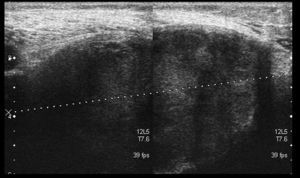
We present the case of an 83-year-old male patient with osteoarthritis, who came to the emergency room due to acute inflammation of the leg simulating DVT. On physical examination, there was a mass of elastic consistency, non-pulsatile, painful, in the popliteal fossa, extending to the leg (Fig. 1). The differential diagnosis was made with Baker cyst. The patient underwent, as a technique of choice, an ultrasound. The color Doppler mode showed patency of the deep venous system. Musculoskeletal ultrasound evidenced a well-defined collection, adjacent to the medial gastrocnemius muscle belly, full of vague echoes predominantly of low amplitude (Fig. 2) Despite being frequent, the size of the tumor made ultrasound insufficient and we decided to perform specific knee MRI with T1 potentiated sequences, T2* sequences (Figs. 3–5) and, after administration of intravenous contrast, we confirmed the existence of giant popliteal cyst of 17cm×9cm. The patient was treated conservatively, using, in the first place, nonsteroidal anti-inflammatory drugs, with clinical improvement and asymptomatic after the first 6 months. For this reason, along with the age of the patient and in spite of the cyst barely changing its size, surgical treatment has so far been dismissed.
Complicated Baker's cyst is a very common entity. The prevalence increases with age. However, we have only found one published case1 of similar dimensions. Cysts containing over150ml produce neurovascular compression phenomena at the popliteal level, being associated with2,3 other conditions, such as rheumatoid arthritis.4,5 Both for possessing a broad spectrum of presentations and the characteristics of the synovial liquid seen by ultrasound sometimes makes this a diagnostic challenge.6,7
Ethical ResponsibilitiesProtection of people and animalsThe authors declare this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no conflict of interest to state.
Please cite this article as: Alonso-Gómez N, Pérez-Piqueras A, Martínez-Izquierdo A, Sáinz-González F. Quiste de Baker gigante. Diagnóstico diferencial de trombosis venosa profunda. Reumatol Clin. 2015;11:179–181.