This article reviews the underlying anatomy of trigger finger and thumb (fibrous digital pulleys, sesamoid bones), flexor tenosynovitis, de Quervain's syndrome, Dupuytren's contracture, some hand deformities in rheumatoid arthritis, the carpal tunnel syndrome and the ulnar nerve compression at Guyon's canal. Some important syndromes and structures have not been included but such are the nature of these seminars. Rather than being complete, we aim at creating a system in which clinical cases are used to highlight the pertinent anatomy and, in the most important part of the seminar, these pertinent items are demonstrated by cross examination of participants and teachers. Self learning is critical for generating interest and expanding knowledge of clinical anatomy. Just look at your own hand in various positions, move it, feel it, feel also your forearms while you move the fingers, do this repeatedly and inquisitively and after a few tries you will have developed not only a taste, but also a lifelong interest in clinical anatomy.
En este artículo revisa la anatomía subyacente en el dedo en gatillo y el pulgar en gatillo (poleas digitales fibrosas, huesos sesamoideos), tenosinovitis flexora, síndrome de De Quervain, contractura de Dupuytren, algunas deformidades de la mano en la artritis reumatoide, el síndrome del túnel carpiano y la compresión del nervio cubital en el canal de Guyon. Debido a la naturaleza de estos seminarios, no se han incluido algunos síndromes importantes y estructuras. Más que ser exhaustivos, nuestro objetivo es crear un sistema en el que los casos clínicos se utilizan para resaltar la anatomía pertinente y, en la parte más importante del seminario, estos elementos se muestran a partir de una examen cruzado entre participantes y profesores. El autoaprendizaje es fundamental para generar interés y ampliar el conocimiento de la anatomía clínica. Basta con mirarse las propias manos en distintas posturas, moverlas, sentirlas; sientan también el antebrazo mientras mueven los dedos, háganlo varias veces, con espiritu de indagación, y tras unos pocos intentos no solo habrán adquirido un gusto, sino un interés por la anatomía clínica.
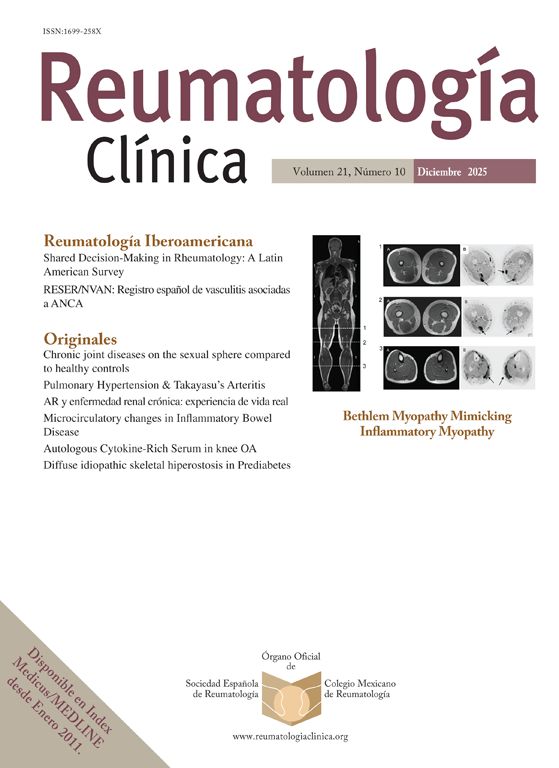
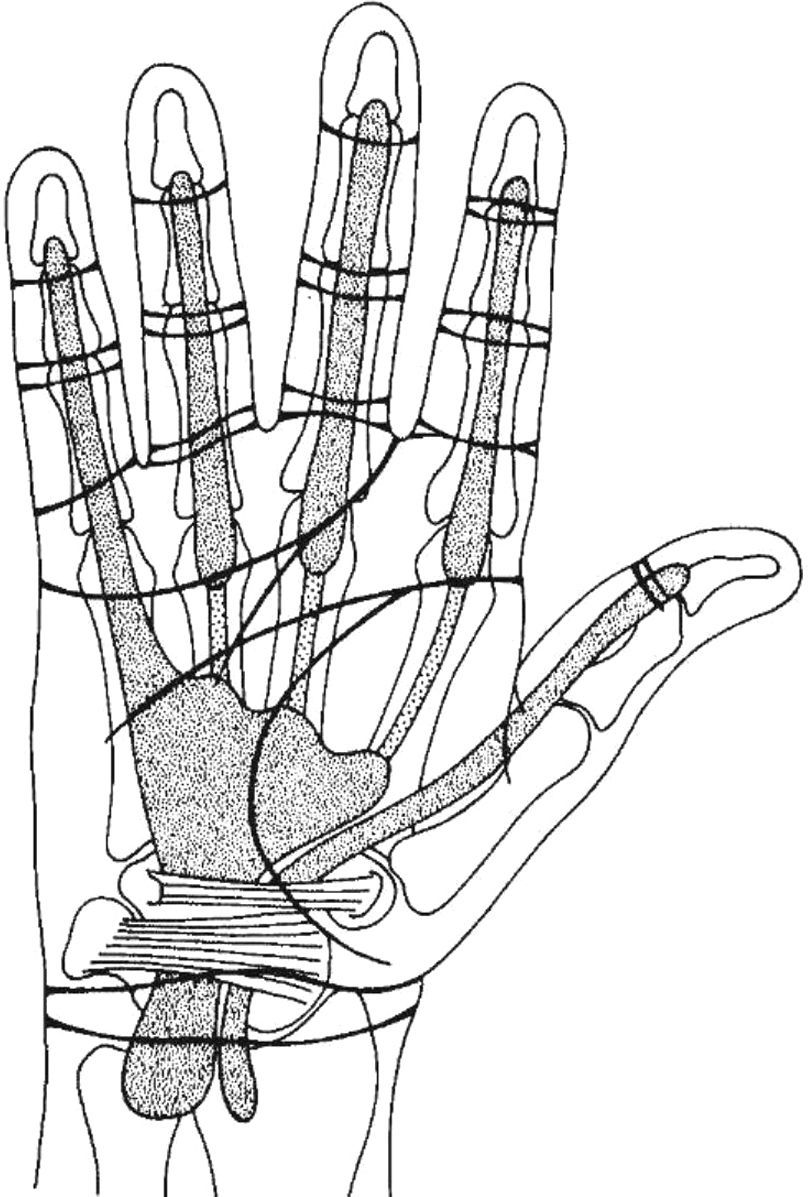
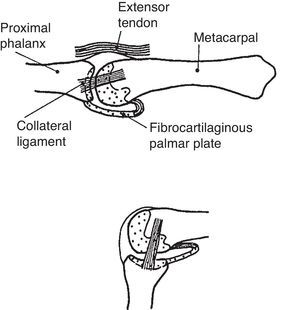
The hand is arranged along 5 rays that in full extension spread apart and in full flexion come together without overlaps, except the thumb, and with an admirable surface economy. The basis of this arrangement is a fixed dorsal convexity of the distal carpal row that translates to the metacarpals and from these to the phalanges. In addition, grasp activities depend on a fixed ratio of 1:1.6 for each segment of a digital ray as compared to its proximal fellow. This provides a perfect adaptability of the fingers for all diameters of an object.1 For the fingers 2–5 passive lateral motions are possible having the hand flat. However, progressive flexion of the MCP causes progressive loss of this motion so that at 90 degrees flexion lateral motions are no longer possible. This is due to the eccentricity of the medial and lateral collateral ligaments of the MCP joint (Fig. 1). In rheumatoid arthritis, chronic inflammation may damage the capsular tissues resulting in an unstable finger at full flexion of the MCP joint. The thumb MCP has no lateral motion in full extension and full flexion but is more than rewarded by the CMC (trapezium-metacarpal) motion that allows a boom-like swing of the metacarpal while preserving the flexion and extension movements of the thumb. Additionally, the thumb CMC exhibits a counter-clockwise rotation – as looked from proximal to distal – which makes the alignment of the thumb nail to the finger nails progressively more perfect as the little finger is approached. A disservice to the hand has been to depict it as a flat structure, thumb out, as in the dissection table. In the real state, as we all know, the wrist is slightly dorsiflexed, the MCFs and the IFs slightly flexed, and the 1st web at about 90 degrees to the other web spaces. Strength and precision are attributes of the human hand. Strength is delivered primarily by the long flexors and extensors, but a hand without intrinsic muscles, while maintaining its strength, is only useful as a hook.2 The wrist, which is part of the hand, allows the hand to work in extension, in flexion and in ulnar and radial deviation. But the all-important forearm pronation and supination are provided by the distal radioulnar joint, the humeroradial and, to a lesser extent, the humeroulnar joints. The neutral position of the wrist is thumb up. In pronation, or palm down, the distal ulnar head becomes more prominent while the radius, with the triangular ligament attached, has fallen palm down. This makes the extensor carpi ulnaris (ECU) tendon to appear in the ulnarmost portion of the wrist. Once again thumb up, the ECU tendon is felt to overlap dorsally the distal ulnar head. Now in supination, or palm up, the ECU tendon appears between the distal ulnar head and the radius. The cases that follow highlight clinically relevant aspects of the hand that are only rarely discussed during rheumatology training.
Upper panel. MCP joint showing the metacarpophalangeal joint (MCP) in neutral. The collateral ligament is relaxed. Note tibrocartilaginous palmar plate in the palmar aspect of the joint. Lower panel. The lateral collateral ligament becomes taut in flexion. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.16, with permission.
Patient 1. Trigger finger “A 56 year-old man has a trigger finger”
Patient 2. Trigger thumb “A 50 year-old woman has a trigger thumb”
Patient 3. Rheumatoid flexor tenosynovitis “A 32 year-old woman with insufficiently treated rheumatoid arthritis has pain and swelling in the left index finger which cannot actively reach the palm”
Cases 1, 2 and 3 focus our attention on the digital flexor sheaths, which comprise fibrous and synovial structures, and highlight the important role of the palmar creases both in diagnosis and as a guide for corticosteroid injections in flexor tenosynovial conditions.
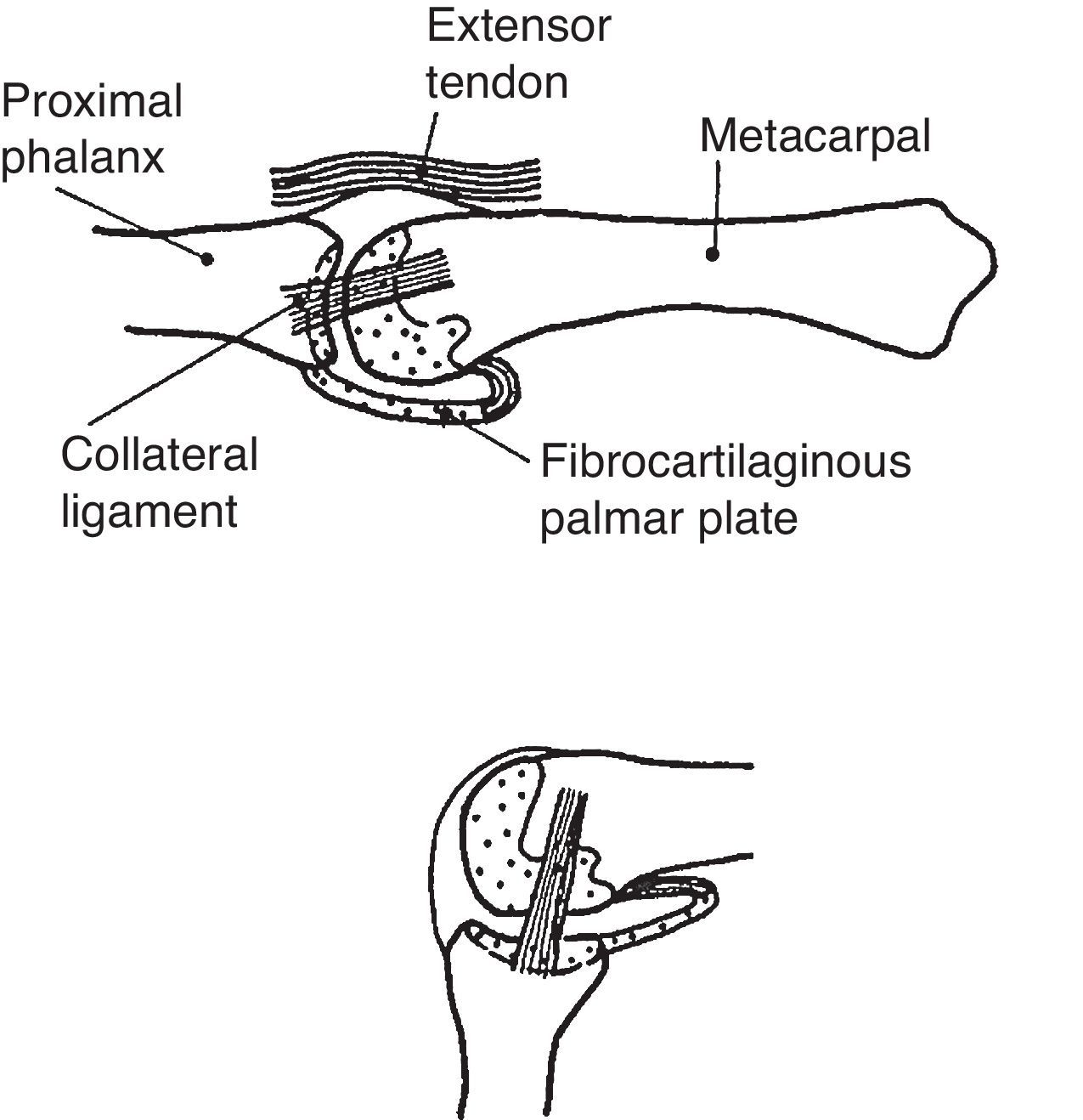
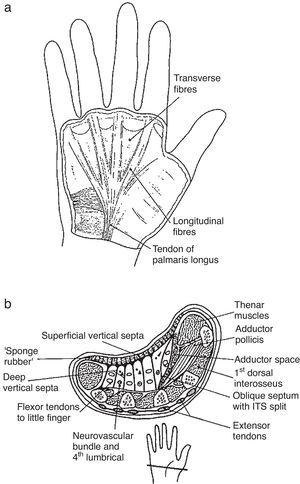
Palmar FasciaThe palmar fascia is a triangle shaped, tough sheet of connective tissue placed deep to the skin in the palm of the hand (Fig. 2).3 Ulnarly it is limited by the hypothenar muscles and laterally by the thenar muscles. Skin displacement during grip is prevented by fibrovascular septae with loculated fat in between that link the skin to the palmar fascia. This arrangement resembles closely to the plantar fat pad.4 In addition, seven sagittal ligaments join the palmar fascia to the deep metacarpals fascia and result in 8 tunnels, 4 for the flexor tendons and 4 for the lumbricals5 distal to the central compartment of the hand. The superficial fibers of the palmar fascia fan out from palmaris longus and continue in the fingers as the pretendinous band, the spiral fibers and the lateral digital sheet. All of these structures, as well as the vertical septae that link the palmar fascia to the skin, are important in the pathogenesis of Dupuytren's contracture.6,7 The deep fibers are generally transverse and can be considered an extension of the transverse carpal ligament into the palm. The fascia that covers the thenar and hypothenar muscles,8,9 in contrast to the thick and complex palmar fascia, is thin and adherent to muscle. There is a superficial, transverse muscle that can be seen to bulge in the hypothenar eminence which originates in the palmar fascia and inserts in the skin. This is palmaris brevis.10 The function of this peculiar muscle is conjectural. On the one hand it deepens the cupping of the hand when we drink from it. Also, it contracts synergistically then the 5th MCP is flexed with the PIP and the DIP in extension and during the abduction of the 5th digit.
(a) The palmar fascia. The longitudinal fibers derive from palmaris longus tendon. Note the transverse fibers of palmaris brevis, a subcutaneous musle at the hypothenar eminence. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.16, with permission. (b) A transverse section of the hand. The palmar fascia is located near the palmar surface. It is connected to the dermis by fibrous strands that loculate tiny fat lobules. Septae connect the deep aspect of the palmar fascia to the deep fascia that overlies the metacarpals and the interosseous muscles (the insert shows the site of the section). From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.16, with permission.
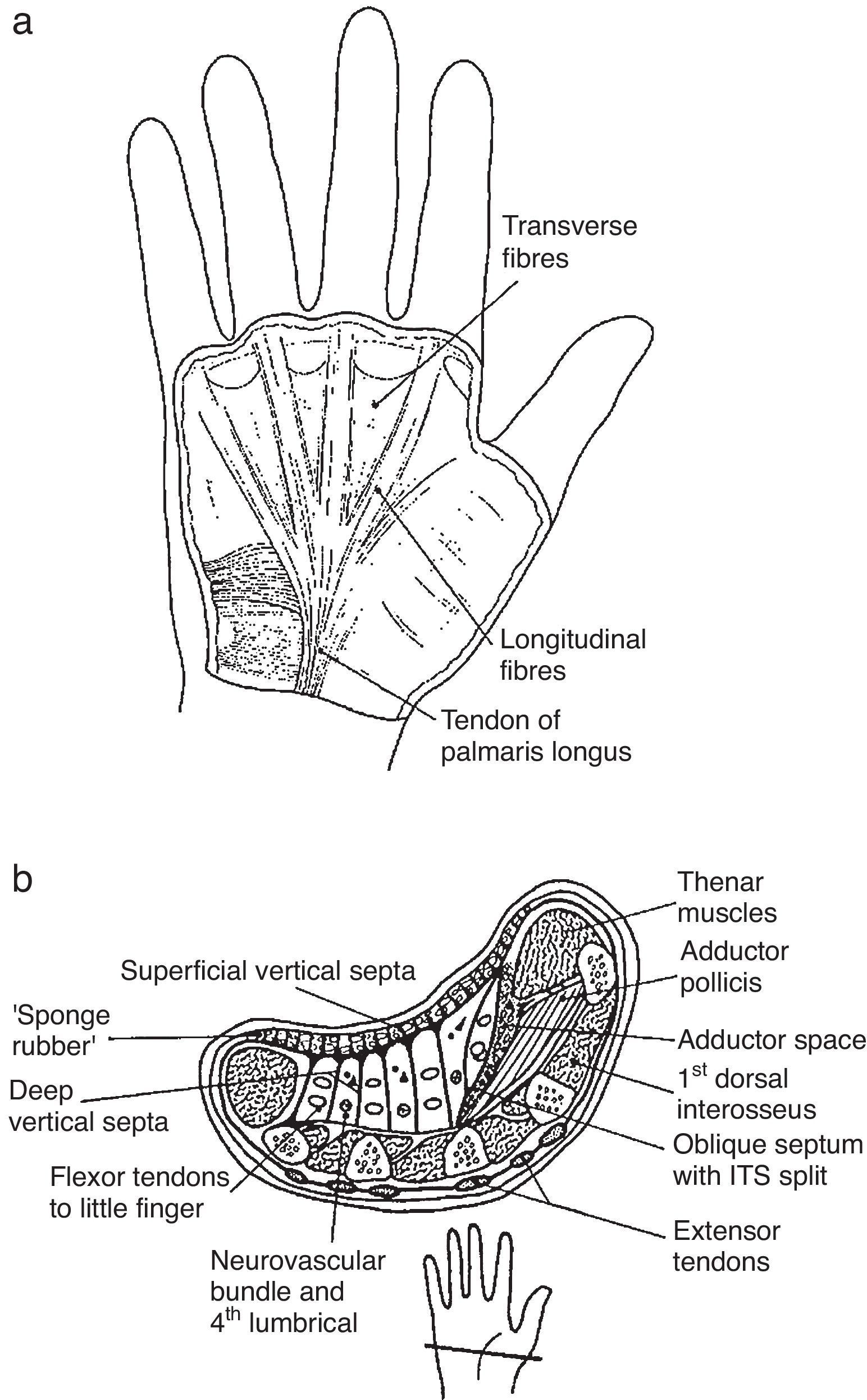
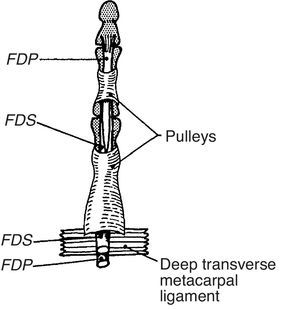
Participants will have traced on their hands the full length of the digital flexor sheaths. They should understand the role of the restraining fibrous structures that maintain the tendons in close vicinity to bone and prevent bowstringing during flexion of the digits, the anular and cruciform pulleys.11 Although pulleys are discontinuous when the fingers are extended, with synovial tissue in between, they come together and form an almost continuous tube when the fingers are flexed (Fig. 3). The A1 pulley, being the most proximal and therefore the one that deflects the flexor tendons is the one that stands the greatest tendon/pulley pressures. Resulting swelling and chondroid changes in both the pulley and the tendon lead to nodule formation and the trigger phenomenon.12 Although patients sometimes perceive the entrapment elsewhere the trigger phenomenon is an A1 pulley affair. Because finger flexor muscles are stronger than extensors trigger fingers are usually caught in flexion. A permanent flexor deformity may result in late, unrelieved cases. An additional restraining fibrous structure is the palmar aponeurosis pulley which is comprised of transverse fibers of the palmar fascia. This restraint, which is of marginal importance in normals, helps at preventing bowstringing when the A1 or the A2 pulley is cut. The thumb has 3 anular pulleys and an oblique pulley. The thumb A1 pulley, as in the fingers, overlaps the MCP joint.13 The correct diagnosis in our patients is a trigger finger in Patient 1 and a trigger thumb in Patient 2. We would like to add that when the MCP joint ligaments are weakened, as in rheumatoid arthritis, the pull of the A1 pulley on the palmar plate and the base of the proximal phalanx in forceful finger flexion may be such as to cause palmar subluxation of the joint.
This is a simplified rendition of the fibrous digital pulleys. The proximal pulley, A1, inserts in the palmar plate and in the transverse metacarpal ligament that binds neighboring palmar plates. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.22, with permission.
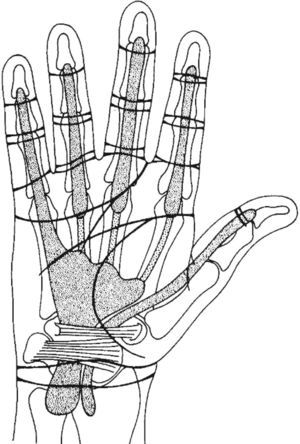
The proximal extension of the synovial flexor tendon sheaths, which are contained in the digital flexor sheaths, will now be shown (Fig. 4). It is often surprising that the synovial sheath of the little finger connects with the ulnar bursa, a synovial expansion deep in the palm, in over 70% of cases.14 This three-layered structure, which provides a gliding surface between the long and short fingers flexors, as well as a gliding surface deep and superficial to these tendons, extends into the carpal tunnel and for about 2.5cm into the distal forearm. The synovial sheath of the long flexor of the thumb, also known as radial bursa, also traverses the palm and the carpal tunnel and extends into the distal forearm. In contrast, the synovial sheaths of the flexor tendons 2–4 end in the palmar space just short of the A1 pulley at the neck of the metacarpal bones. In Patient 3 the diagnosis is a rheumatoid flexor tenosynovitis. In this condition the swelling, which is due to both tenosynovial proliferation and effusion, involves the finger and the distal portion of the palm. Rheumatoid tenosynovitis may present few local findings but it must be suspected when a rheumatoid patient cannot actively make a full fist but passively the affected fingers can be painlessly flexed. The swelling tends to be diffuse and distend, as in our patient, the palmar cul-de-sac. Needless to say, these patients greatly improve with a well-placed tenosynovial corticosteroid injection.
This figure shows the relationship between the transverse palmar creases and the flexor synovial sheaths. Note that for the digits 2,3,4 the synovial sheaths end near the transverse creases. For the thumb and the small finger the sheaths extend to the distal forearm. The expansion of the latter in the mid palm is the ulnar bursa, a synovial structure extends to the carpal tunnel and the distal forearm. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.24, with permission.
The great British anatomist Frederick Wood Jones stated that creases are the joints of the skin.15 Looking at the palm there are 2 transverse creases, the distal and the proximal (Fig. 4). The distal crease, arising in the ulnar side of the hand bends distally and ends in the 2nd web space. The proximal crease begins with the longitudinal thenar crease in the 1st web space and ends short of the hypothenar eminence. An amazing phenomenon occurs when the straight fingers are bent 90 degrees at the MCP joints. Both the distal and the proximal crease come together in a continuous transverse crease. A cord placed in this crease indicates the proximal edge of the A1 pulley for the fingers 2–5. Deeper structures overlied by this cord include the flexor tendons, the palmar plates, the deep intermetacarpal ligaments that link neighboring palmar plates, and the MCP joints. Look at this region, known as region V or metacarpophalangeal by hand surgeons, from the palm, the radial side and the dorsum to get an idea of its complexity. More distally in the palmar side there is a crease where the finger appears to arise, the proximal digital crease. However, a cord placed around the finger at this crease, looked from the dorsum, crosses the mid portion of the proximal phalanx. Finally, a cord placed around the mid and the distal digital creases roughly overlaps the PIP and the DIP joints, respectively.
The Palmar Plates and the Deep Intermetacarpal LigamentThe palmar plates are thick and dense plates – whether they are fibrocartilaginous or not is in debate – that reinforce the volar aspect of the MCP joints (Fig. 1). While distally the palmar plates are firmly attached to the proximal phalanx, proximally they become a thin, membranous capsule.16,17 Each palmar plate is connected to the neighboring palmar plates by the deep intermetacarpal ligament. Also, sagittal bands (SB) connect the extensor tendon to the edges of the palmar plates, which also give insertion to the accessory MCP lateral collateral ligament and the A1 pulley. Thus, the palmar plates provide a true anchoring system to the fibrous skeleton of the MCP region. Together, the SBs and the palmar plate form a closed cylindrical tube that surrounds the metacarpal head. It is considered that the SBs represent the main stabilizer of the extensor tendon at the MCP joint.18 Damage of the radial sagittal fibers is one of the factors leading to ulnar deviation in rheumatoid arthritis. Palmar plates with a similar phalangeal attachment are also present in the interphalangeal joints.19
Corticosteroid Infiltration in Trigger Finger/Thumb and TenosynovitisIn Patient 1 the injecting needle is placed just distal to the proximal transverse crease for the index, between the proximal and distal creases for the middle finger and just distal to the distal crease for the anular and the little finger. There is no need to place the steroid within the synovial sheath in this condition. Indeed, extrasynovial injections appear to work better. The injection for the trigger thumb is quite different and the thumb sesamoids are used as a landmark. The thumb has 2 sesamoid bones which are easily palpable at the base of the thumb on the flexor side. These tiny bones transmit force from the abductor pollicis and the flexor pollicis brevis to the proximal phalanx via the volar plate. They also guide the flexor pollicis longus tendon that lies between them.20 The thumb sesamoids vary in size among people and one may be larger than the other. The sesamoids area is normally tender to palpation. The injecting needle is aimed at the sesamoids (Fig. 5). In Patient 3, with a diagnosis of rheumatoid flexor tenosynovitis, it is quite important to place the steroid within the sheath because synovial tissue is interspersed between pulleys and at both ends of the tube. An intrasynovial injection is felt by the patient as fluid extending distally along the palmar aspect of the finger.
Practical Review of Some Palmar Structures- •
Palmar creases
- •
Dorsal projection of proximal digital crease
- •
Palmaris brevis muscle
- •
Palmar fascia and its longitudinal and transverse components (superficial transverse metacarpal ligament, longitudinal and transverse fascicles)
- •
Digital pulleys
- •
Flexor synovial sheaths
- •
Flexor tendons
- •
Palmar plates, approximate position
- •
Thumb sesamoids
- •
Tendons that are contained in the carpal tunnel
Patient 4. Interosseous muscle function “A fellow is asked during the certifying examination: Which muscles separate the fingers and which muscles bring them together? He pales and looks at the examiner in disbelief”.
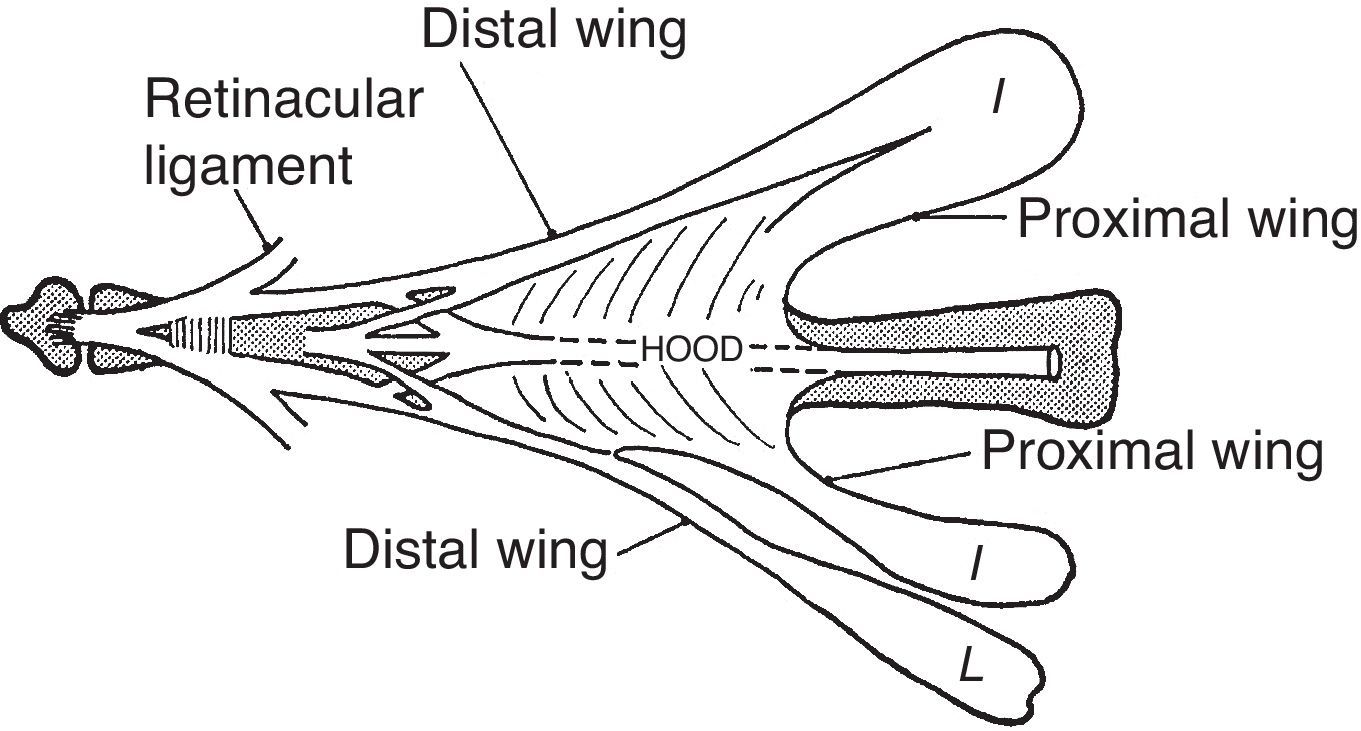
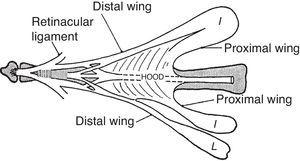
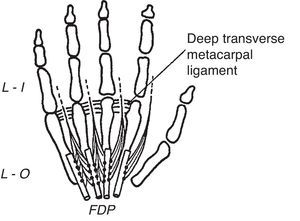
If we overstretch the fingers the extensor tendons, prominent in the dorsum of the hand, are seen to disappear at the fingers. One of the reasons of this phenomenon is that the extensor tendon itself is anchored by sagittal fibers to the palmar cartilaginous plate that reinforces the MCP on the palmar side.21,22 A second reason is that the extensor tendon becomes embedded in the dorsal digital expansion.23–25 The dorsal digital expansion may be viewed as an isosceles triangle applied on the proximal phalanx (Fig. 6). The expansion incorporates the central tendon fibers destined to the base of the middle phalanx. In addition, it contains two previously separated extensor tendon contingents, the radial and the ulnar lateral bands, that join together prior to their destination at the base of the distal phalanx. Also, the interossei muscles as well as the lumbricals, past the deep transverse metacarpal ligament that separates them, run toward the angles of the extensor lamina and once incorporated to this structure, extend along the lateral sides in the middle and lateral conjoined tendons.21 In finger flexion the lateral bands slide palmarly over the PIP joint while in extension the tendon pull brings them closer together as to better extend the DIP joint.26 Is it possible to palpate the extensor lamina? Yes, by 2-finger palpation, one radial and one ulnar, on the dorsolateral aspect of the proximal phalanx during flexion-extension movements. Is it important? Yes, to get a dynamic idea of what it is going on.
The extensor lamina is a triangular fibrous sheath in the dorsum of the proximal phalanx. The extensor tendon is incorporated into this lamina and the interosseous muscles and the lumbrical muscles attach to its sides. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.54, with permission.
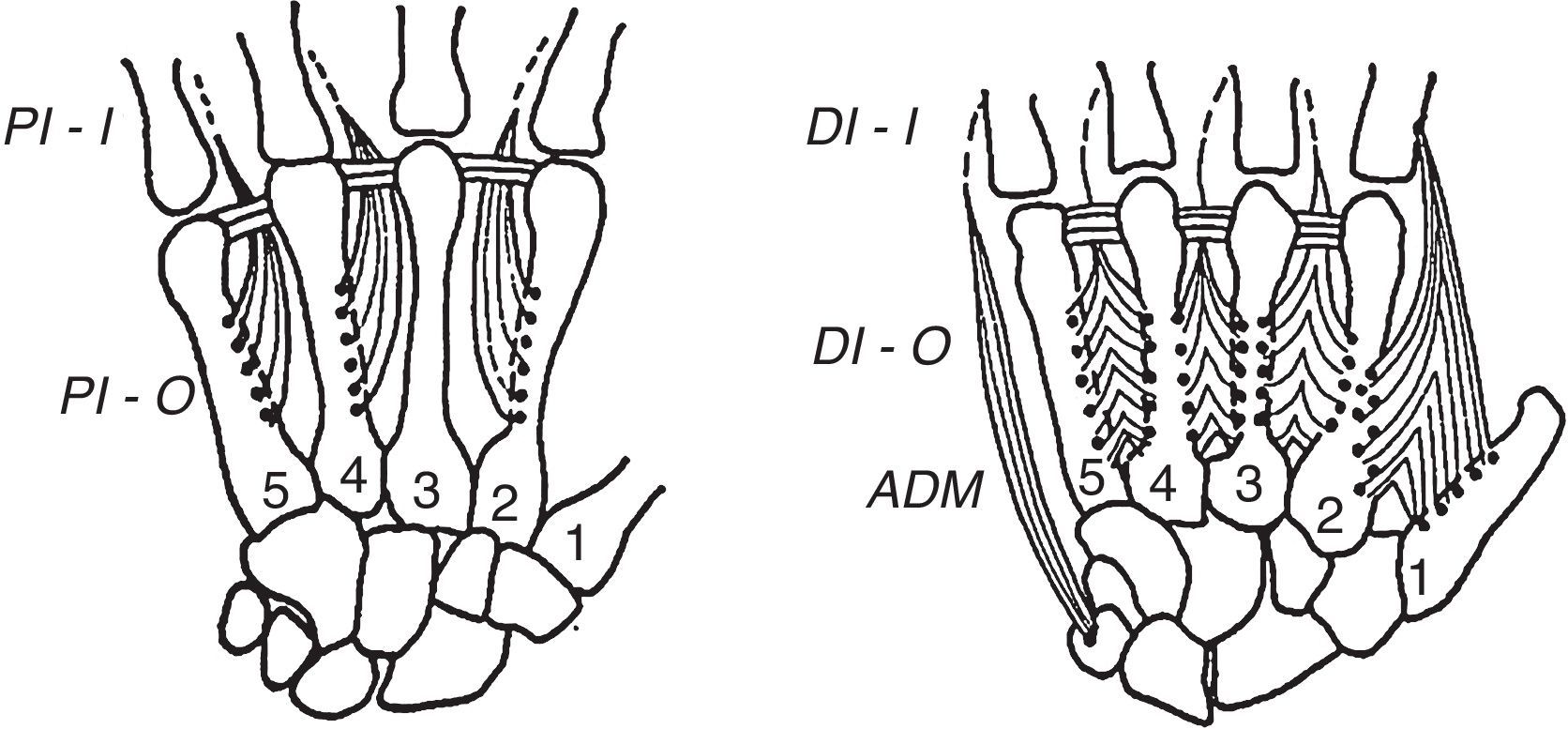
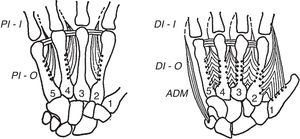
The interosseal muscles, both the dorsal and the palmar (Fig. 7), have their origin in the metacarpals and insert at the corners of the extensor lamina. In addition, the dorsal interossei have a point of insertion in the proximal phalanx.27,28 Both sets of muscles run dorsal to de deep intermetacarpal ligament. The longitudinal axis of the hand is comprised of the long finger and the 3rd metacarpal. Proof of this is that the 3erd digit stays still when the fingers are spread apart and when they are brought back together. While the dorsal interosseus tendons are so placed as to separate the index and the anular away from the long finger, by having 2 dorsal interossei this finger is able to separate from its own axis to the ulnar and the radial sides. The separation of the little finger is achieved primarily by the abductor digiti minimi and the separation of the thumb primarily by the abductor pollicis brevis. Are the bellies of the dorsal interossei identifiable on examination? The answer is a timid yes for the interossei of the long and anular fingers (you can feel them hardening during abduction with a finger appropriately placed on the dorsum of the hand) and a rotund yes for the index dorsal interosseus. This muscle is eminently placed, as well as distinctly developed in normal subjects, as to allow its clinical identification and functional characterization far beyond dissection.29 An experiment can be made “in vivo” by looking at the radial side of the 2nd MCP joint which is free of an overlapping finger. With the tip of a ballpen is possible to identify a point that remains still during flexion-extension movements. This is the transverse axis of the MCP joint. Now let's abduct the index. This motion brings up a strong muscle belly in the web space, which is no other than the dorsal interosseus muscle. If the free edge of this muscle is followed toward the index a tiny tendon appears to attach to the proximal phalanx (in most cases the attachment is to both bone and the dorsal lamina) about 1cm palmar to the axis point which explains its flexor action on the MCP joint. Furthermore, through the dorsal lamina the same contraction extend the interphalangeal joints. Variations are common in the dorsal interossei.30 All dorsal interossei are innervated by the ulnar nerve.
The left panel depicts the palmar interosseus muscles. These are three and given their disposition they bring the index, the anular and the little finger toward the 3rd finger which is the axis of the hand. The dorsal interosseus muscles are shown in the right panel. The middle finger has two and the anular and the index fingers have one. Their disposition is such that they separate the fingers from the 3rd finger, and move the 3rd finger to one and the other side. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.20, with permission.
There are 3 palmar interosseous muscles (Fig. 7), one for the index, one for the anular and 1 for the little finger.28 These muscles, similar to the dorsal counterparts, insert near the corner of the dorsal lamina, on the opposite side. With their origins and insertions facing the long finger it is easy to appreciate that they function as adductors, i.e. they bring the fingers close together. Their actions on the transverse axis of the joints are the same as in the dorsal interossei, flexion of the MCP joint and extension of the PIP and DIP joints. The palmar interossei cannot be reliably identified by palpation. Anatomical variations in these muscles are common.27 All palmar interossei are innervated by the ulnar nerve. Before leaving the interosseous muscles let's make one more experiment. Please note that adduction and abduction of the fingers have been tested in extension. How about with the MCP joints flexed 90 degrees? These motions are not possible. Is this due to the characteristics of insertion of the interosseal muscles? The answer is not, as passive motion is also canceled. The reason for the inability to abduct and adduct the fingers is the eccentric nature of the collateral ligaments of the MCP joints. They are lax in extension and taut in flexion. In rheumatoid arthritis, where damage to the MCP collateral ligaments may occur, lateral finger motion at 90 degrees of MCP flexion is a reliable indicator of this lesion.
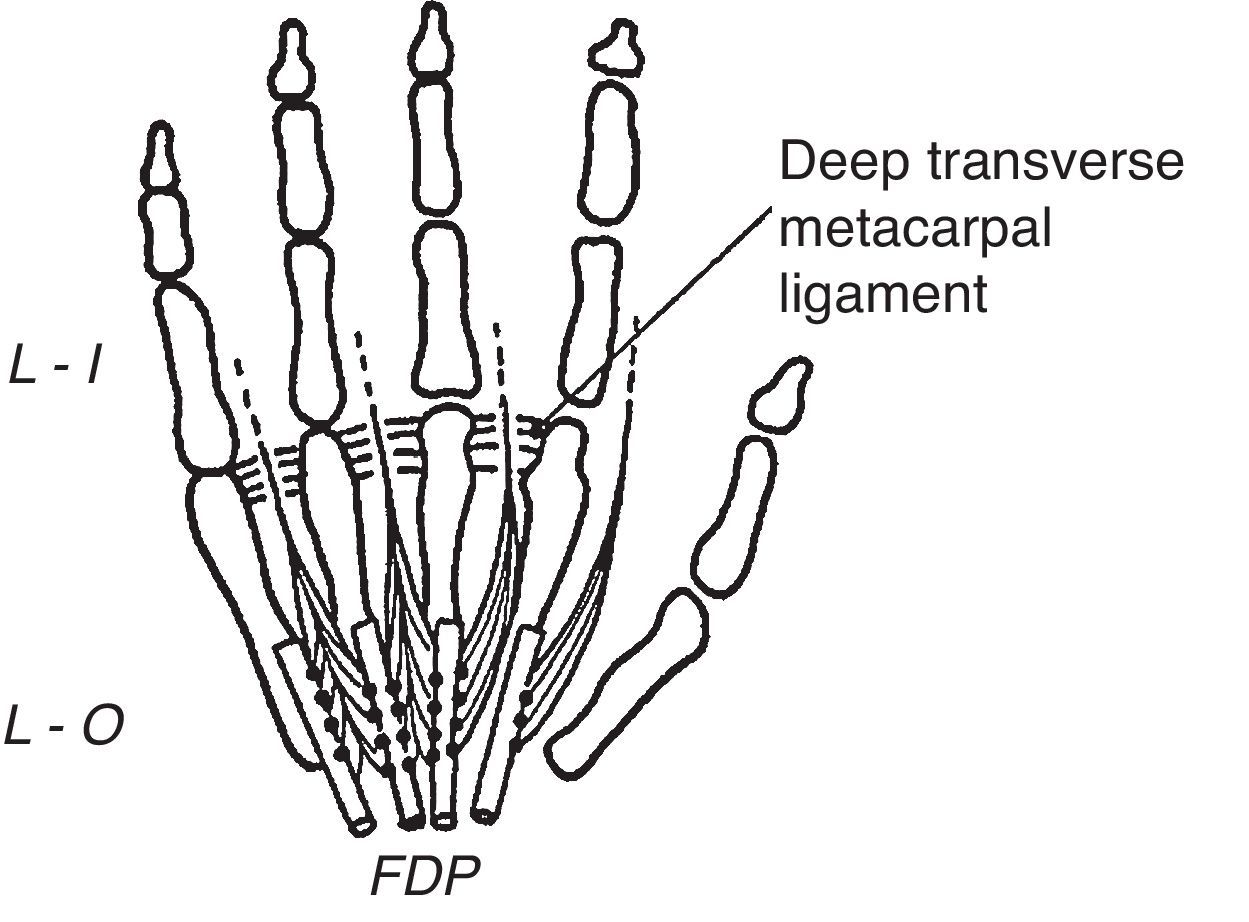
The Lumbrical MusclesThese unique muscles that really look like earthworms have their origin in the deep flexor tendons in the palm of the hand (Fig. 8).30,31 In their way to the extensor lamina they run palmar to the deep metacarpal ligament.32 A unique characteristic of the lumbrical muscles is that, having had an origin in a flexor muscle their insertion is in the extensor lamina and therefore their main action is to flex the MCP joints while extending the PIP and DIP joints. This flexor/extensor linkage, an abundance of mechanoreceptors, plus a common innervation with the flexor digitorum profundus (index and middle finger, median nerve; ring and small finger, ulnar nerve) is telling us something in a language we still do not understand. Variations in the lumbrical muscles are frequent.39 One such variation that may cause a carpal tunnel syndrome is an origin within the carpal tunnel. An origin in the forearm has also been described.
The lumbrical muscles are shown. They are palmar, while the dorsal and the palmar interossei are dorsal, to the transverse metacarpal ligament. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.20, with permission.
Patient 5. De Quervain's tenosynovitis. “A 79-year old violist presents with severe pain in the radial side of his wrist. He is due to play in a concert in 2 days. On physical examination there is a bulky trapeziometacarpal osteoarthritis. He has a markedly positive Finkelstein test. What am I supposed to do? This patient exemplifies a common clinical situation. When there are concurrent conditions, which one is causing the pain? One of his conditions is known to be rather refractory to treatment, the osteoarthritis. The other, de Quervain's tenosynovitis, is eminently treatable by a steroid infiltration. This dilemma was presented to the patient and he had no doubts about the correct course of action which was to have the 1st dorsal compartment tenosynovial sheath injected. The infiltration was successful and he was able to play at his concert”.
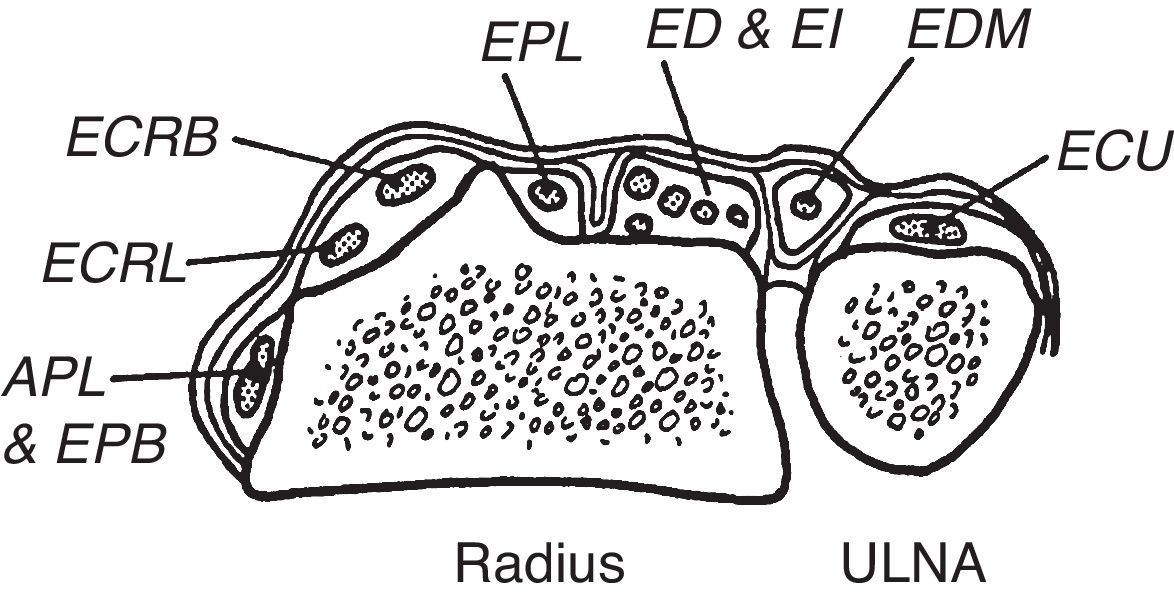
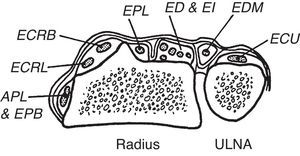
Continuing with our cord experiments, if we place a cord at the distal wrist crease, on the palmar side the cord indicates the proximal limit of the transverse palmar ligament and on the dorsum, the distal limit of the extensor retinaculum (Fig. 9). Thus, the extensor retinaculum is a forearm extensor tendon restraint and the transverse carpal ligament is a wrist flexor tendon restraint. This concept is critical to an understanding of the contents of the radial-most tendon compartments:first dorsal compartment, abductor pollicis longus (APL) and extensor pollicis brevis (EPB); second compartment, extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB); and third compartment, extensor pollicis longus (EPL). Moving distally, at the wrist the first compartment tendons remain the same, but they are followed by EPL and then ECRL and ECRB. The reason for this transposition is an oblique course of EPL at the wrist. Going back to the extensor retinaculum, EPL is flanked radially by a bony eminence, the dorsal tubercle of radius or Lister's tubercle, that redirects its course. The fourth compartment contains extensor indicis (EI) and extendor digitorum (ED). The fifth compartment, which is easy to locate between the distal end of ulna and the radius contains extensor digiti minimi (EDM) and the sixth and compartment, extensor carpi ulnaris. At the first compartment both APL and EPB may have multiple slips In addition, a septum and a bone ridge may be present in 30%–40% between the APL and the EPB tendons.33
The dorsal fibrous tunnels are shown. An important landmark is the dorsal tubercle of radius (Lister's tubercle) which lies radial to extensor pollicis longus (EPL). This is a frequent site of tendon rupture in rheumatoid arthritis. From A Companion to Medical Studies, Volume 1, Ed. by Passmore R and Robson JS, 2nd Edition, Oxford, Wiley/Blackwell 1976, p. 23.22, with permission.
A unique pain syndrome may occur after heavy labor, the intersection syndrome of the forearm.34,35 Pain, tenderness and swelling occur dorso-radially in the forearm about 4 FB proximal to Lister's tubercle. A diagnostic sign is a tendon friction rub brought about by thumb abduction and flexion-extension movements of the wrist. A simple maneuver reveals the anatomy of this condition. Place 4 fingers on the wrist and distal forearm, the little finger next to the base of the 2nd and 3rd metacarpals, the anular over Lister's tubercle, and the long finger and the index proximal to the latter. Now ask the patient to gently dorsiflex the wrist. The tension of the ECRL and ECRB will be felt with the little finger and less with the other fingers. Let's now ask the patient to abduct the thumb. The APL and EPB will be tense up and this will be felt by the index but not by the other digits. Indeed, if one runs the index proximally over the radius these muscles will be felt to run obliquely over a generally longitudinal background. To summarize, APL and EPB cross superficially over ECRL and ECRL A rheumatologist with an interest in clinical anatomy should be able to make an instant diagnosis of intersection syndrome. Someone less informed may require an MRI or an ultrasonography study.
Practical Review of Some Dorsal Structures- •
Palpation of the extensor lamina
- •
Palpation of dorsal interossei
- •
Action of dorsal interossei
- •
Action of palmar interossei
- •
Why interossei flex the MCP (review of the insertion of the 1st dorsal interosseus muscle)
- •
Lumbricals action
- •
Palpatory recognition of trapezium, scaphoid, head of capitate, radial styloid, distal radius, Lister's tubercle (dorsal radial tubercle), distal ulna, ulnar styloid
- •
Visual and palpatory recognition of tendons at the dorsal wrist. From radial to ulnar:abductor pollicis longus (APL), extensor pollicis brevis (APB), extensor pollicis longus (EPL), extensor carpi radialis longus (ECRL), extensor carpi radialis brevis (ECRB), extensor indicis (EI), extensor digitorum (ED), extensor digiti minimi (EDM), and extensor carpi ulnaris (ECU)
- •
Anatomical snuffbox (APL, EPB, radial styloid, radius, Lister's tubercle, scaphoid, trapezium, radial artery, EPL)
- •
Distal boundary of extensor retinaculum
- •
Intersection site, recognition by palpation of APL and EPB, ECRL and ECRB
- •
Finkelstein's maneuver
Patient 6. Carpal tunnel syndrome. “A 46 year-old woman with rheumatoid arthritis. She has tingling in her hands, decreased pin prick sensation in her thumb and index and early atrophy of abductor pollicis brevis”
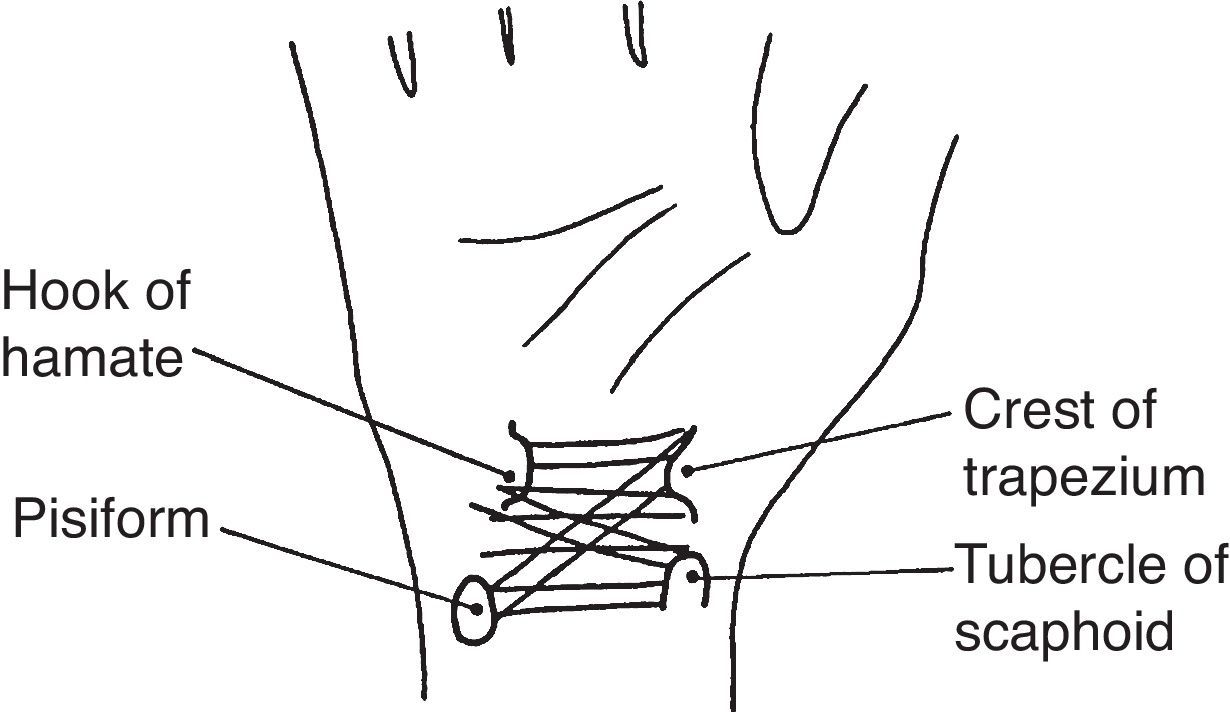
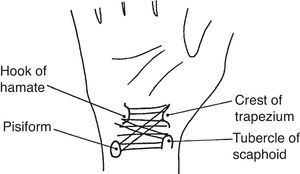
Transverse carpal ligament. This ligament, also known as flexor retinaculum, binds anteriorly the carpal tunnel (Figs. 4 and 10). Its main insertions, on the radial side, are the tubercle of scaphoid and the crest of the trapezium.36 The ulnar side insertions include the pisiform and the hook of hamate. The latter lies deep and can be distinguished only in thin people with supple hands. As mentioned, a string placed at the distal anterior wrist crease indicates the proximal border of the transverse carpal ligament. Nine tendons are contained within the carpal tunnel: four flexor digitorum superficialis tendons, four flexor digitorum profundus tendons and flexor pollicis longus tendon.37 Within the tunnel the 3 synovial tongues that make up the ulnar bursa separate the anterior carpal ligament from the superficial flexor tendons, the superficial from the deep flexor tendons, and the deep flexor tendons from the carpal ligaments and bones. On the radial side the synovial sheath of flexor pollicis longus, known as radial bursa, partially surrounds this tendon on its radial, anterior and posterior sides. The median nerve was left to last because it lies superficially in the boundary between the radial and the ulnar bursae. The subsynovial tissue, as in other connective tissues that glide upon each other, has a complex microstructural arrangement.38 In addition, it may act as a barrier to diffusion.39 The flexor tendons and the median nerve cannot be palpated while in the carpal tunnel. Tissues are just too tightly packed, the anterior carpal ligament is thick and the inserting thenar and hypothenas muscles almost reach each other anterior to the ligament. The distal edge of the transverse carpal ligament cannot be felt as it blends imperceptively with the palmar fascia.
Guyon's canal. Guyon's canal is placed anteriorly in the ulnar third of the wrist. This canal has a proximal opening for the ulnar nerve and artery and 2 distal openings, one for the deep (motor) branch of the ulnar nerve and its artery and another for the superficial (sensory) branch of the ulnar nerve and its artery. Gross and Gelberman have recognized 3 distinct zones in this region, zone 1 in which the nerve is still undivided, zone 2 that refers to the opening for the motor branch, and zone 3 that relates to the superficial branch.40 The roof of Guyon's canal includes the palmar carpal ligament in zone 1, palmaris brevis muscle in zone 2 and fat and fibrous tissue in zone 3. An important point in surface innervation is that the radial half of the palm is supplied by the palmar cutaneous branch of the median nerve and its ulnar half, by the palmar cutaneous branch of the ulnar nerve. Both of these branches arise from the corresponding nerves in the distal forearm and being anterior to the transverse ligamentous structures they are not compressed in the carpal tunnel syndrome and the Guyon's canal syndrome.41
Tendon boundaries of the median nerve at the distal forearm. As mentioned, the median nerve runs deep into, and in between, palmaris longus and flexor carpi radialis. The ulnar bursa, covering the flexor tendons, extends 2–2.5cm proximal to the transverse carpal ligament. This synovial extension allows the injection of the largest synovial structure within the carpal tunnel proximal to the tight limits of the tunnel. The radial bursa, which underlies flexor carpi radialis, is a much smaller than the ulnar bursa. It makes sense to inject the larger rather than the smaller synovial structure hoping that volume reduction after the corticosteroid injection would be greater. We use a needle entry medial to palmaris longus, 1.5–2cm proximal to the distal flexor crease, with a distal angulation of 45 degrees (Fig. 11). Free flow of the local anesthetic without creating a collection indicates a correct placement. Of course, the median nerve and an important branch, the anterior interosseal nerve, as well as the ulnar nerve counterparts, may be compressed more proximally in the forearm.41,42
Practical Review of the Carpal Tunnel and Related Anatomical Structures- •
Thumb movements in the functional position of the hand
- •
Thenar eminence muscles
- •
Median nerve
- •
Hypothenar eminence
- •
Palmar cutaneous muscle, why is it there and how to demonstrate it
- •
Guyon's canal
- •
Transverse carpal ligament and its insertions
- •
Flexor carpi radialis longus
- •
Palmaris muscle
- •
Flexor carpi radialis
- •
Ulnar bursa (in the palm, the carpal tunnel and the distal forearm)
- •
Tinel's and Phalen's maneuvers
The authors have no conflict of interest to declare.