Heterotopic ossification is an uncommon disorder that consists of deposition of ectopic bone outside the extraskeletal tissues. In the skin, it can be primary, in association with genetic syndromes, or be secondary to different disorders. The latter include subcutaneous ossification of the legs in chronic venous insufficiency, an infrequent and unrecognised complication. We report the case of a patient with subcutaneous ossification of both legs secondary to venous insufficiency and review the literature.
La osificación heterotópica es un trastorno infrecuente que consiste en el depósito de tejido óseo extraesquelético. En la piel, puede ser primario, en el contexto de síndromes genéticos, o secundario a trastornos muy diversos. Dentro de las formas secundarias, la osificación subcutánea de las piernas por insuficiencia venosa crónica es una complicación infrecuente y poco reportada. Presentamos un paciente con osificación subcutánea de las piernas secundaria a insuficiencia venosa y revisamos la literatura.
Heterotopic ossification (HO) consists of the extra-skeletal and cutaneous formation of bone, and it is due to multiple causes. We present the case of subcutaneous HO (SCHO) of the legs, in connection with chronic venous insufficiency (CVI).
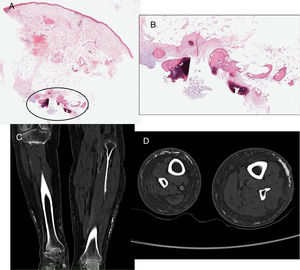
Clinical observationA 66 year-old male with a history of years with auricular fibrillation, ischaemic ictus with right hemiplegia, and CVI with left deep vein thrombosis in 2005. He visited due to gradual and slightly painful hardening of the legs during 3 months. Palpation found subcutaneous stony consistency in the posterior and lateral regions of both lower thirds of the legs, chiefly the left one. X-rays showed subcutaneous reticulated opacities with bone density. A biopsy was performed, finding bony consistency when cutting subcutaneously, with ossification in the deep dermis and fat (Fig. 1, images A and B). The analytical results (including phosphor-calcium metabolism), thoracic X-ray and abdominal ultrasound scan were all normal. Bone scintigraphy showed hyperabsorption in the soft parts of the legs, fundamentally the left leg, while CAT showed lineal plaques with a trabecular/reticular appearance in the subcutaneous regions of both legs (Fig. 1, images C and D). Given the mild symptoms, the patient did not request treatment and was lost during follow-up.
Biopsy. (A) Panoramic view of atrophic epidermis and telangiectasias in dermis, with an area of deep and fatty dermis ossification (circled) (haematoxylin–eosin 4×). (B) This area in greater detail, in deep dermis and subcutaneous cellular tissue: bone trabeculas enclosing adipose tissue (haematoxylin–eosin 40×). (C and D) CAT without contrast: lineal bone density plaques, trabecular/reticular in appearance in the subcutaneous cellular tissue along the perimeter of both legs, more evident in the left leg, fundamentally on the exterior face. Asymmetrical arterial atheromatosis in the size on the legs is due to previous right hemiplegia.
Cutaneous HO has a wide range of causes. The primary forms are very rare, and they appear in hereditary syndromes and different types of osteoma cutis. The great majority of SCHO or ossifying paniculitis are secondary to heterogeneous pre-existing lesions, including calcifications. The association of SCHO and CVI was described by Lippman in 1957 in 23 patients1 followed by 37 others, concluding that it would occur in 10% of CVI.2 Isolated cases have been published subsequently,3–6 and the few reviews which exist refer to CVI and subcutaneous dystrophic calcification using radiological findings.7,8 In one of these, calcification occurred in 17.5% of 40 cases with CVI7; in another publication calcification was found in 65% of 20 cases of long-term severe CVI, and SCHO was found in 20% of patients who had received biopsies.8 The incidence of SCHO in CVI is unknown, although it may be under-diagnosed, and it may be found by chance. It mainly affects women over the age of 50 years old and obese, with long-term CVI. It manifests with hard uni- or bilateral subcutaneous nodules and plaque and it is generally asymptomatic.2–8 Nevertheless, in advanced cases it may cause pain, joint deformation and nerve entrapment.9 The underlying skin may be normal or show signs of CVI, venous ulcers and, more rarely, livedo racemosa,6 and it does not involve the fascia or muscles. Analytic study including phosphorus-calcium metabolism is normal. Biopsy, which is the test of choice, is similar to other cutaneous HO, showing bone deposits in the dermis and fat. Radiography shows diffuse or reticulated subcutaneous opacities, affecting the leg perimeter, and it may be associated with periostitis due to CVI.10 Ultrasound scan is a fast, accessible and economical technique that is considered to be suitable for the early diagnosis of calcification and ossification, as simple X-ray may not shows alterations until 10–14 days have transpired.11 The ossification shows hyperechogenic images with a posterior acoustic shadow artefact in the subcutaneous layer, while calcifications are less echogenic.6,9 Bone scintigraphy too is highly sensitive in early diagnosis, although this is not the case for CAT or magnetic resonance imaging, which make it possible to evaluate extension.
The pathogenesis of SCHO in CVI is unknown, and it is not always preceded by calcification. Oedema and/or persistent inflammation would lead to cellular necrosis with the liberation of cells and inflammatory mediators, causing ossification. It has also been hypothesised that pluripotent mesenchymal cells or adipocytes themselves turn into bone, or that latent bone progenitors in the involved and surrounding tissue, or that even circulating cells differentiate into osteoblasts.6,8
The early detection of calcification and SCHO in CVI is important to halt progression, as there is no effective treatment and debridement or excision is recommended, if possible. In other cases of SCHO diltiazem, probenecid, minocycline, aluminium hydroxide and bisphosphonates have been used with favourable results; sodium thiosulfate may be an option for dystrophic calcification.9
ConclusionsWe present a new case of SCHO in association with long-term CVI; it is possible that immobility due to right hemiplegia (worsening the CVI) and chiefly left TVP have influenced its appearance. Although biopsy is the standard test, ultrasound scan seems to the technique of choice for early diagnosis.9
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Arpa M, Flores-Terry MA, Franco-Muñoz M, Villasanti-Rivas N, González-Ruiz L, Banegas-Illescas ME. Osificación heterotópica de las piernas en un varón. Reumatol Clin. 2020;16:300–302.