Fever of unknown origin is a diagnostic challenge. Among its causes are of Large Caliber Vessels Vasculitis (LCVV), including Takayasu arteritis (TA) and giant cell arteritis (GCA). Early diagnosis is vital to prevent fibrosis of the vessel wall, and consequently, stenoses, aneurysms or occlusions. Imaging techniques can be of great help in recent years, highlighting the temporal artery through ultrasound, MRI and PET-CT.
La fiebre de origen desconocido supone un reto diagnóstico. Entre sus causas se encuentran las Vasculitis de Grandes Vasos (VGV), que incluyen la Arteritis de Takayasu (AT) y de Células Gigantes (ACG). Resulta de vital importancia su diagnóstico precoz para evitar la fibrosis de la pared vascular, y como consecuencia, estenosis, aneurismas u oclusiones. Las técnicas de imagen nos pueden resultar de gran ayuda, destacando en los últimos años la ecografía de la arteria temporal, la RM y el PET-TAC.
The diagnosis of large vessel vasculitis (LVV) is challenging because many of the clinical manifestations are nonspecific and are shared with other types of vasculitis and with various systemic diseases. Both Takayasu's arteritis (TA) and giant cell arteritis (GCA) are considered LVV. It is vital to reach an early diagnosis in order to prevent fibrosis of the vessel wall, and as a result, stenosis, aneurysms or occlusions. Imaging techniques can be helpful, and in recent years the role of temporal artery ultrasound, magnetic resonance imaging (MRI) and the combination of positron emission tomography with computed tomography (PET-TAC) has been highlighted.
This paper describes 2 cases in which the use of PET-CT was definitive for the diagnosis, and then analyzes other imaging techniques.
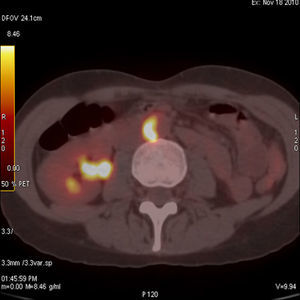
Case 1We present the case of a 43-year-old woman with a history of chronic sinusitis, corneal ulcers and relapsing blepharitis, treated with 30mg of prednisone day after being studied in the infectious diseases unit due to persistent low-grade fever of 37.5°C, where a microbiological origin was ruled out. A few weeks after presenting clinical improvement, her fever returned for 15 days, improving with antipyretics; her blood pressure (BP) levels were 100/60mmHg and she presented paresthesias of her left foot. An electrophysiology study was conducted and showed an electroneurographic pattern of conduction block at the left distal posterior tibial nerve, compatible with peripheral nervous system vasculitis. Laboratory tests showed mild leukocytosis with a small leftward shift, erythrocyte sedimentation rate (ESR) of 97mm (normal values up to 25mm) and C reactive protein (CRP) of 1.22mg/dl (normal to 0.5mg/dl) with negative antineutrophil cytoplasm antibodies (ANCAS). A cerebrospinal fluid study showed pleocytes and lymphocytes. The first clinical suspicion was polyarteritis nodosa (PAN), so we decided to perform a muscle and sural nerve biopsies that were nonspecific. Because of the history of sinusitis, the diagnosis of microscopic polyangiitis or Wegener's granulomatosis (WG) had to be ruled out, which we did after a biopsy of the affected mucosa. At all times peripheral pulses remained present and symmetrical, with no significant differences in BP between the 2 arms; there were no murmurs on auscultation of the aorta or subclavian arteries and the patient did not complain of fatigue or discomfort and presented no claudication. Within 10 days of admission she presented occipital and frontal headache with photophobia and little improvement with analgesic treatment as well as hypertension (160/95mmHg) which responded with the administration of ACE inhibitors. Keeping with our clinical suspicion of vasculitis we conducted a magnetic resonance angiography (MRA) of the aorta (Ao), which showed no abnormalities, a brain MRI which confirmed the existence of pachymeningitis and a thoracoabdominal CT that showed a small infrarenal aneurysm cm2 diameter. Finally, we performed a PET-CT which showed hypermetabolic lesions of the pulmonary bifurcation and the abdominal Ao wall (Fig. 1), which along with gender, age, involvement of large vessels (Ao and pulmonary), the presence of aneurysms, the negativity of ANCAS, the result of the biopsy and exclusion of PAN and GW, very likely led the diagnosis of Takayasu's arteritis (TA) with the added difficulty of performing a biopsy of the affected area.
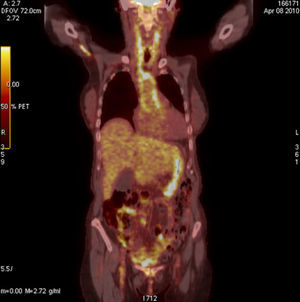
Case 2This case was a 74-year-old woman with pain and weakness of the shoulders and hips, with morning stiffness of more than 1h and elevated acute phase reactants. Suspecting polymyalgia rheumatica (PR) we administered 30mg/day of prednisone with initial improvement, but rapid recurrence of symptoms and deterioration in the laboratory tests, with a hemoglobin of 8mg/dl, CRP 19mg/dl and an ESR of 120mm in the first hour. The patient reported no headache, jaw claudication or tenderness on the temporal artery and peripheral pulses were normal. Suspecting a neoplasia we requested tumor markers, a thoracoabdominal CT, gastroscopy and colonoscopy, all with normal results; the study was completed, finally, with the performance of a PET-CT (Fig. 2) which evidenced a vasculitic process in the Ao, innominate, carotid and subclavian arteries. Given the strong suspicion of GCA we performed a temporal artery biops, which confirmed the diagnosis.
DiscussionGCA is a granulomatous polyarteritis which affects arteries of medium and large caliber, with a predilection for the cranial branches of the arteries originating from the aortic arch, although in about 15% it may affect the entire Ao and its main branches.1 Its etiology remains unknown. Diagnosis is histological and done by finding a granulomatous inflammation in which giant cells are located between the intima and media. The lesions and the evolution of focal inflammation lead to a wall thickening and fibrosis with stenosis and subsequent occurrence of ischemic events. Among the most common symptoms found: headache, malaise, fever and myalgia.2
TA is a LVV which mainly affects the Ao and its main branches such as coronary or pulmonary arteries. It predominates in young women. It presents an early stage where the symptoms are nonspecific, such as fever, and late-stage symptoms associated with ischemic events such as arm claudication, low pulses or high blood pressure. Histology is shared with GCA, with some authors arguing that this may be the same disease.3
In 1990 the American College of Rheumatology established a series of clinical, radiological and histological classification criteria for LVV, with a sensitivity of 93.5% and a specificity of 90.5% for GCA,4 and 91.2% and 97.8% respectively for TA, in patients with a positive biopsy.4 These criteria are still applied today, although approximately 40% and 70% of these vasculitis do not meet any of these criteria for classification and appear with nonspecific clinical signs and symptoms.5
Another confounding factor are markers of disease activity. Thus, 70% of patients with active disease have elevated ESR, while the rest may remain normal, as has later been revealed by imaging techniques.6
The temporal artery biopsy, in the case of GCA, has emerged as the diagnostic procedure of choice, as this cannot be done in the case of Takayasu's arteritis because of the location of the affected arteries, considering arteriography as the diagnostic gold standard. This is the most reliable technique for assessing stenotic vascular disease, aneurysms and the state of the collateral circulation and allows for endovascular treatment which be performed simultaneously, but raises the serious drawback of a diagnosis in later stages of the disease, when complications have developed.7
In recent years other imaging techniques have been investigated that allow us to identify and assess the arterial wall, among which Doppler ultrasound of the temporal artery. The presence of a hypoechoic halo around the arterial lumen of the inflamed temporal artery has been described, and since then, there have been several studies that have confirmed its existence, specifically considering GCA and suggesting that the practice of color Doppler ultrasound improves the performance of arterial biopsy diagnosis, and may even prevent its practice. Its use is controversial because it is a technique that depends on user experience.8,9
CT allows the study of great area of the body in a short period of time, leading to a good assessment of the wall and the vessel lumen, and is a good technique for detecting aneurysms, although it does not detect inflammation in the early phase of the vasculitis.
Today, MRI is the technique that provides higher resolution. In the case of inflammation of the vascular wall it may detect abnormal uptake in sequences obtained after administration of gadolinium in both T1 and LGE sequences. It is the technique of choice for studying the Ao, and to a lesser extent, its large branches, allowing for the assessment of the morphology and swelling thereof. Its main drawback is that it requires long scan times for small vascular territories and the use of gadolinium contrast for higher resolution.
Finally, positron emission tomography (PET) is based on the distribution of glucose analog, radiolabeled deoxyglucose which emits positrons -18-fluoro-, administered intravenously and distributed through the organs following the metabolic pathway of glucose uptake. PET does not provide a good spatial resolution, so to overcome this limitation, it is complemented by CT, and by overlaying the 2 images a combination of precise anatomic localization and functional status of metabolically active lesions is achieved in a single image, a PET-CT.10 Glucose is stored not only in the vasculitic vessels but is captured by atheroma plaques, where there is inflammation, which reduces the specificity of the test, although in the thoracic Ao the intensity and pattern of uptake enables differentiation, using the Meller visual scale (Table 1), which compares the vascular uptake of 18F-FDG with the accumulation thereof in the liver, demonstrating its later validity to assess the degree of inflammation and the activity of the disease.11
Currently, several studies show that PET-CT is effective in the detection of large vessel vasculitis and evaluation of the extent of disease, with a sensitivity which ranges from 77% to 100% and with 89% to 100% specificity, making it an important aid in the diagnosis of patients with fever of unknown origin.12
ConclusionsTA and GCA are LVV that require histopathological confirmation. In the case of TA, due to the location of the involved arteries, arterial biopsy is often not an option, and in the case of GCA, biopsy sometimes does not provide a high diagnostic yield due to the involvement of irregular affection of vessels or the use of glucocorticoids prior to its execution. In both cases imaging techniques may prove highly profitable for diagnostic confirmation. In recent years, PET-CT gained increasing importance as a diagnostic technique, being non-invasive and having a superior sensitivity to magnetic resonance angiography. It detects more affected regions than MRI and at an earlier stage.
However, the main indication for PET-CT, at this time, in the initial diagnosis of arteritis of large vessels would be confirmation of vascular inflammatory disease when the clinical presentation and the findings of other imaging techniques provide nonspecific information.
Ethical ResponsibilitiesProtection of People and AnimalsThe authors state that no experiments were performed on humans or animals.
Data ConfidentialityThe authors declare that they have followed the protocols of their workplace on the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to Privacy and Informed ConsentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Pacheco Castellanos MC, et al. Diagnóstico precoz de las vasculitis de grandes vasos. Utilidad de la tomografía por emisión de positrones con la tomografía axial computarizada. Reumatol Clin. 2013;9:65–68.