currently acts as the reference committee.
Informed consentInformed consent was obtained from all the participants.
Consent for publicationNot applicable.
FundingBIOBADASER was supported by the Spanish Foundation of Rheumatology and Spanish Agency of Medicines and Medical Devices (AEMPS), as well as the following pharmaceutical companies: Abbvie, Biogen, Bristol-Myers and Squibb (BMS), Celltrion, Galapagos, Janssen, Lilly, Merck Sharp and Dohm (MSD), Novartis, Pfizer, Regeneron, and Samsung Bioepis. The abovementioned pharmaceutical companies had no role in data collection, analysis, interpretation, and presentation of the data.
Conflict of interestAuthors declare no competing interests regarding this manuscript.
Data availabilityThe data supporting the findings of this study are available from the Spanish Foundation of Rheumatology, although restrictions apply to the availability of these data, which were used under the license for the current study and are therefore not publicly available. However, the data are available from the authors upon reasonable request and with permission from the Spanish Foundation of Rheumatology.
We would like to thank the Research Unit of the Spanish Society of Rheumatology (SER) for their support in logistics and statistical analyses. The authors would like to thank all investigators participating in the BIOBADASER registry.