To design referral criteria from primary care to rheumatology for patients with rheumatic and musculoskeletal diseases (RMDs).
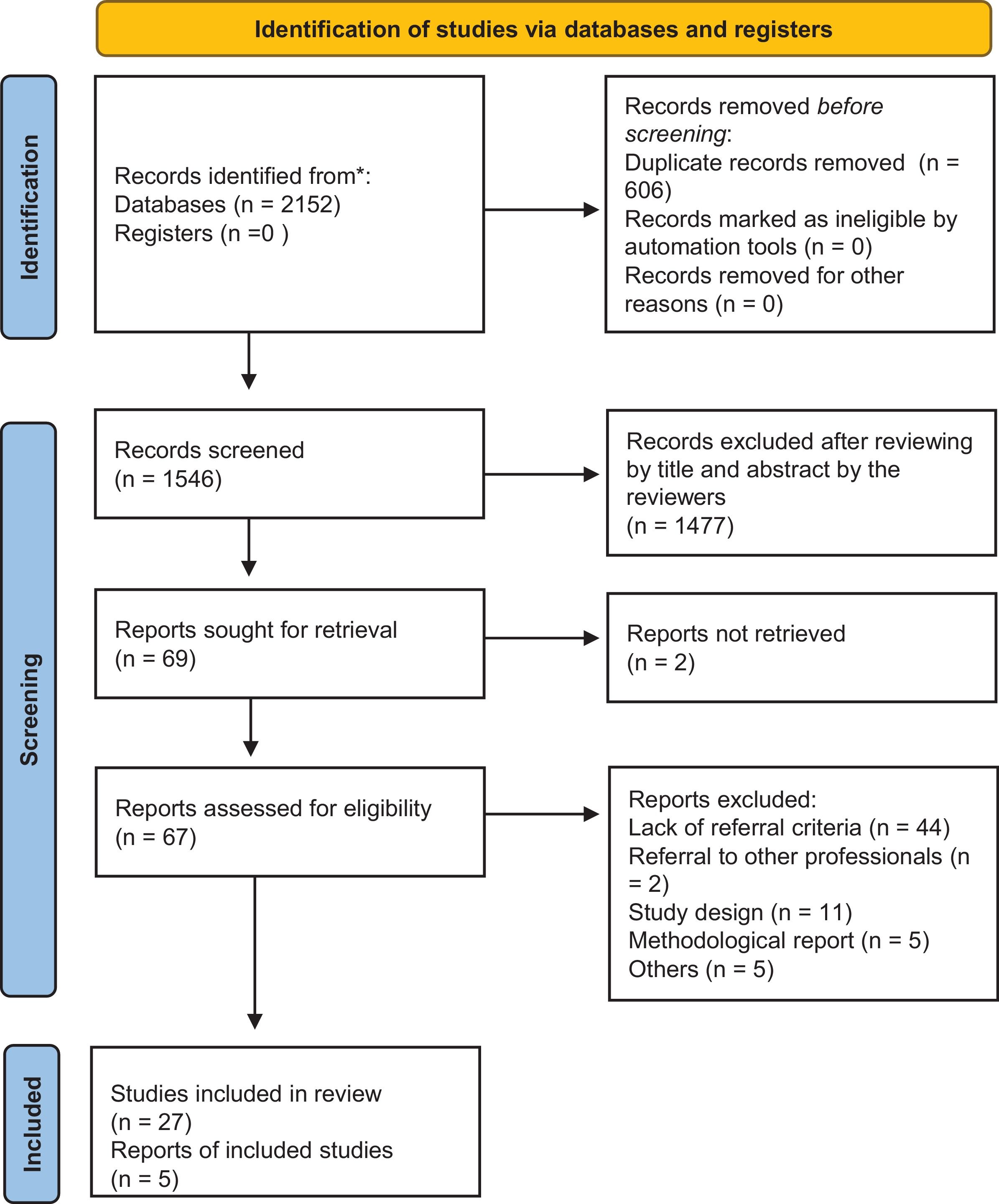
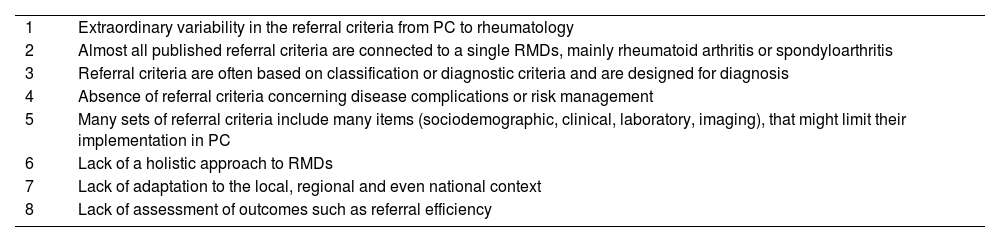
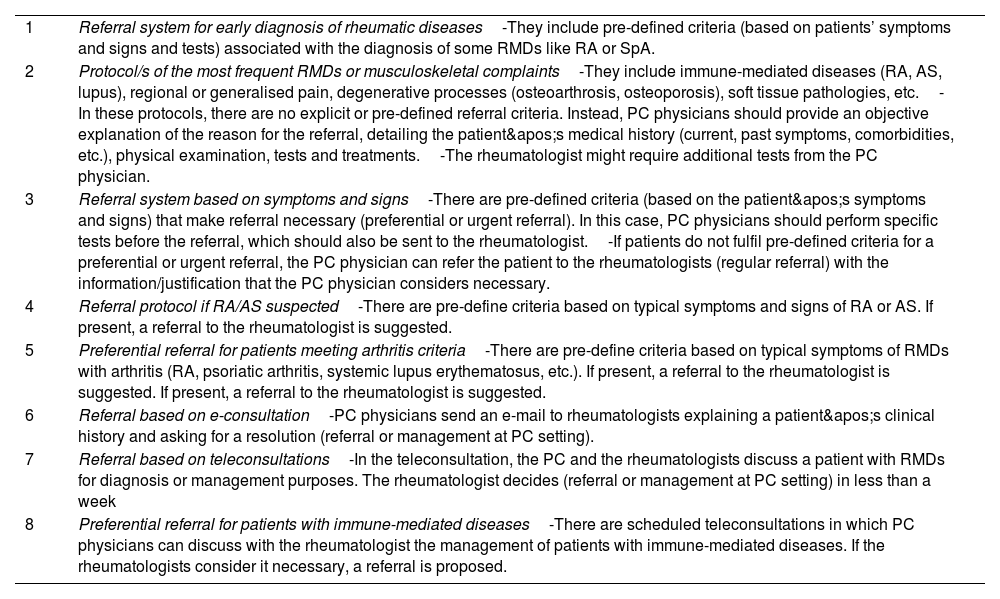
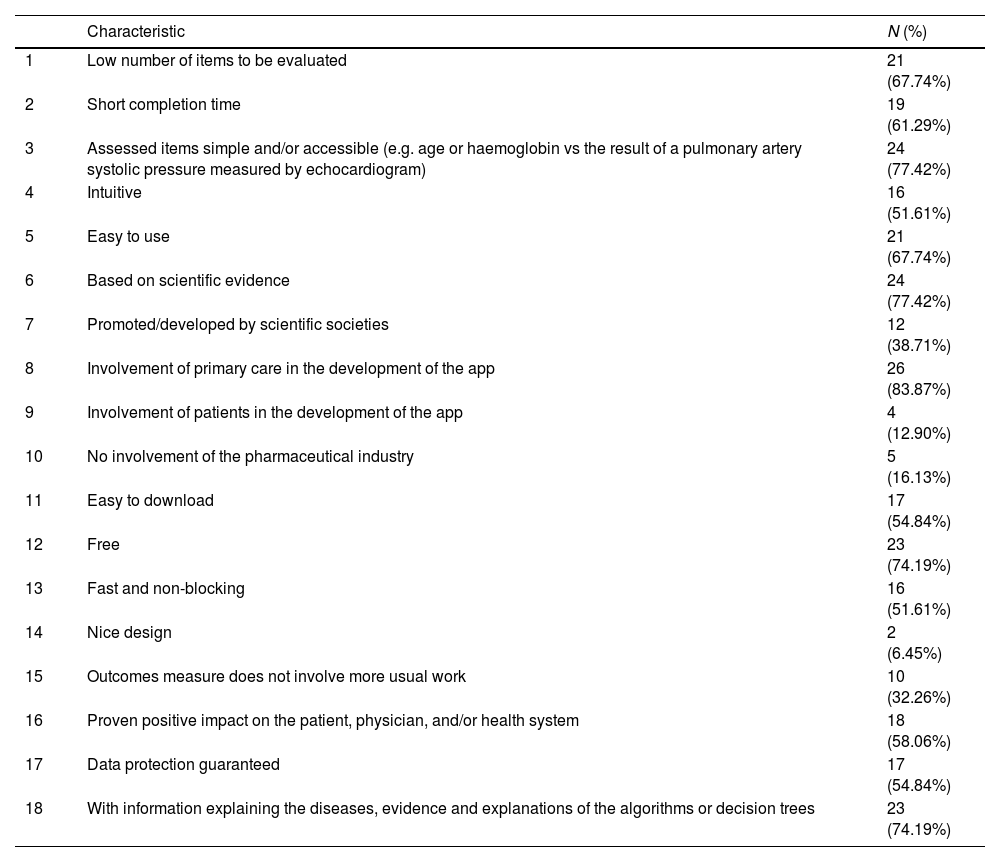
MethodsQualitative study. A panel of 13 expert rheumatologists and primary care physicians was convened. They defined the inclusion and exclusion criteria for a systematic review to analyse the efficacy and safety of primary care referral protocols/systems/criteria for patients with suspected or diagnosed RMDs. A survey was also launched in primary care setting to assess the level of knowledge of RMDs, available referral systems/criteria and the use of digital health tools for patient referral. The experts discussed the systematic review and survey results and defined and agreed on several referral criteria and other helpful educational materials to be included in a digital application (DerivaREUMA app).
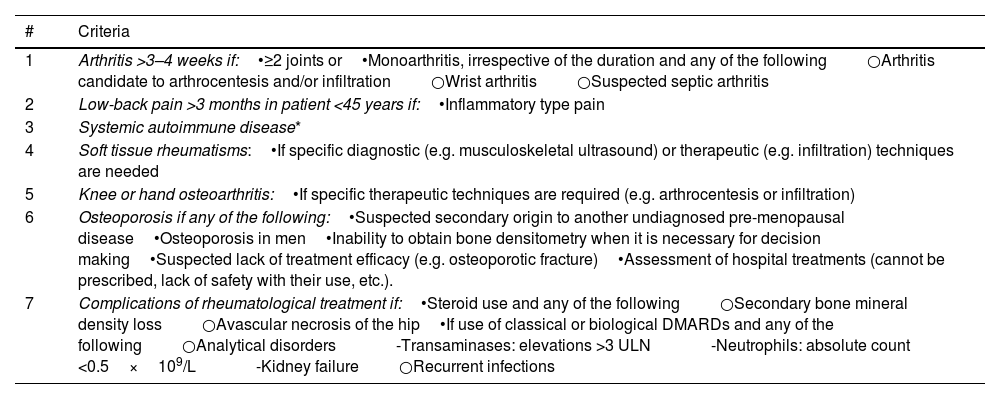
ResultsThe systematic review identified 32 articles of moderate quality. The survey revealed that more than 60% of primary care physicians lacked standard referral protocols/systems/criteria to rheumatology. A consensus was reached on seven referral criteria, starting with one of the following that have more questions and sub-criteria afterwards: (1) arthritis >3–4 weeks; (2) low-back pain >3 months in patients aged <45 years; (3) systemic autoimmune disease; (4) soft tissue rheumatism; (5) knee and hand osteoarthritis; (6) osteoporosis; (7) complications of rheumatological treatment. The app also contains informative and explanatory material.
DiscussionWe have proposed referral criteria and other helpful materials aimed at promoting and improving efficiency in early referral of patients with RMDs from primary care to rheumatology.
Generar criterios de derivación de pacientes con enfermedades reumatológicas y musculoesqueléticas (ERyME) desde atención primaria a reumatología.
MetodologíaEstudio cualitativo. Se estableció un grupo de 13 expertos reumatólogos y médicos de atención primaria. Se realizó una revisión sistemática para analizar la eficacia y seguridad de los criterios de derivación de pacientes con ERyME desde atención primaria a reumatología. Se diseñó una encuesta para evaluar el nivel de conocimiento y manejo de las ERyME en atención primaria, la disponibilidad del sistema de derivación y el uso de las herramientas digitales en salud para la derivación. En una reunión de grupo nominal, se discutieron los resultados de la revisión sistemática y la encuesta, y se consensuaron los criterios de derivación, así como otros materiales de ayuda para ser incluidos en una aplicación (app DerivaREUMA).
ResultadosLa revisión sistemática incluyó 32 artículos de calidad moderada. La encuesta mostró que>60% de los encuestados no disponen de criterios/protocolos/sistemas de derivación a reumatología estandarizados. Se consensuaron 7 criterios de derivación, en los que, partiendo de alguna de las siguientes, se van dando más criterios: 1) artritis>3-4 semanas; 2) dolor lumbar>3 meses en paciente<45 años; 3) enfermedad autoinmune sistémica; 4) reumatismos de partes blandas; 5) artrosis de rodilla y mano; 6) osteoporosis, y 7) complicaciones del tratamiento reumatológico. La app también contiene material informativo y explicativo.
DiscusiónSe proponen unos criterios de derivación y otros materiales de ayuda para incrementar la eficiencia en la derivación de pacientes con ERyME desde atención primaria a reumatología.