Plantar fasciitis is a common cause of heel pain worldwide, having a high burden on quality of life.1 Corticosteroid plantar injection (CPI) is a treatment option frequently used, especially when conservative strategies fail. Although efficacy on relieving pain has already been shown,2,3 data on predictors of relapse are scarce.
The rationale behind this study was to assess the clinical response to CPI and the influence of socio-demographic and clinical factors on the risk of relapse.
This retrospective study included 85 patients from our rheumatology department, with plantar fasciitis who underwent plantar injection with 40 milligrams of methylprednisolone guided either by body landmarks or ultrasound, between 2017 and 2018. Patients with chronic rheumatic inflammatory disorders were excluded. Socio-demographic and clinical information were obtained through the clinical records. Missing data and information about clinical evolution after the CPI were obtained by telephonic survey. Pain was assessed before and after CPI using the visual analogue scale (VAS). Patients were asked to evaluate the efficacy in relieving pain using a Likert scale. Paired sample t-test was used to evaluate the efficacy of CPI on relieving pain. Cox-regression was used to assess predictors of relapse after CPI.
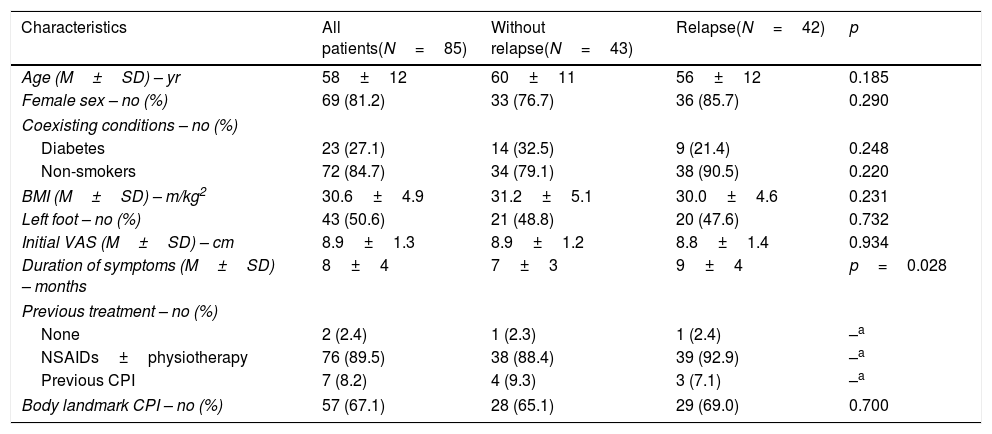
Sixty-nine (81.2%) patients were female and the mean age was 58±12 years. The average body mass index (BMI) was 30.6±4.9kg/m2. The mean duration of symptoms before the procedure was 8.0±3.6 months and the mean VAS score of pain was 8.9±1.3cm. Most CPI (67.1%) were guided by body landmarks. Table 1 summarizes the baseline characteristics. There was a significant reduction in VAS score after the CPI (8.9 vs 1.3cm, p<0.001), which illustrates the effectiveness of CPI in the treatment of plantar fasciitis, as supported by other studies.2,3 In fact, most patients agreed (38.8%) or strongly agreed (42.4%) with its effectiveness.
Baseline characteristics.
| Characteristics | All patients(N=85) | Without relapse(N=43) | Relapse(N=42) | p |
|---|---|---|---|---|
| Age (M±SD) – yr | 58±12 | 60±11 | 56±12 | 0.185 |
| Female sex – no (%) | 69 (81.2) | 33 (76.7) | 36 (85.7) | 0.290 |
| Coexisting conditions – no (%) | ||||
| Diabetes | 23 (27.1) | 14 (32.5) | 9 (21.4) | 0.248 |
| Non-smokers | 72 (84.7) | 34 (79.1) | 38 (90.5) | 0.220 |
| BMI (M±SD) – m/kg2 | 30.6±4.9 | 31.2±5.1 | 30.0±4.6 | 0.231 |
| Left foot – no (%) | 43 (50.6) | 21 (48.8) | 20 (47.6) | 0.732 |
| Initial VAS (M±SD) – cm | 8.9±1.3 | 8.9±1.2 | 8.8±1.4 | 0.934 |
| Duration of symptoms (M±SD) – months | 8±4 | 7±3 | 9±4 | p=0.028 |
| Previous treatment – no (%) | ||||
| None | 2 (2.4) | 1 (2.3) | 1 (2.4) | –a |
| NSAIDs±physiotherapy | 76 (89.5) | 38 (88.4) | 39 (92.9) | –a |
| Previous CPI | 7 (8.2) | 4 (9.3) | 3 (7.1) | –a |
| Body landmark CPI – no (%) | 57 (67.1) | 28 (65.1) | 29 (69.0) | 0.700 |
BMI: body mass index; CPI: corticosteroid plantar injection; M: mean; no: number; NSAIDs: nonsteroidal anti-inflammatory drugs; SD: standard deviation; VAS: visual analogue scale.
However, after a median follow-up of 19 months (IQR 14–25 months), 42 patients (49.4%) had a relapse of symptoms, on average, 4.9±4.3 months after the procedure, which demonstrates that CPI may only have a short-term efficacy. Nonetheless, VAS score of pain after relapse was significantly lower than the initial VAS (8.9 vs 6.6cm, p<0.001). Moreover, in this study, time-to-relapse was longer than the 1–3 months-efficacy reported in literature.3,4
In univariate analysis, patients who suffered a relapse had a significantly longer duration of symptoms (p=0.028). BMI is considered a risk factor for plantar fasciitis and for recurrence of symptoms.5 Yet, in this study, BMI did not influence the risk of relapse, which may be explained by the fact that most patients were obese and the sample of subjects with normal BMI was short, therefore influencing the results. Moreover, Tsai et al. reported that sonographic guidance was associated with lower recurrence of symptoms,6 which was not observed in this study. The limited number of subjects in whom CPI was guided by ultrasound may have limited this analysis.
In multivariate analysis, after adjusting for sex and age, the duration of symptoms was an independent predictor of relapse (HR 1.10, 95% CI 1.01–1.20, p=0.039), indicating that CPI could be considered an early approach to plantar fasciitis, instead of a second line option.
In conclusion, in accordance to other studies, CPI was effective in alleviating pain in plantar fasciitis, but relapse was common. Furthermore, even after a relapse, the intensity of the pain was lower. Finally, duration of symptoms was an independent predictor of relapse, highlighting the importance of early diagnosis and treatment of plantar fasciitis.
Compliance with ethical standardsAll procedures performed were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.